Chinese Medical Sciences Journal ›› 2023, Vol. 38 ›› Issue (1): 11-19.doi: 10.24920/004120
Special Issue: 心脏疾病与健康
• Original Article • Previous Articles Next Articles
Relationship of Microvascular Obstruction with Global and Regional Myocardial Function Determined by Cardiac Magnetic Resonance after ST-Segment Elevation Myocardial Infarction
Ya-Nan Zhao1, Jia-Ning Cui1, Xing-Hua Zhang1, Jin-Feng Li1, Shi-Min Chen2, Xiu-Zheng Yue3, Tao Li1, *( )
)
- 1Department of Radiology, First Medical Center of Chinese People's Liberation Army General Hospital, Beijing 100853, China
2Department of Epidemiology and Statistics, Graduate School of Chinese People's Liberation Army General Hospital, Beijing 100853, China
3Philips Healthcare, Beijing 100600, China
-
Received:2022-06-08Accepted:2022-08-10Published:2023-03-31Online:2022-09-09 -
Contact:Tao Li E-mail:litaofeivip@163.com
Cite this article
Ya-Nan Zhao, Jia-Ning Cui, Xing-Hua Zhang, Jin-Feng Li, Shi-Min Chen, Xiu-Zheng Yue, Tao Li. Relationship of Microvascular Obstruction with Global and Regional Myocardial Function Determined by Cardiac Magnetic Resonance after ST-Segment Elevation Myocardial Infarction[J].Chinese Medical Sciences Journal, 2023, 38(1): 11-19.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

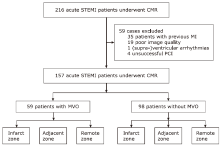
Figure 1.
The division of the infarct, adjacent and remote segments of left ventricle. (A) Definition of the infarct, adjacent and remote zone of myocardium on a representative short-axis late gadolinium enhancement image of a patient with anterior myocardial infarction. (B) Schematic diagram of the infarct, adjacent and remote zones based on a myocardial 16-segment model recommended by the American Heart Association (AHA). If the infarct zone includes the segments 1, 2, 7, 8, 13, 14, 15 and 16, the adjacent zone includes the segments 3, 6, 9, 10, 11 and 12, and the rest of myocardium is defined as the remote zone."
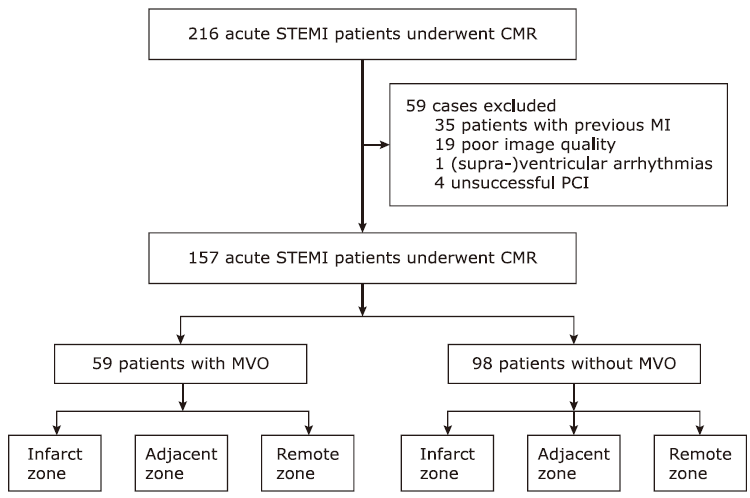
Figure 2.
Schematic diagram of myocardial strain assessment. (A) A typical example of short axis image of inferior myocardial infarction with MVO scanned by LGE imaging (arrows). (B) Representative bull's eye map for radial strain assessment. (C) Representative bull's eye map for circumferential strain assessment. (D) Representative bull's eye map for longitudinal strain assessment. MVO: microvascular obstruction; LGE: late gadolinium enhancement."

Table 1.
Baseline characteristics of the STEMI patients with and without microvascular obstruction (n = 157)"
| Items | All patients (n = 157) | Patient with MVO (n = 59) | Patient without MVO (n = 98) | P value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age (yrs, mean ± SD) | 56.66 ± 11.38 | 54.12 ± 11.63 | 58.18 ± 11.01 | 0.03 |
| Gender [male n (%)] | 136 (86.6) | 53 (89.8) | 83 (84.7) | 0.36 |
| Body mass index [kg/m2, mean ± SD] | 25.68 ± 3.43 | 25.76 ± 3.20 | 25.63 ± 3.57 | 0.49 |
| Clinical parameters | ||||
| Family history of CAD [n (%)] | 15 (9.6) | 5 (8.5) | 10 (10.2) | 0.72 |
| Hypertension [n (%)] | 79 (50.3) | 28 (47.5) | 51 (52.0) | 0.58 |
| Hypercholesterolemia [n (%)] | 33 (21.0) | 17 (28.8) | 16 (16.3) | 0.63 |
| Diabetes mellitus [n (%)] | 23 (14.6) | 11 (18.6) | 12 (12.2) | 0.27 |
| Smoking [n (%)] | 103 (65.6) | 42 (71.2) | 61 (62.2) | 0.25 |
| Drinking [n (%)] | 37 (23.6) | 13 (22.0) | 24 (24.5) | 0.73 |
| Heart rate (beats/min, mean ± SD) | 71.29 ± 11.61 | 73.59 ± 11.97 | 69.91 ± 11.22 | 0.054 |
| Killip class >Ⅰ [n (%)] | 16 (10.2) | 7 (11.9) | 9 (9.2) | 0.59 |
| Multivessel disease [n (%)] | 101 (64.3) | 36 (60.1) | 65 (66.3) | 0.501 |
| Infarct related artery [n (%)] | 0.52 | |||
| Left anterior descending artery | 69 (43.94) | 28 (47.46) | 41 (41.84) | |
| Right coronary artery | 70 (44.59) | 22 (37.29) | 48 (48.98) | |
| Left circumflex artery | 18 (11.46) | 6 (10.17) | 12 (12.24) | |
| TIMI flow pre PCI < 3 [n (%)] | 148 (94.3) | 58 (98.3) | 90 (91.8) | 0.06 |
| TIMI flow post PCI < 3 [n (%)] | 2 (1.3) | 1 (1.7) | 1 (1.0) | 0.72 |
| Blood test results | ||||
| NT-proBNP (pg/mL, mean ± SD) | 1,616.01 ± 1,552.90 | 1,838.72 ± 2,118.44 | 1,481.92 ± 1,070.77 | 0.23 |
| Maximum CK-MB (U/L, mean ± SD) | 233.28 ± 163.89 | 317.34 ± 173.51 | 182.67 ± 135.31 | <0.001 |
| Peak troponin (mg/L, mean ± SD) | 7.85 ± 7.84 | 12.65 ± 9.13 | 4.95 ± 5.15 | <0.001 |
| Medication [n (%)] | ||||
| Aspirin | 156 (99.4) | 58 (98.3) | 98 (100) | 0.16 |
| Statin | 156 (99.4) | 59 (100) | 97 (99.0) | 0.33 |
| ACEI/ARB | 70 (44.6) | 21 (35.6) | 49 (50.0) | 0.08 |
| Beta-blockers | 135 (86.0) | 50 (84.7) | 85 (86.7) | 0.73 |
| Diuretic | 76 (48.4) | 31 (52.5) | 45 (45.9) | 0.42 |
Table 2.
Comparisons of LV global and regional functions between STEMI patients with and without MVO (mean ± SD)"
| Items | All Patients (n = 157) | Patient with MVO (n = 59) | Patient without MVO (n = 98) | t value | P value* |
|---|---|---|---|---|---|
| LV EDVI (mL/m2) | 80.81 ± 18.94 | 83.31 ± 16.07 | 79.30 ± 20.40 | 1.29 | 0.20 |
| LV ESVI (mL/m2) | 43.44 ± 13.40 | 47.39 ± 13.04 | 41.06 ± 13.11 | 2.94 | 0.004 |
| LV myocardial mass index (g/m2) | 59.83 ± 11.61 | 62.24 ± 9.42 | 58.37 ± 12.58 | 2.04 | 0.04 |
| LV infarct size (mL) | 24.96 ± 16.18 | 36.55 ± 16.55 | 17.97 ± 11.23 | 8.37 | <0.001 |
| LVEF (%) | 46.14 ± 9.23 | 43.01 ± 9.45 | 48.02 ± 8.61 | -3.41 | 0.001 |
| LV global WTR (%) | 44.25 ± 13.64 | 40.21 ± 11.62 | 46.68 ± 14.23 | -2.95 | 0.004 |
| LV GRS (%) | 22.70 ± 5.84 | 20.25 ± 4.75 | 24.17 ± 5.96 | -4.30 | <0.001 |
| LV GCS (%) | -14.19 ± 2.80 | -12.85 ± 2.52 | -14.99 ± 2.66 | 4.99 | <0.001 |
| LV GLS (%) | -11.95 ± 3.28 | -10.80 ± 3.39 | -12.64 ± 3.03 | 3.51 | 0.001 |
| Infarct zone RS (%) | 14.46 ± 7.77 | 12.05 ± 5.83 | 15.92 ± 8.42 | -3.38 | 0.001 |
| Infarct zone CS (%) | -9.99 ± 5.49 | -8.53 ± 4.83 | -10.87 ± 5.70 | 2.64 | 0.01 |
| Infarct zone LS (%) | -7.34 ± 4.48 | -7.13 ± 3.65 | -7.47 ± 4.93 | 0.46 | 0.65 |
| Adjacent zone RS (%) | 22.52 ± 7.59 | 22.90 ± 7.07 | 22.29 ± 7.92 | 0.49 | 0.63 |
| Adjacent zone CS (%) | -14.71 ± 3.93 | -14.42 ± 3.48 | -14.89 ± 4.18 | 0.73 | 0.47 |
| Adjacent zone LS (%) | -7.25 ± 4.18 | -6.50 ± 3.46 | -7.69 ± 4.51 | 1.75 | 0.08 |
| Remote zone RS (%) | 30.31 ± 9.85 | 31.94 ± 9.84 | 29.33 ± 9.78 | 1.62 | 0.11 |
| Remote zone CS (%) | -17.30 ± 4.39 | -17.20 ± 3.99 | -17.36 ± 4.63 | 0.22 | 0.83 |
| Remote zone LS (%) | -5.15 ± 9.67 | -3.60 ± 8.98 | -6.09 ± 9.99 | 1.57 | 0.12 |
Table 3.
Univariate and multivariate Logistic regression analysis of the factors associated with impaired LV GCS"
| Items | Univariate Logistic regression | Multivariate Logistic regression | |||
|---|---|---|---|---|---|
| P value | OR [95%CI] | P value | OR [95%CI] | ||
| Age (yrs) | 0.81 | 1.00 (0.97 - 1.03) | |||
| Gender (Male) | 0.06 | 2.65 (0.97 - 7.24) | |||
| Body mass index (kg/m2) | 0.27 | 1.05 (0.96 - 1.16) | |||
| Family history of CAD | 0.15 | 2.30 (0.75 - 7.08) | |||
| Hypertension | 0.23 | 1.47 (0.78 - 2.76) | |||
| Hypercholesterolemia | 0.25 | 0.63 (0.29 - 1.38) | |||
| Diabetes mellitus | 0.70 | 1.19 (0.49 - 2.89) | |||
| Smoking | 0.09 | 1.80 (0.92 - 3.52) | |||
| Drinking | 0.06 | 2.08 (0.98 - 4.42) | |||
| Killip class >Ⅰ | 0.24 | 1.89 (0.65 - 5.49) | |||
| Heart rate | 0.001 | 1.06 (1.02 - 1.09) | 0.001 | 1.08 (1.03 - 1.13) | |
| Culprit lesion in the LAD (%) | <0.001 | 3.25 (1.69 - 6.27) | |||
| NT-proBNP (pg/mL) | 0.01 | 1.00 (1.00 - 1.00) | |||
| Maximum CK-MB (U/L) | <0.001 | 1.01 (1.00 - 1.01) | |||
| Peak troponin (mg/L) | <0.001 | 1.12 (1.06 - 1.20) | |||
| LV EDVI | 0.35 | 1.01 (0.99 - 1.03) | |||
| LV ESVI | <0.001 | 1.08 (1.05 - 1.12) | |||
| LV myocardial mass index (g/m2) | <0.001 | 1.08 (1.04 - 1.12) | |||
| LV infarct size (mL) | <0.001 | 1.11 (1.07 - 1.15) | 0.003 | 1.10 (1.03 - 1.16) | |
| Presence of LV MVO (%) | <0.001 | 4.10 (2.05 - 8.19) | |||
| LV MVO size (mL) | 0.01 | 1.38 (1.10 - 1.72) | |||
| [1] |
Amier RP, Tijssen RYG, Teunissen PFA, et al. Predictors of intramyocardial hemorrhage after reperfused ST-segment elevation myocardial infarction. J Am Heart Assoc 2017; 6(8):e005651. doi: 10.1161/jaha.117.005651.
doi: 10.1161/jaha.117.005651 |
| [2] |
Nijveldt R, Beek AM, Hirsch A, et al. Functional recovery after acute myocardial infarction: comparison between angiography, electrocardiography, and cardiovascular magnetic resonance measures of microvascular injury. J Am Coll Cardiol 2008; 52(3):181-9. doi: 10.1016/j.jacc.2008.04.006.
doi: 10.1016/j.jacc.2008.04.006 pmid: 18617066 |
| [3] |
Schwaiger JP, Reinstadler SJ, Tiller C, et al. Baseline LV ejection fraction by cardiac magnetic resonance and 2D echocardiography after ST-elevation myocardial infarction—influence of infarct location and prognostic impact. Eur Radiol 2020; 30(1):663-71. doi: 10.1007/s00330-019-06316-3.
doi: 10.1007/s00330-019-06316-3 pmid: 31428825 |
| [4] |
Amzulescu MS, De Craene M, Langet H, et al. Myocardial strain imaging: review of general principles, validation, and sources of discrepancies. Eur Heart J Cardiovasc Imaging 2019; 20(6):605-19. doi: 10.1093/ehjci/jez041.
doi: 10.1093/ehjci/jez041 pmid: 30903139 |
| [5] |
Wamil M, Borlotti A, Liu D, et al. Combined T1-mapping and tissue tracking analysis predicts severity of ischemic injury following acute STEMI—an Oxford Acute Myocardial Infarction (OxAMI) study. Int J Cardiovasc Imaging 2019; 35(7):1297-308. doi: 10.1007/s10554-019-01542-8.
doi: 10.1007/s10554-019-01542-8 |
| [6] |
Khan JN, Singh A, Nazir SA, et al. Comparison of cardiovascular magnetic resonance feature tracking and tagging for the assessment of left ventricular systolic strain in acute myocardial infarction. Eur J Radiol 2015; 84(5):840-8. doi: 10.1016/j.ejrad.2015.02.002.
doi: 10.1016/j.ejrad.2015.02.002 pmid: 25743248 |
| [7] |
Everaars H, Robbers L, Götte M, et al. Strain analysis is superior to wall thickening in discriminating between infarcted myocardium with and without microvascular obstruction. Eur Radiol 2018; 28(12):5171-81. doi: 10.1007/s00330-018-5493-0.
doi: 10.1007/s00330-018-5493-0 pmid: 29948065 |
| [8] |
Fischer K, Linder OL, Erne SA, et al. Reproducibility and its confounders of CMR feature tracking myocardial strain analysis in patients with suspected myocarditis. Eur Radiol 2022; 32(5):3436-46. doi: 10.1007/s00330-021-08416-5.
doi: 10.1007/s00330-021-08416-5 |
| [9] |
Eitel I, Stiermaier T, Lange T, et al. Cardiac magnetic resonance myocardial feature tracking for optimized prediction of cardiovascular events following myocardial infarction. JACC Cardiovasc Imaging 2018; 11(10):1433-44. doi: 10.1016/j.jcmg.2017.11.034.
doi: S1936-878X(17)31176-2 pmid: 29454776 |
| [10] |
Gavara J, Rodriguez-Palomares JF, Valente F, et al. Prognostic value of strain by tissue tracking cardiac magnetic resonance after ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 2018; 11(10):1448-57. doi: 10.1016/j.jcmg.2017.09.017.
doi: S1936-878X(17)30985-3 pmid: 29248649 |
| [11] |
O'Regan DP, Ariff B, Baksi AJ, et al. Salvage assessment with cardiac MRI following acute myocardial infarction underestimates potential for recovery of systolic strain. Eur Radiol 2013; 23(5):1210-7. doi: 10.1007/s00330-012-2715-8.
doi: 10.1007/s00330-012-2715-8 pmid: 23179525 |
| [12] |
Reindl M, Tiller C, Holzknecht M, et al. Global longitudinal strain by feature tracking for optimized prediction of adverse remodeling after ST-elevation myocardial infarction. Clin Res Cardiol 2021; 110(1):61-71. doi: 10.1007/s00392-020-01649-2.
doi: 10.1007/s00392-020-01649-2 |
| [13] |
Kidambi A, Mather AN, Swoboda P, et al. Relationship between myocardial edema and regional myocardial function after reperfused acute myocardial infarction: an MR imaging study. Radiology 2013; 267(3):701-8. doi: 10.1148/radiol.12121516.
doi: 10.1148/radiol.12121516 pmid: 23382292 |
| [14] |
Zhao H, Lee AP, Li Z, et al. Impact of intramyocardial hemorrhage and microvascular obstruction on cardiac mechanics in reperfusion injury: a speckle-tracking echocardiographic study. J Am Soc Echocardiogr 2016; 29(10):973-82. doi: 10.1016/j.echo.2016.06.011.
doi: 10.1016/j.echo.2016.06.011 |
| [15] |
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012; 60(16):1581-98. doi: 10.1016/j.jacc.2012.08.001.
doi: 10.1016/j.jacc.2012.08.001 pmid: 22958960 |
| [16] |
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002; 105 (4):539-42. doi: 10.1161/hc0402.102975.
doi: 10.1161/hc0402.102975 pmid: 11815441 |
| [17] |
Zou Q, Zheng T, Zhou SL, et al. Quantitative evaluation of myocardial strain after myocardial infarction with cardiovascular magnetic resonance tissue-tracking imaging. Int Heart J 2020; 61(3):429-36. doi: 10.1536/ihj.19-384.
doi: 10.1536/ihj.19-384 pmid: 32350202 |
| [18] |
Bulluck H, Carberry J, Carrick D, et al. A noncontrast CMR risk score for long-term risk stratification in reperfused ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 2022; 15(3):431-40. doi: 10.1016/j.jcmg.2021.08.006.
doi: 10.1016/j.jcmg.2021.08.006 pmid: 35272808 |
| [19] |
He J, Yang W, Wu W, et al. Early diastolic longitudinal strain rate at MRI and outcomes in heart failure with preserved ejection fraction. Radiology 2022; 302(1):E5. doi: 10.1148/radiol.2021219026.
doi: 10.1148/radiol.2021219026 pmid: 34928734 |
| [20] |
Lee JW, Hur JH, Yang DH, et al. Guidelines for cardiovascular magnetic resonance imaging from the Korean Society of Cardiovascular Imaging-Part 2: interpretation of cine, flow, and angiography data. Korean J Radiol 2019; 20(11):1477-90. doi: 10.3348/kjr.2019.0407.
doi: 10.3348/kjr.2019.0407 pmid: 31606953 |
| [21] |
Carrick D, Haig C, Ahmed N, et al. Myocardial hemorrhage after acute reperfused ST-segment-elevation myocardial infarction: relation to microvascular obstruction and prognostic significance. Circ Cardiovasc Imaging 2016; 9(1):e004148. doi: 10.1161/circimaging.115.004148.
doi: 10.1161/circimaging.115.004148 |
| [22] |
Huang Y, Lei D, Chen Z, et al. Factors associated with microvascular occlusion in patients with ST elevation myocardial infarction after primary percutaneous coronary intervention. J Int Med Res 2021; 49(6): 3000605211024490. doi: 10.1177/03000605211024490.
doi: 10.1177/03000605211024490 |
| [23] |
Podlesnikar T, Pizarro G, Fernández-Jiménez R, et al. Left ventricular functional recovery of infarcted and remote myocardium after ST-segment elevation myocardial infarction (METOCARD-CNIC randomized clinical trial substudy). J Cardiovasc Magn Reson 2020; 22: (1):44. doi: 10.1186/s12968-020-00638-8.
doi: 10.1186/s12968-020-00638-8 |
| [24] |
Lange T, Stiermaier T, Backhaus SJ, et al. Functional and prognostic implications of cardiac magnetic resonance feature tracking-derived remote myocardial strain analyses in patients following acute myocardial infarction. Clin Res Cardiol 2021; 110(2):270-80. doi: 10.1007/s00392-020-01747-1.
doi: 10.1007/s00392-020-01747-1 pmid: 33083869 |
| [25] |
Zhang L, Mandry D, Chen B, et al. Impact of microvascular obstruction on left ventricular local remodeling after reperfused myocardial infarction. J Magn Reson Imaging 2018; 47(2):499-510. doi: 10.1002/jmri.25780.
doi: 10.1002/jmri.25780 pmid: 28580619 |
| [26] |
Pankaj G, Ananth K, James RJ, et al. Ventricular longitudinal function is associated with microvascular obstruction and intramyocardial haemorrhage. Open Heart 2016; 3(1): e000337. doi: 10.1136/openhrt-2015-000337.
doi: 10.1136/openhrt-2015-000337 |
| [27] |
Claus P, Omar AMS, Pedrizzetti G, et al. Tissue tracking technology for assessing cardiac mechanics: principles, normal values, and clinical applications. JACC Cardiovasc Imaging 2015; 8(12):1444-60. doi: 10.1016/j.jcmg.2015.11.001.
doi: S1936-878X(15)00845-1 pmid: 26699113 |
| [28] |
Regenfus M, Schlundt C, Krähner R, et al. Six-year prognostic value of microvascular obstruction after reperfused ST-elevation myocardial infarction as assessed by contrast-enhanced cardiovascular magnetic resonance. Am J Cardiol 2015; 116(7):1022-7. doi: 10.1016/j.amjcard2015.06.034.
doi: 10.1016/j.amjcard.2015.06.034 pmid: 26260397 |
| [29] |
Smiseth OA, Torp H, Opdahl A, et al. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J 2016; 37(15):1196-207. doi: 10.1093/eurheartj/ehv529.
doi: 10.1093/eurheartj/ehv529 pmid: 26508168 |
| [1] | Jianing Cui, Yanan Zhao, Wei Wang, Tao Li. Associations of Infarct Size and Regional Myocardial Function Examined by Cardiac Magnetic Resonance Feature Tracking Strain Analysis with the Infarct Location in Patients with Acute ST-Segment Elevation Myocardial Infarction [J]. Chinese Medical Sciences Journal, 2022, 37(4): 309-319. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|