Chinese Medical Sciences Journal ›› 2018, Vol. 33 ›› Issue (2): 91-99.doi: 10.24920/11809
特发性膜性肾病患者血栓栓塞事件发病率及危险因素的队列研究
邹佩美1,李航1,蔡建芳1,陈振杰1,李超1,徐平2,李明喜1,陈丽萌1,李雪梅1( ),李学旺1,*
),李学旺1,*
- 1 中国医学科学院 北京协和医学院,北京协和医院 肾内科,北京 100730 中国
2 中国医学科学院 北京协和医学院,北京 100730 中国
-
收稿日期:2017-10-20出版日期:2018-06-30发布日期:2018-05-07 -
通讯作者:李学旺 E-mail:xuewanglee@126.com
A Cohort Study of Incidences and Risk Factors for Thromboembolic Events in Patients with Idiopathic Membranous Nephropathy
Zou Peimei1,Li Hang1,Cai Jianfang1,Chen Zhenjie1,Li Chao1,Xu Ping2,Li Mingxi1,Chen Limeng1,Li Xuemei1( ),Li Xuewang1,*
),Li Xuewang1,*
- 1 Department of Nephrology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China;
2 Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China;
-
Received:2017-10-20Published:2018-06-30Online:2018-05-07 -
Contact:Li Xuewang E-mail:xuewanglee@126.com
摘要:
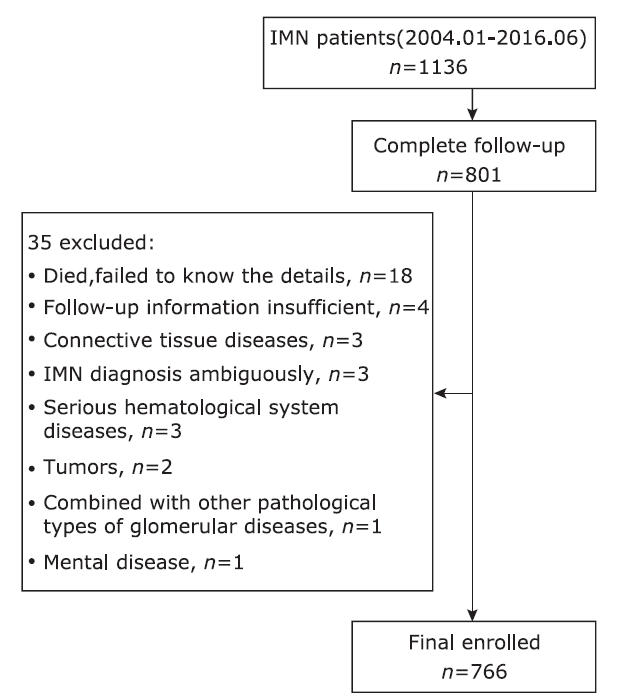
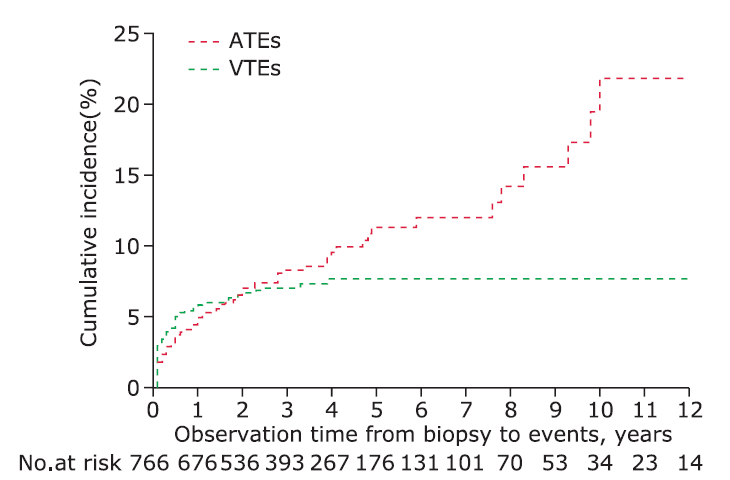
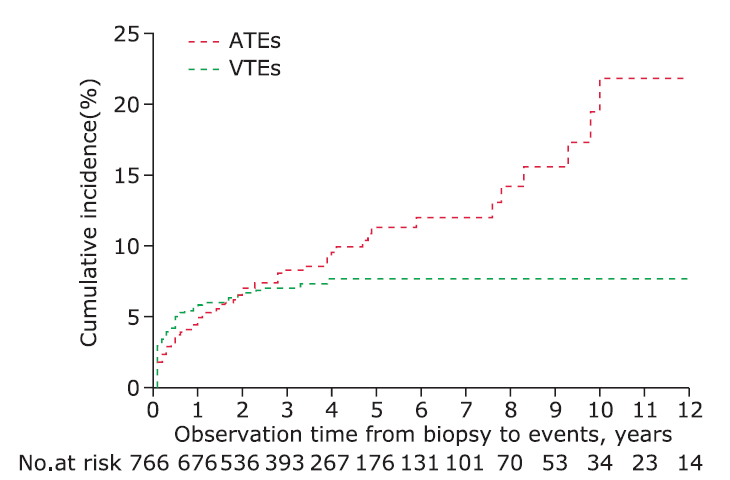
目的 评估特发性膜性肾病(IMN)患者队列中动脉血栓栓塞事件(ATEs)和静脉血栓栓塞事件(VTEs)的发生率及其特点,并探索其相关危险因素。方法 回顾性研究队列共纳入766名连续中国人IMN患者,以Kaplan-Meier模型统计新发的ATEs和VTEs的累积发病率,以单因素和多因素风险回归分析其可能的危险因素。结果 在肾活检诊断为IMN后的第0.5、1、2、3、5年中,ATEs的累积发病率分别为4.3%、5.7%、6.3%、7.1%和8.0%,VTEs的累积发病率分别为5.9%、6.8%、6.9%、7.0%和7.2%。在78起ATE事件(71例)中,心血管疾病、血栓性缺血性脑卒中和外周动脉性疾病分别占比50%、45%和5%;在60起VTE事件(53例)中,深静脉血栓、肾静脉血栓和肺栓塞分别占比60%、13%和27%。ATE和VTE事件发生时,分别有42.1%和81.5%的患者处于肾病综合征(NS)状态(χ 2=18.1,P < 0.001)。ATEs与大量蛋白尿、年龄、吸烟史、高血压和既往ATE史相关,其中年龄是ATEs的独立危险因素(P=0.001),低白蛋白血症为VTEs主要独立危险因素(P=0.03)。 结论 IMN患者ATEs和VTEs发病率高,尤其在病程的前6个月内。ATEs中IS占比高。大量蛋白尿和动脉粥样硬化经典危险因素与ATEs的发生相关,低白蛋白血症为VTEs的独立预测因素。肾病综合征状态时ATEs和VTEs的发生风险增高,特别是VTEs。
引用本文
Zou Peimei, Li Hang, Cai Jianfang, Chen Zhenjie, Li Chao, Xu Ping, Li Mingxi, Chen Limeng, Li Xuemei, Li Xuewang. A Cohort Study of Incidences and Risk Factors for Thromboembolic Events in Patients with Idiopathic Membranous Nephropathy[J].Chinese Medical Sciences Journal, 2018, 33(2): 91-99.
Table 1
Comparison of baseline characteristics between ATE and VTE patients§"
| ATEs (n=71) | VTEs (n=53) | Pvalue | |
|---|---|---|---|
| Sex, n (%) | 0.84 | ||
| Male | 44(62.0) | 34(64.2) | |
| Female | 27(38.0) | 19(35.8) | |
| Age, year | 57.0±11.9 | 49.6±14.8 | 0.003 |
| History of | |||
| Smoking, n(%) | 31 (43.7) | 15 (28.3) | 0.08 |
| Hypertension, n (%) | 46 (64.8) | 26 (49.1) | 0.08 |
| Diabetes, n(%) | 16 (22.5) | 14 (26.4) | 0.62 |
| Prior ATE, n(%) | 4 (5.6) | 2 (3.8) | 0.63 |
| Observation time, month | 43.2 (5.4, 145.1) | 43.6 (21.5, 62.0) | 0.41 |
| Proteinuria, g/24 h | 6.38 (3.79, 10.16) | 7.30 (4.88, 10.54) | 0.15 |
| Serum albumin, g/L | 26.7±6.3 | 25.8±6.6 | 0.45 |
| eGFR, ml/min/1.73 m2 | 88.65±22.27 | 97.22±18.86 | 0.03 |
| Total cholesterol, mmol/L | 7.98±2.42 | 8.87±2.84 | 0.11 |
| Triglycerides, mmol/L | 2.43 (1.81, 3.60) | 3.32 (1.96, 4.71) | 0.10 |
| LDL-C, mmol/L | 5.41±2.19 | 5.63±2.48 | 0.68 |
| NS, n (%) | 49 (69.0) | 38 (71.7) | 0.75 |
Table 2
Comparison of the clinical characteristics at the time of events between ATEs and VTEs§"
| Characteristics | ATEs (n=58) | VTEs (n=56) | P value? | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean/ Median | Early onset (n=27) | Delayed onset (n=31) | P value* | Mean/ Median | Early onset (n=48) | Delayed onset (n=8) | P value* | |||
| Age, year | 59.0±11.4 | 59.4±11.8 | 58.7±11.2 | 0.81 | 50.0±15.4 | 49.0±16.0 | 56.4±9.5 | 0.21 | 0.001 | |
| Proteinuria, g/24 h | 3.5(1.05, 7.12) | 4.5(2.0, 6.7) | 2.8(0.7, 7.8) | 0.33 | 6.2(4.5, 9.6) | 6.2(4.5, 9.8) | 6.7(4.4, 9.2) | 0.76 | 0.002 | |
| Serum albumin, g/L | 29.8±8.0 | 26.8±7.6 | 32.4±7.5 | 0.01 | 25.1±7.7 | 25.1±8.1 | 25.1±5.8 | 1.00 | 0.002 | |
| eGFR, ml/min/ 1.73m2 | 84.2±22.1 | 87.5±20.8 | 81.6±23.1 | 0.35 | 94.8±22.3 | 96.6±21.4 | 84.0±26.3 | 0.14 | 0.02 | |
| Total cholesterol, mmol/L | 7.4(5.1, 8.9) | 7.8(6.5, 8.9) | 6.1(4.9, 9.3) | 0.11 | 8.0(6.3, 9.3) | 8.4±2.7 | 7.9±1.4 | 0.66 | 0.21 | |
| Triglycerides, mmol/L | 2.1(1.7, 3.0) | 2.1(1.7, 4.3) | 2.6(1.1, 2.9) | 0.75 | 3.4(1.9, 4.4) | 3.4(2.0, 4.0) | 1.9(1.6, 4.8) | 0.63 | 0.04 | |
| LDL-C, mmol/L | 4.3(2.7, 6.5) | 5.5(2.7, 6.7) | 3.8(2.6, 6.4) | 0.27 | 4.5(3.4, 7.0) | 4.5(3.3, 7.2) | 4.51(3.45, -) | 0.87 | 0.54 | |
| NS, n (%) | < 0.001 | |||||||||
| NS status | 24 (42.1) | 16 (59.3) | 8 (26.7) | 0.01 | 44 (81.5) | 38 (79.2) | 6 (75.0) | N/A | ||
| Sub-NS | 22 (38.6) | 10 (37.0) | 12 (38.7) | 8 (14.8) | 8 (16.7) | 0 (0.0) | ||||
| CR | 11 (19.3) | 1 (3.7) | 10 (35.5) | 2 (3.7) | 2 (4.2) | 0 (0.0) | ||||
Table 3
Univariable model proportional-hazards analysis on association of clinical characteristics with VTE and ATE"
| Variables | n | ATE | VTE | |||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | Pvalue | HR | 95% CI | P value | |||
| Sex, male | 449 | 1.2 | 0.8-2.0 | 0.39 | 1.6 | 0.8-2.4 | 0.29 | |
| Age, years | 766 | < 0.001 | 0.35 | |||||
| <35 | 167 | 1.0 | reference | 1.0 | reference | |||
| 35-54 | 323 | 5.1 | 1.2-21.7 | 0.8 | 0.4-1.7 | |||
| ≥55 | 276 | 13.0 | 3.1-53.3 | 1.3 | 0.6-2.6 | |||
| History of | 766 | |||||||
| Smoking | 228 | 1.7 | 1.0-2.7 | 0.03 | 0.9 | 0.5-1.7 | 0.81 | |
| Hypertension | 360 | 1.8 | 1.1-3.0 | 0.02 | 0.9 | 0.5-1.6 | 0.77 | |
| Diabetes | 90 | 1.5 | 0.8-2.8 | 0.24 | 1.3 | 0.6-2.9 | 0.44 | |
| ATE | 35 | 2.4 | 1.1-5.2 | 0.03 | 0.8 | 0.2-3.4 | 0.79 | |
| Proteinuria, g/24 h | 712 | 0.04 | 0.03 | |||||
| <3.5 | 191 | 1.0 | reference | 1.0 | reference | |||
| 3.5-8.0 | 313 | 1.3 | 0.7-2.7 | 3.6 | 1.3-10.5 | |||
| >8.0 | 208 | 2.2 | 1.1-4.4 | 4.3 | 1.5-12.8 | |||
| Serum albumin, g/L | 710 | 0.64 | 0.01 | |||||
| <20 | 73 | 1.6 | 0.6-4.4 | 5.5 | 1.5-19.9 | |||
| 20-35 | 198 | 1.4 | 0.6-3.0 | 2.3 | 0.7-7.6 | |||
| ≥35 | 246 | 1.0 | reference | 1.0 | reference | |||
| eGFR, ml/min/1.73 m2 | 760 | 0.10 | 0.27 | |||||
| ≥90 | 517 | 1.0 | reference | 1.0 | reference | |||
| 60-89 | 195 | 1.4 | 0.8-2.4 | 1.4 | 0.8-2.5 | |||
| <60 | 48 | 2.2 | 1.0-4.8 | 0.3 | 0.1-2.4 | |||
| Total cholesterol, mmol/L | 543 | 0.97 | 0.14 | |||||
| <5.18 | 43 | 1.0 | reference | 1.0 | reference | |||
| 5.18-7.76 | 240 | 0.9 | 0.3-2.4 | 2.4 | 0.3-18.3 | |||
| >7.76 | 260 | 0.9 | 0.3-2.3 | 4.1 | 0.6-30.5 | |||
Table 4
Multivariable model proportional-hazards analysis on risk factors of VTE and ATE"
| ATE | VTE | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | Pvalue | Variables | HR | 95% CI | Pvalue | |
| History of | Serum albumin, g/L | 0.03 | ||||||
| Smoker | 1.4 | 0.8-2.4 | 0.19 | <20 | 3.2 | 0.8-12.5 | ||
| ATE | 1.6 | 0.7-3.5 | 0.28 | 20-35 | 1.3 | 0.4-4.5 | ||
| Hypertension | 1.1 | 0.6-1.8 | 0.84 | ≥35 | 1.0 | reference | ||
| Age, years | 0.001 | |||||||
| <35 | 1.0 | reference | ||||||
| 35-54 | 4.4 | 1.0-19.1 | ||||||
| ≥55 | 9.2 | 2.2-39.5 | ||||||
| Proteinuria, g/24 h | 0.11 | Proteinuria, g/24 h | 0.13 | |||||
| <3.5 | 1.0 | reference | <3.5 | 1.0 | reference | |||
| 3.5-8.0 | 1.1 | 0.6-2.3 | 3.5-8.0 | 3.0 | 1.0-8.9 | |||
| >8.0 | 1.9 | 0.9-3.8 | >8.0 | 3.2 | 1.0-10.1 | |||
| 1. |
Cattran D . Management of membranous nephropathy: when and what for treatment. J Am Soc Nephrol 2005; 16(5):1188-94. doi: 10.1681/ASN.2005010028.
doi: 10.1681/ASN.2005010028 pmid: 15800117 |
| 2. |
Pan X, Xu J, Ren H , et al. Changing spectrum of biopsy-proven primary glomerular diseases over the past 15 years: a single-center study in China. Contrib Nephrol 2013; 181:22-30. doi: 10.1159/000348638.
doi: 10.1159/000348638 |
| 3. |
Barbour SJ, Greenwald A, Djurdjev O , et al. Disease-specific risk of venous thromboembolic events is increased in idiopathic glomerulonephritis. Kidney Int 2012; 81(2):190-5. doi: 10.1038/ki.2011.312.
doi: 10.1038/ki.2011.312 pmid: 21918501 |
| 4. |
Glassock RJ . Prophylactic anticoagulation in nephrotic syndrome: a clinical conundrum. J Am Soc Nephrol 2007; 18(8):2221-5. doi: 10.1681/ASN.2006111300.
doi: 10.1681/ASN.2006111300 pmid: 17599972 |
| 5. |
Kayali F, Najjar R, Aswad F , et al. Venous thromboembolism in patients hospitalized with nephrotic syndrome. Am J Med 2008; 121(3):226-30. doi: 10.1016/j.amjmed.2007.08.042.
doi: 10.1016/j.amjmed.2007.08.042 pmid: 18328307 |
| 6. |
Gilboa N . Letter: Incidence of coronary heart disease associated with nephrotic syndrome. Med J Aust 1976; 1(7):207-8.
pmid: 1272153 |
| 7. |
Ordo?ez JD, Hiatt RA, Killebrew EJ , et al. The increased risk of coronary heart disease associated with nephrotic syndrome. Kidney Int 1993; 44(3):638-42. doi: 10.1038/ki.1993.292.
doi: 10.1038/ki.1993.292 pmid: 8231039 |
| 8. |
Wass VJ, Jarrett RJ, Chilvers C , et al. Does the nephrotic syndrome increase the risk of cardiovascular disease? Lancet 1979; 2(8144):664-7. doi: 10.1016/s0140-6736(79)92067-1.
doi: 10.1016/s0140-6736(79)92067-1 pmid: 90759 |
| 9. |
Mahmoodi BK, ten Kate MK, Waanders F , et al. High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study. Circulation 2008; 117(2):224-30. doi: 10.1161/CIRCULATIONAHA.107.716951.
doi: 10.1161/CIRCULATIONAHA.107.716951 pmid: 18158362 |
| 10. |
Lee T, Derebail VK, Kshirsagar AV , et al. Patients with primary membranous nephropathy are at high risk of cardiovascular events. Kidney Int 2016; 89(5):1111-8. doi: 10.1016/j.kint.2015.12.041.
doi: 10.1016/j.kint.2015.12.041 pmid: 26924046 |
| 11. |
Levey AS, Stevens LA, Schmid CH , et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150(9):604-12.
doi: 10.7326/0003-4819-150-9-200905050-00006 pmid: 2763564 |
| 12. |
Troyanov S, Wall CA, Scholey J W , et al. Idiopathic membranous nephropathy: definition and relevance of a partial remission. Kidney Int 2004; 66(3):1199-205. doi: 10.1111/j.1523-1755.2004.00873.x
doi: 10.1111/j.1523-1755.2004.00873.x pmid: 15327418 |
| 13. |
Radhakrishnan J, Appel AS, Valeri A , et al. The nephrotic syndrome, lipids, and risk factors for cardiovascular disease. Am J Kidney Dis 1993; 22(1):135-42. doi: 10.1016/s0272-6386(12)70179-8.
doi: 10.1016/s0272-6386(12)70179-8 pmid: 8322776 |
| 14. |
Vaziri ND . Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences. Kidney Int 2016; 90(1):41-52. doi: 10.1016/j.kint.2016.02.026.
doi: 10.1016/j.kint.2016.02.026 pmid: 27165836 |
| 15. |
Nandwani A, Pathania D, Jha PK , et al. Renal artery thrombosis with renal infarction: a rare cause of acute abdomen. Indian J Nephrol 2017; 27(4):313-5. doi: 10.4103/0971-4065.183581.
doi: 10.4103/0971-4065.183581 pmid: 5514829 |
| 16. |
Parag KB, Somers SR, Seedat YK , et al. Arterial thrombosis in nephrotic syndrome. Am J Kidney Dis 1990; 15(2):176-7. doi: 10.1016/s0272-6386(12) 80516-6.
doi: 10.1016/s0272-6386(12) 80516-6 pmid: 609917 |
| 17. |
Sasaki Y, Raita Y, Uehara G , et al. Carotid thromboembolism associated with nephrotic syndrome treated with dabigatran. Case Rep Nephrol Urol 2014; 4(1):42-52. doi: 10.1159/000362162.
doi: 10.1159/000362162 pmid: 24803917 |
| 18. |
Singhal R, Brimble KS . Thromboembolic complications in the nephrotic syndrome: pathophysiology and clinical management. Thromb Res 2006; 118(3):397-407. doi: 10.1016/j.thromres.2005.03.030.
doi: 10.1016/j.thromres.2005.03.030 pmid: 15990160 |
| 19. |
Li SJ, Guo JZ, Zuo K , et al. Thromboembolic complications in membranous nephropathy patients with nephrotic syndrome-a prospective study. Thromb Res 2012; 130(3):501-5. doi: 10.1016/j.thromres.2012.04.015.
doi: 10.1016/j.thromres.2012.04.015 pmid: 22633211 |
| 20. |
Lionaki S, Derebail VK, Hogan SL , et al. Venous thromboembolism in patients with membranous nephropathy. Clin J Am Soc Nephrol 2012; 7(1):43-51. doi: 10.2215/CJN.04250511.
doi: 10.2215/CJN.04250511 pmid: 22076873 |
| 21. |
Llach F . Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome. Kidney Int 1985; 28(3):429-39. doi: 10.1038/ki.1985.149.
doi: 10.1038/ki.1985.149 pmid: 3906225 |
| 22. |
Bellomo R, Atkins RC . Membranous nephropathy and thromboembolism: is prophylactic anticoagulation warranted? Nephron 1993; 63(3):249-54. doi: 10.1159/000187205.
doi: 10.1159/000187205 pmid: 8446259 |
| 23. |
Ponticelli C, Glassock RJ . Glomerular diseases: membranous nephropathy-a modern view. Clin J Am Soc Nephrol 2014; 9(3):609-16. doi: 10.2215/CJN.04160413.
doi: 10.2215/CJN.04160413 |
| [1] | 廖中华, 冯俊涛, 唐家乐, 罗丽颖, 李晓照. 1例严重肺及下肢血管栓塞并轻微肾损害的髓过氧化物酶阳性的抗中性粒细胞胞浆抗体相关性血管炎:病例报告[J]. Chinese Medical Sciences Journal, 2021, 36(4): 342-345. |
| [2] | 李慧利, 林陪双, 姚允泰. 海德综合征与主动脉瓣置换术:已发表文献回顾[J]. Chinese Medical Sciences Journal, 2021, 36(4): 307-315. |
| [3] | 王轶, 张竹花, 连伟. 垂体瘤切除术后突发感音神经性聋—病例系列报告及文献复习[J]. Chinese Medical Sciences Journal, 2021, 36(2): 120-126. |
| [4] | 王维嘉, 申乐, 拉巴次仁, 李晗歌, 张越伦, 黄宇光. 西藏地区麻醉医师职业耗竭现状及相关因素分析[J]. Chinese Medical Sciences Journal, 2021, 36(2): 97-102. |
| [5] | 祖红林,侯骊坤,刘洪伟,詹渊博,何菊. 应用BITOLA系统筛选腹主动脉瘤与2型糖尿病相互作用的候选基因[J]. Chinese Medical Sciences Journal, 2021, 36(1): 50-56. |
| [6] | 尹俊雄, 余诚, 魏丽霞, 余传勇, 刘红星, 杜明洋, 孙丰, 王崇骏, 王小姗. 基于机器学习的脑卒中高危人群无症状性颈动脉狭窄的检测研究[J]. Chinese Medical Sciences Journal, 2020, 35(4): 297-305. |
| [7] | 章旭,吉磊,陈梦寅,王威,郑月宏. 腹主动脉瘤腔内隔绝术后经动脉栓塞与经腰栓塞治疗Ⅱ型内漏效果对比的meta分析[J]. Chinese Medical Sciences Journal, 2020, 35(2): 135-141. |
| [8] | 张兴华, 李涛, 杨立, 金鑫, 吴坚, 常瑞萍, 张晶. 主动脉壁内血肿CT血管成像形态学特征与C反应蛋白的相关性研究[J]. Chinese Medical Sciences Journal, 2019, 34(4): 241-247. |
| [9] | 陈强, 张丽伟, 黄党生, 张春红, 王秋霜, 沈东, 熊敏俊, 杨菲菲. 冠状动脉疾病合并糖尿病患者经StentBoost技术指导的经皮冠状动脉介入治疗后5年的随访分析[J]. Chinese Medical Sciences Journal, 2019, 34(3): 177-183. |
| [10] | 黄河, 林颖, 姚荣欣, 何牧卿, 林晓骥. 静脉丙种球蛋白联合血小板输注、利伐沙班治疗肝素诱导的危重血小板减少症1例[J]. Chinese Medical Sciences Journal, 2019, 34(1): 60-64. |
| [11] | 陈伟健, 乔宏宇, 方桂婷, 钟兴. 1例可能由按摩引起的椎动脉夹层[J]. Chinese Medical Sciences Journal, 2019, 34(1): 65-68. |
| [12] | 马瑾, 陈婷, 王一玮, 赵潺, 李东辉, 王萌, 干霖洋, 钟勇. 纵向测量大鼠非动脉炎性前部缺血性视神经病变模型中后部视乳头血流变化的研究[J]. Chinese Medical Sciences Journal, 2018, 33(4): 252-259. |
| [13] | 张雪芳,张震宇,李楠. 一例妊娠早期合并脑静脉窦血栓女性成功中期引产的报道[J]. Chinese Medical Sciences Journal, 2018, 33(4): 267-271. |
| [14] | 张宏民, 王小亭, 张青, 刘大为. 应用“目标与目的”方案进行脓毒症患者的复苏:来自一个中国三级甲等医院ICU的回顾性研究[J]. Chinese Medical Sciences Journal, 2018, 33(3): 135-142. |
| [15] | 李涛, 杨立, 张卫国, 罗春才, 黄自立, 李金锋, 李欣. 6 4层多排CT对冠状动脉旁路移植术后的中期随访:影响桥血管通畅性的危险因素研究[J]. Chinese Medical Sciences Journal, 2018, 33(2): 69-76. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
|