Chinese Medical Sciences Journal ›› 2019, Vol. 34 ›› Issue (4): 256-262.doi: 10.24920/003541
全身麻醉下剖宫产术的单中心回顾性队列研究
- 1. 中国医学科学院北京协和医院麻醉科,北京,100730中国
2. 复旦大学附属肿瘤医院麻醉科,上海,200032中国
3. 中国医学科院肿瘤医院麻醉科,北京,100021中国
A Single-center Retrospective Cohort Study on Cesarean Section under General Anesthesia
Li Xu1,#,Wu Biye1,2,#,Zhang Mingzhu1,3,Shen Le1,*( )
)
- 1. Department of Anesthesiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
2. Department of Anesthesiology, Fudan University Shanghai Cancer Center, Shanghai 200032, China
3. Department of Anesthesiology, Cancer Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100021, China
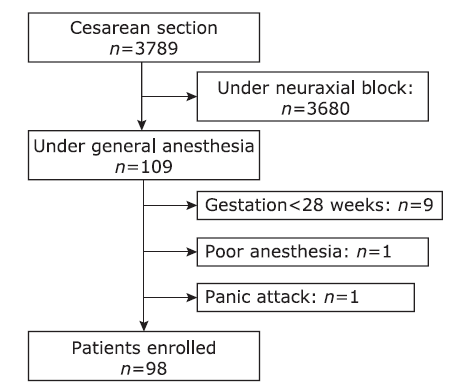
摘要: 目的 椎管内阻滞是剖宫产术最常用的麻醉方法,而在某些情况下全身麻醉在剖宫产术中发挥重要作用。本研究旨在分析选择全身麻醉进行剖宫产的原因以及可能影响母婴结局的因素。方法 回顾性搜集北京协和医院在2014年1月1日至2016年12月31日期间进行全身麻酔的剖宫产产妇和新生儿的临床资料(产妇基本情况,术前状态,围术期情况以及母婴预后)。搜集并分析选择全身麻醉的主要原因,分析产妇返回ICU继续监护与ASA 分级(Ⅲ-Ⅳ vs.Ⅰ-Ⅱ)、孕周(<37周vs. ≥37周)、术中失血量(<800 ml vs. ≥800 ml)的相关性,并比较不同ASA分级和孕周的产妇其胎儿的1分钟Apgar评分情况的差异。 结果 本研究共纳入98例全麻剖宫产术的产妇。在母婴的多种因素中,妊娠合并内科或外科疾病是选择全身麻醉的主要原因(59例,60.2%),其次是妊娠合并胎盘和胎膜异常(38例,38.8%)和妊娠特异性疾病(36例,36.7%)。ASA分级Ⅲ-Ⅳ(χ 2=44.3,P<0.05),孕周<37周(χ 2=23.4,P<0.05),出血量>800 ml的产妇(χ 2=5.5,P<0.05),其术后返ICU的比率较高。产妇住院时间在ASA分级Ⅲ-Ⅳ(t=-2.99,P<0.05)及孕周<37周(t=2.47,P<0.05)的产妇中明显更长。 新生儿1分钟Apgar评分在ASA分级Ⅲ-Ⅳ(t=2.21,P<0.05)以及孕周<37周(t=-3.21,P<0.05)的产妇明显较低。 结论 妊娠合并内科和外科疾病是剖宫产手术选择全身麻醉的最常见原因。ASA分级高,孕周短于37周的产妇术后需要ICU照护的比率较高,住院时间更长,新生儿1分钟Apgar评分较低。