Chinese Medical Sciences Journal ›› 2020, Vol. 35 ›› Issue (2): 121-134.doi: 10.24920/003630
• Original Article • Previous Articles Next Articles
Penehyclidine Hydrochloride Premedication Is Not Associated with Increased Incidence of Post-Operative Cognitive Dysfunction or Delirium:A Systemic Review and Meta-Analysis
Yao Yuntai1, a*( ), Ying Hua2, Fang Nengxin1a, Zhang Yongbao1b, Yuan Xin1c
), Ying Hua2, Fang Nengxin1a, Zhang Yongbao1b, Yuan Xin1c
- 1a. Department of Anesthesiology; Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100037, China
1b. Department of Vascular Surgery; Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100037, China
1c. Department of Adult Cardiac Surgery; Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100037, China
2. Department of Orthopaedics, Shanghai Key Laboratory of Orthopaedic Implants, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200011, China
-
Received:2019-06-15Accepted:2019-08-20Published:2020-06-30Online:2020-06-08 -
Contact:Yao Yuntai E-mail:yuntaiyao@126.com
Cite this article
Yao Yuntai,Ying Hua,Fang Nengxin,Zhang Yongbao,Yuan Xin. Penehyclidine Hydrochloride Premedication Is Not Associated with Increased Incidence of Post-Operative Cognitive Dysfunction or Delirium:A Systemic Review and Meta-Analysis[J].Chinese Medical Sciences Journal, 2020, 35(2): 121-134.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Patients and surgery data of the included studies (n=33)"
| Study | Surgery | Patient characteristics | Comparator drug(s) | Jadad assessment | ||||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Education | ASA | Randomization | Blindness | Withdrawals | |||
| Bi el al., 2012[ | Ortho, Uro | 75-89 | >High school | Ⅱ-Ⅲ | Scopolamine | 1 | 0 | 1 |
| Chen el al., 2011[ | Ex, Ab | >65 | 6-9 years | Ⅰ-Ⅲ | Saline | 1 | 0 | 1 |
| Guo el al., 2010[ | Ex, Ab | 20-59 | 6-9 years | Ⅰ-Ⅱ | Atropine | 1 | 0 | 1 |
| Guo el al., 2014[ | Ab | 61-73 | NR | NR | Penehyclidine | 1 | 0 | 1 |
| Hu el al., 2015[ | Thorax | 61-80 | NR | Ⅱ-Ⅲ | Penehyclidine | 2 | 0 | 1 |
| Kong el al., 2010[ | Ab | ≥60 | >9 years | Ⅰ-Ⅱ | Atropine/Scopolamine/Saline | 1 | 0 | 1 |
| Li el al., 2008[ | NCS | >60 | NR | Ⅰ-Ⅱ | Atropine | 1 | 0 | 1 |
| Li el al., 2009[ | LC | 65-75 | Illiteracy | Ⅰ-Ⅲ | Saline | 1 | 1 | 1 |
| Li el al., 2010[ | NCS | >60 | NR | Ⅰ-Ⅳ | Atropine | 1 | 0 | 1 |
| Li el al., 2012[ | LC | 60-80 | NR | Ⅰ-Ⅲ | Penehyclidine | 1 | 0 | 1 |
| Liao el al., 2017[ | Ortho | ≥60 | NR | Ⅰ-Ⅱ | Atropine/Saline | 1 | 0 | 1 |
| Liu el al., 2009[ | NCS | >65 | NR | Ⅰ-Ⅱ | Atropine | 1 | 0 | 1 |
| Liu el al., 2013[ | NCS | 60-85 | NR | Ⅰ-Ⅲ | Atropine | 1 | 0 | 1 |
| Liu el al., 2014[ | NR | 52-79 | NR | NR | Penehyclidine | 1 | 0 | 1 |
| Liu el al., 2015[ | Thyroid | 18-85 | NR | Ⅰ-Ⅱ | Atropine/Saline | 1 | 0 | 1 |
| Liu el al., 2016[ | NCS | 34-67 | NR | Ⅱ-Ⅲ | Penehyclidine | 2 | 0 | 1 |
| Lv el al., 2009[ | Maxillo-facial | 61-79 | Mixed | Ⅰ-Ⅲ | Atropine | 1 | 1 | 1 |
| Shu el al., 2009[ | NCS | 65-78 | NR | Ⅱ-Ⅲ | Atropine/Scopolamine | 1 | 0 | 1 |
| Shu el al., 2013[ | NCS | 65-78 | NR | Ⅱ-Ⅲ | Penehyclidine | 1 | 0 | 1 |
| Tang el al., 2010[ | CS | 15-55 | NR | Ⅱ-Ⅲ | Saline | 1 | 0 | 1 |
| Wang el al., 2013[ | Mixed | 35-60 | NR | Ⅱ-Ⅲ | Scopolamine | 1 | 1 | 1 |
| Wang el al., 2017[ | Thorax | 43-65 | NR | Ⅰ-Ⅱ | Saline/Ulinastatin | 1 | 0 | 1 |
| Wu el al., 2010[ | Ab | 65-75 | >9 years | Ⅱ-Ⅲ | Saline | 1 | 0 | 1 |
| Wu el al., 2014[ | Ab | 60-83 | NR | Ⅰ-Ⅲ | Scopolamine | 1 | 0 | 1 |
| Xia el al., 2017[ | NCS | 60-78 | NR | Ⅰ-Ⅲ | Atropine | 2 | 0 | 1 |
| Xiang el al., 2011[ | Thorax, Ab | 60-80 | NR | NR | Atropine | 1 | 0 | 1 |
| Xu el al., 2008[ | Ab | >65 | >9 years | Ⅰ-Ⅲ | Saline | 1 | 0 | 1 |
| Yang el al., 2011[ | LC | 64-70 | NR | NR | Atropine | 1 | 0 | 1 |
| Ye el al., 2011[ | Ex | 65-90 | NR | Ⅰ-Ⅲ | Atropine/Saline | 1 | 0 | 1 |
| Ye el al., 2015[ | LC | 65-80 | >5 years | Ⅰ-Ⅱ | Saline | 2 | 0 | 1 |
| Yu el al., 2011[ | Vocal cord | 31-70 | NR | Ⅰ-Ⅱ | Atropine/Scopolamine | 1 | 0 | 1 |
| Zhang el al., 2012[ | NCS | >65 | >9 years | Ⅰ-Ⅲ | Saline | 1 | 0 | 1 |
| Zou el al., 2017[ | NCS | 65-76 | NR | Ⅰ-Ⅲ | Atropine | 2 | 0 | 1 |
Table 2
PHC administration scheme and reported outcomes of the included trials (n=33)"
| Studies | Sample size | Groups (n) | PHC group | Control group | Outcomes reported | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Dose | Route | Timing | n | Comparator | Dose | POCD | POD | MMSE | |||||
| Bi et al., 2012[ | 90 | 3 | 30 | 0.002 mg/kg | iv | After iv access | 30 | Scopolamine | 0.002 mg/kg | √ | - | √ | ||
| 30 | 0.01 mg/kg | iv | ||||||||||||
| Chen et al., 2011[ | 124 | 3 | 42 | 0.5 mg | iv | 10’ BA | 42 | Saline | Same volume | √ | - | √ | ||
| 40 | 1.0 mg | iv | ||||||||||||
| Guo et al., 2010[ | 300 | 6 | 50 | 0.008 mg/kg | im | 10’ BA | 50 | Atropine | 0.08 mg/kg | √ | - | √ | ||
| 50 | 0.01 mg/kg | |||||||||||||
| 50 | 0.012 mg/kg | |||||||||||||
| 50 | 0.014 mg/kg | |||||||||||||
| 50 | 0.016 mg/kg | |||||||||||||
| Kong et al., 2010[ | 320 | 4 | 78 | 1.0 mg | im | 30’ BA | 80 | Saline | Same volume | √ | - | √ | ||
| 80 | Scopolamine | 0.3 mg | ||||||||||||
| 82 | Atropine | 0.5 mg | ||||||||||||
| Li et al., 2008[ | 80 | 2 | 40 | 0.01 mg/kg | iv | 30’ BA | 40 | Atropine | 0.01 mg/kg | - | √ | - | ||
| Li et al., 2009[ | 120 | 3 | 40 | 0.5 mg | iv | 10’ BA | 40 | Saline | Same volume | - | √ | √ | ||
| 40 | 1.0 mg | |||||||||||||
| Li et al., 2010[ | 289 | 3 | 98 | 0.01 mg/kg | im | 30’ pre-op | 96 | Atropine | 0.01 mg/kg | - | √ | - | ||
| 95 | 0.02 mg/kg | |||||||||||||
| Liao et al., 2017[ | 144 | 3 | 48 | 1.0 mg | im | 30’ pre-op | 48 | Blank | - | √ | √ | - | ||
| 48 | Atropine | 0.5 mg | ||||||||||||
| Liu et al., 2009[ | 60 | 2 | 30 | 0.5 mg | im | 30’ pre-op | 30 | Atropine | 0.5 mg | √ | - | √ | ||
| Liu et al., 2013[ | 60 | 2 | 30 | 0.5 mg | iv | 10’ BA | 30 | Atropine | 0.5 mg | √ | - | √ | ||
| Liu et al., 2015[ | 116 | 4 | 29 | 0.01 mg/kg | iv | 30’ BA | 29 | Saline | Same volume | - | - | √ | ||
| 29 | 0.02 mg/kg | 29 | Atropine | 0.06 mg/kg | ||||||||||
| Lv et al., 2009[ | 120 | 2 | 60 | 0.01 mg/kg | iv | 30’ pre-op | 60 | Atropine | 0.01 mg/kg | √ | - | √ | ||
| Shu et al., 2009[ | 120 | 3 | 40 | 0.5 mg | im | 30’ BA | 40 | Scopolamine | 0.3 mg | √ | - | √ | ||
| 40 | Atropine | 0.5 mg | ||||||||||||
| Tang et al., 2010[ | 40 | 2 | 20 | 0.015 mg/kg | im | 30’ BA | 20 | Saline | Same volume | √ | - | √ | ||
| Wang et al., 2013[ | 60 | 2 | 30 | 1.0 mg | im | Pre-op | 30 | Scopolamine | 0.3 mg | - | √ | - | ||
| Wang et al., 2017[ | 60 | 2 | 30 | 0.02 mg/kg | iv | 15’ BA | 30 | Saline | Same volume | - | - | √ | ||
| Wu et al., 2010[ | 71 | 2 | 40 | 0.5 mg | iv | 10’ BA | 31 | Saline | Same volume | √ | √ | √ | ||
| Wu et al., 2014[ | 120 | 4 | 30 | 0.005 mg/kg | im | 40’ BA | 30 | Scopolamine | 0.006 mg/kg | √ | √ | - | ||
| 30 | 0.01 mg/kg | |||||||||||||
| 30 | 0.02 mg/kg | |||||||||||||
| Xia et al., 2017[ | 90 | 2 | 45 | 0.5 mg | iv | 10’ BA | 45 | Atropine | 0.5 mg | √ | - | √ | ||
| Xiang et al., 2011[ | 80 | 2 | 40 | 1.0 mg | im | 30’ pre-op | 40 | Atropine | 0.5 mg | - | - | √ | ||
| Xu et al., 2008[ | 80 | 2 | 42 | 0.5 mg | iv | 10’ BA | 38 | Saline | Same volume | √ | √ | √ | ||
| Yang et al., 2011[ | 64 | 2 | 32 | 0.01-0.02 mg/kg | im | 40’ BA | 32 | Atropine | 0.008-0.01 mg/kg | - | - | √ | ||
| Ye et al., 2011[ | 180 | 3 | 60 | 1.0 mg | im | 30’ BA | 60 | Saline | Same volume | √ | - | √ | ||
| 60 | Atropine | 0.5 mg | ||||||||||||
| Ye et al., 2015[ | 60 | 3 | 20 | 0.01 mg/kg | iv | 30’ BA | 20 | Saline | Same volume | √ | - | √ | ||
| 20 | 0.02 mg/kg | |||||||||||||
| Ye et al., 2015[ | 241 | 4 | 80 | 0.5 mg | iv | 40’ BA | 50 | Scopolamine | 0.3 mg | - | √ | - | ||
| 61 | 1.0 mg | 50 | Atropine | 0.5 mg | ||||||||||
| Zhang et al., 2012[ | 60 | 2 | 30 | 0.02 mg/kg | iv | 10’ BA | 30 | Saline | Same volume | √ | √ | - | ||
| Zou et al., 2017[ | 120 | 2 | 60 | 0.5 mg | iv | 10’ BA | 60 | Atropine | 0.5 mg | - | - | √ | ||
| Guo et al., 2014[ | 60 | 3 | 20 | 0.004 mg/kg | im | 30’ BA | - | √ | - | √ | ||||
| 20 | 0.008 mg/kg | |||||||||||||
| 20 | 0.012 mg/kg | |||||||||||||
| Hu et al., 2015[ | 146 | 2 | 73 | 0.005 mg/kg | iv | 30’ BA | - | √ | - | √ | ||||
| 73 | 0.015 mg/kg | |||||||||||||
| Li et al., 2012[ | 120 | 4 | 30 | 0.25 mg | iv | 5’ BA | - | √ | √ | √ | ||||
| 30 | 0.50 mg | |||||||||||||
| 30 | 0.75 mg | |||||||||||||
| 30 | 1.00 mg | |||||||||||||
| Liu et al., 2014[ | 200 | 5 | 40 | 0.008 mg/kg | iv | 30’ BA | - | √ | √ | - | ||||
| 40 | 0.011 mg/kg | |||||||||||||
| 40 | 0.014 mg/kg | |||||||||||||
| 40 | 0.017 mg/kg | |||||||||||||
| 40 | 0.020 mg/kg | |||||||||||||
| Liu et al., 2016[ | 102 | 3 | 34 | 0.50 mg | in | 20’ BA | - | - | - | √ | ||||
| 34 | 1.00 mg | |||||||||||||
| 34 | 1.50 mg | |||||||||||||
| Shu et al., 2013[ | 120 | 3 | 40 | 0.005 mg/kg | iv | 30’ BA | - | √ | - | √ | ||||
| 40 | 0.010 mg/kg | |||||||||||||
| 40 | 0.015 mg/kg | |||||||||||||
Table 3
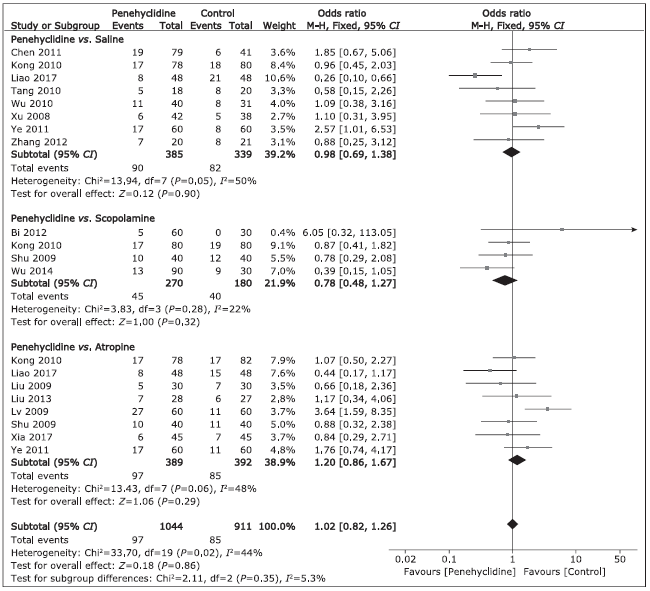
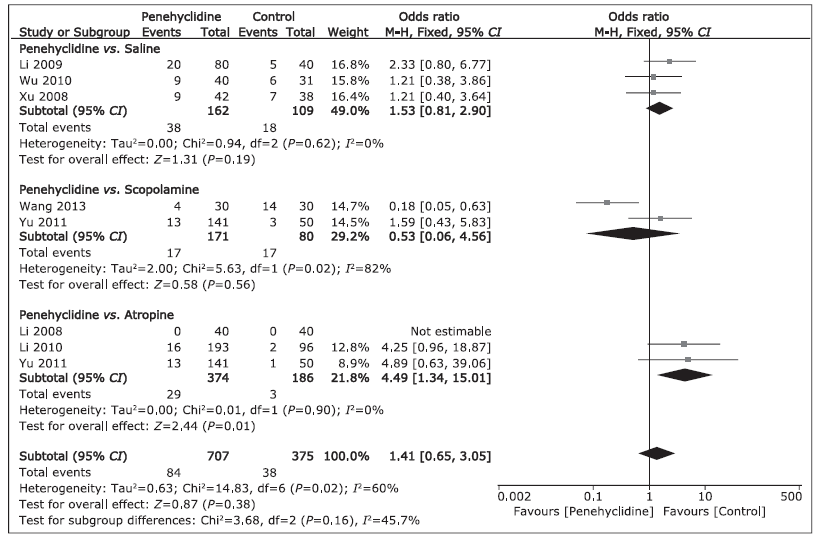
Comparison of incidences of POCD and POD between groups of penehyclidine and contrals"
| Incidence of the outcomes (%) | Trials (n) | Group PHC (n) | Group Control (n) | Heterogeneity | Analysis model | OR | 95% CI | Overall effect P | |
|---|---|---|---|---|---|---|---|---|---|
| I2 (%) | P | ||||||||
| POCD | |||||||||
| Penehyclidine vs. Saline | 8 | 385 | 339 | 50 | 0.05 | M-H, random | 0.97 | 0.58,1.64 | 0.92 |
| Penehyclidine vs. Scopolamine | 4 | 270 | 180 | 22 | 0.28 | M-H, fixed | 0.78 | 0.48,1.27 | 0.32 |
| Penehyclidine vs. Atropine | 8 | 389 | 392 | 48 | 0.06 | M-H, fixed | 1.20 | 0.86,1.67 | 0.29 |
| POD | |||||||||
| Penehyclidine vs. Saline | 3 | 162 | 109 | 0 | 0.62 | M-H, fixed | 1.53 | 0.81,2.90 | 0.19 |
| Penehyclidine vs. Scopolamine | 2 | 171 | 80 | 82 | 0.02 | M-H, random | 0.53 | 0.06,4.56 | 0.56 |
| Penehyclidine vs. Atropine | 3 | 374 | 186 | 0 | 0.90 | M-H, fixed | 4.49 | 1.34,15.01 | 0.01 |
Table 4
Comparison of MMSE scores of POD between the PHC group and the control groups"
| Outcomes | Trials (n) | Group PHC (n) | Group Control (n) | Heterogeneity | Analysis model | WMD | 95% CI | Overall effect P | |
|---|---|---|---|---|---|---|---|---|---|
| I2 (%) | P | ||||||||
| Penehyclidine vs. Saline | |||||||||
| Pre-op | 9 | 493 | 390 | 0 | 0.97 | IV, fixed | 0.10 | -0.11,0.31 | 0.34 |
| POD1 | 5 | 214 | 197 | 95 | <0.00001 | IV, random | -0.22 | -1.82,1.38 | 0.79 |
| POD2 | 4 | 187 | 151 | 95 | <0.00001 | IV, random | 0.14 | -1.62,1.90 | 0.88 |
| POD3 | 5 | 178 | 139 | 89 | <0.00001 | IV, random | -0.68 | -1.87,0.51 | 0.26 |
| POD5 | 1 | 60 | 60 | NA | NA | IV, random | -2.30 | -2.87,-1.73 | <0.00001 |
| POD7 | 2 | 118 | 111 | 0 | 0.55 | IV, fixed | 0.07 | -0.37,0.52 | 0.75 |
| Penehyclidine vs. Scopolamine | |||||||||
| Pre-op | 3 | 208 | 148 | 57 | 0.05 | IV, random | 0.11 | -0.17,0.39 | 0.44 |
| POD1 | 3 | 208 | 148 | 97 | <0.00001 | IV, random | 0.88 | -0.36,2.13 | 0.17 |
| POD2 | 3 | 208 | 148 | 95 | <0.00001 | IV, random | 0.87 | -0.04,1.78 | 0.06 |
| POD3 | 2 | 130 | 70 | 71 | 0.02 | IV, random | -0.12 | -0.51,0.27 | 0.54 |
| POD5 | 0 | NA | NA | NA | NA | NA | NA | NA | NA |
| POD7 | 1 | 78 | 78 | NA | NA | IV, random | 0.20 | -0.30,0.70 | 0.44 |
| Penehyclidine vs. Atropine | |||||||||
| Pre-op | 12 | 771 | 546 | 40 | 0.04 | IV, fixed | -0.02 | -0.18,0.13 | 0.78 |
| POD1 | 8 | 399 | 374 | 81 | <0.00001 | IV, random | -0.38 | -1.09,0.32 | 0.29 |
| POD2 | 3 | 178 | 182 | 4 | 0.35 | IV, fixed | -0.16 | -0.55,0.22 | 0.41 |
| POD3 | 4 | 193 | 193 | 81 | 0.001 | IV, random | -0.23 | -1.20,0.74 | 0.64 |
| POD5 | 2 | 310 | 110 | 79 | 0.0002 | IV, random | 0.95 | -1.09,3.00 | 0.36 |
| POD7 | 5 | 210 | 214 | 96 | <0.00001 | IV, Random | -0.74 | -2.57,1.08 | 0.42 |
Table 5
Incidences of POCD, POD,and POCD+POD compared between different PHC dosages"
| Outcomes | Trials (n) | Dosage 1 Events/Patients | Dosage 2 Events/Patients | Heterogeneity | Analysis model | OR | 95% CI | Overall effect P | |
|---|---|---|---|---|---|---|---|---|---|
| I2 (%) | P | ||||||||
| 1.0 mg | 0.5 mg | ||||||||
| POCD | 2 | 22/69 | 6/70 | 56 | 0.13 | M-H, random | 6.00 | 0.67,53.51 | 0.11 |
| POD | 3 | 28/131 | 15/150 | 0 | 0.78 | M-H, fixed | 2.36 | 1.19,4.69 | 0.01 |
| POCD+POD | 4 | 50/200 | 21/220 | 0 | 0.52 | M-H, fixed | 3.05 | 1.75,5.29 | <0.0001 |
| 0.01 mg/kg | 0.02 mg/kg | ||||||||
| POCD | 3 | 9/90 | 29/90 | 0 | 0.82 | M-H, fixed | 0.23 | 0.10,0.53 | 0.0005 |
| POD | 2 | 5/138 | 21/135 | 0 | 0.96 | M-H, fixed | 0.20 | 0.07,0.56 | 0.002 |
| POCD+POD | 4 | 14/228 | 50/225 | 0 | 0.98 | M-H, fixed | 0.22 | 0.12,0.41 | <0.00001 |
| 0.01 mg/kg | 0.015 mg/kg | ||||||||
| POCD | 2 | 13/80 | 18/80 | 0 | 0.56 | M-H, fixed | 0.66 | 0.29,1.48 | 0.31 |
| POD | 1 | 2/40 | 2/40 | NA | NA | NA | 1.00 | 0.13,7.47 | 1.00 |
| POCD+PD | 2 | 15/120 | 20/120 | 0 | 0.79 | M-H, fixed | 0.70 | 0.33,1.47 | 0.34 |
| 0.01 mg/kg | 0.008 mg/kg | ||||||||
| POCD | 2 | 10/60 | 4/60 | 0 | 0.98 | M-H, fixed | 3.09 | 0.86,11.08 | 0.08 |
| POD | 1 | 2/40 | 2/40 | NA | NA | NA | 5.26 | 0.24,113.11 | 0.29 |
| POCD+POD | 2 | 4/100 | 12/100 | 0 | 0.95 | M-H, fixed | 3.39 | 1.05,10.98 | 0.04 |
| 0.01 mg/kg | 0.005 mg/kg | ||||||||
| POCD | 3 | 22/90 | 13/90 | 31 | 0.23 | M-H, fixed | 1.95 | 0.90,4.22 | 0.09 |
| POD | 0 | 0 | 0 | NA | NA | NA | NA | NA | NA |
| POCD+POD | 3 | 22/90 | 13/90 | 31 | 0.23 | M-H, fixed | 1.95 | 0.90,4.22 | 0.09 |
Table 6
Influence of statistical model on estimated treatment effects of primary outcomes"
| Statistical model | OR (95% CI) of POCD | OR (95% CI) of POD | |||||
|---|---|---|---|---|---|---|---|
| PHC vs. SAL | PHC vs. SCO | PHC vs. ATR | PHC vs. SAL | PHC vs. SCO | PHC vs. ATR | ||
| Fixed effects | 0.98 (0.69,1.38) | 0.78 (0.48,1.27) | 1.20 (0.86,1.67) | 1.56 (0.83,2.93) | 0.53 (0.24,1.16) | 4.51 (1.35,15.08) | |
| Random effects | 0.97 (0.58,1.64) | 0.73(0.40,1.32) | 1.13 (0.70,1.83) | 1.53 (0.81,2.90) | 0.53 (0.06,4.56) | 4.49 (1.34,15.01) | |
| 1. |
Kotekar N, Shenkar A, Nagaraj R . Postoperative cognitive dysfunction-current preventive strategies. Clin Interv Aging 2018; 13:2267-73. doi: 10.2147/CIA.S133896.
doi: 10.2147/CIA.S133896 pmid: 30519008 |
| 2. |
Brown C 4th, Deiner S. Perioperative cognitive protection. Br J Anaesth 2016; 117(suppl 3):iii52-iii61. doi: 10.1093/bja/aew361.
doi: 10.1093/bja/aew248 pmid: 28077539 |
| 3. |
Benhamou D, Brouquet A . Postoperative cerebral dysfunction in the elderly: diagnosis and prophylaxis. J Visc Surg 2016; 153(6S):S27-S32. doi: 10.1016/j.jviscsurg.2016.09.015.
doi: 10.1016/j.jviscsurg.2016.09.015 pmid: 27789263 |
| 4. |
Cropsey C, Kennedy J, Han J , et al. Cognitive dysfunction, delirium, and stroke in cardiac surgery patients. Semin Cardiothorac Vasc Anesth 2015; 19(4):309-17. doi: 10.1177/1089253215570062.
doi: 10.1177/1089253215570062 pmid: 26660055 |
| 5. | Krenk L, Rasmussen LS . Postoperative delirium and postoperative cognitive dysfunction in the elderly-what are the differences? Minerva Anestesiol 2011; 77(7):742-9. |
| 6. |
Deiner S, Silverstein JH . Postoperative delirium and cognitive dysfunction. Br J Anaesth 2009; 103(Suppl 1):i41-6. doi: 10.1093/bja/aep291.
doi: 10.1093/bja/aep291 |
| 7. |
Bottiggi KA, Salazar JC, Yu L , et al. Long-term cognitive impact of anticholinergic medications in older adults. Am J Geriatr Psychiatry 2006; 14(11):980-4. doi: 10.1097/01.JGP.0000224619.87681.71.
doi: 10.1097/01.JGP.0000224619.87681.71 pmid: 17068321 |
| 8. |
Renner UD, Oertel R, Kirch W . Pharmacokinetics and pharmacodynamics in clinical use of scopolamine. Ther Drug Monit 2005; 27(5):655-65. doi: 10.1097/01.ftd.0000168293.48226.57.
doi: 10.1097/01.ftd.0000168293.48226.57 pmid: 16175141 |
| 9. |
Anderson S, McGuire R, McKeown D. Comparison of the cognitive effects of premedication with hyoscine and atropine. Br J Anaesth 1985; 57(2):169-73. doi: 10.1093/bja/57.2.169.
doi: 10.1093/bja/57.2.169 pmid: 3882109 |
| 10. |
Han XY, Liu H, Liu CH , et al. Synthesis of the optical isomers of a new anticholinergic drug, penehyclidine hydrochloride (8018). Bioorg Med Chem Lett 2005; 15:1979-82. doi: 10.1016/j.bmcl.2005.02.071.
doi: 10.1016/j.bmcl.2005.02.071 |
| 11. | Chen XZ. Penehyclidine hydrochloride. Cent S Pharm 2003; 1:188-9.Chinese. doi: 10.3969/j.issn.1672-2981.2003.03.028. |
| 12. |
Li BQ, Sun HC, Nie SN , et al. Effect of penehyclidine hydrochloride on patients with acute lung injury and its mechanisms. Chin J Traumatol 2010; 13(6):329-35. doi: 10.3760/cma.j.issn.1008-1275.2010.06.002.
doi: 10.3760/cma.j.issn.1008-1275.2010.06.002 |
| 13. |
Xiao HT, Liao Z, Tong RS . Penehyclidine hydrochloride: a potential drug for treating COPD by attenuating Toll-like receptors. Drug Des Devel Ther 2012; 6:317-22. doi: 10.2147/DDDT.S36555.
doi: 10.2147/DDDT.S36555 pmid: 23139625 |
| 14. |
Zhang Z, Zhuang Y, Ouyang F , et al. Penehyclidine enhances the efficacy of tropisetron in prevention of PONV following gynecological laparoscopic surgery. J Anesth 2012; 26(6):864-9. doi: 10.1007/s00540-012-1443-1.
doi: 10.1007/s00540-012-1443-1 |
| 15. |
Sun YJ, Song DD, Diao YG , et al. Penehyclidine hydrochloride preserves the intestinal barrier function in patients undergoing cardiopulmonary bypass. J Thorac Cardiovasc Surg 2013; 146(1):179-85. doi: 10.1016/j.jtcvs.2013.01.042.
doi: 10.1016/j.jtcvs.2013.01.042 pmid: 23434449 |
| 16. |
Shamseer L, Moher D, Clarke M , et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 350:g7647. doi: 10.1136/bmj.g7647.
doi: 10.1136/bmj.g7647 pmid: 25555855 |
| 17. |
Clark HD, Wells GA, Hu?t C , et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials 1999; 20(5):448-52. doi: 10.1016/S0197-2456(99)00026-4.
doi: 10.1016/s0197-2456(99)00026-4 pmid: 10503804 |
| 18. | Wu JL, Zhang DY, Yang XL , et al. Effects of preoperative administration of penehyclidine hydrochloride on early cognitive function in aged patients with type 2 diabetes mellitus after operation. Chongqing Med 2010; 39(18):2468-69+72. Chinese. doi: 10.3969/.j.issn.1671-8348.2010.18.036. |
| 19. | Chen H, Zhang ZW. Effects of different doses of penehyclidine hydrochloride on early post-operative cognitive dysfunction. Guide China Med 2011; 9(25):271-2. Chinese. doi: 671-8194(2011)25-0271-02 |
| 20. | Guo CN, Xia XQ, Xia SJ. Effects of different doses of penehyclidine hydrochloride on post-operative cognitive dysfunction. J Wannan Med University 2010; 29(2):149-50. Chinese. doi: 1002-0217(2010)02-0149-02 |
| 21. | Li SJ. Effects of different doses of penehyclidine hydrochloride on post-operative cognitive dysfunction in elderly patients. Contemporary Medicine 2012, 18(15):145-6. Chinese. doi: 10.3969/j.issn.1009-4393.2012.15.102. |
| 22. | Li K, Yu T, Yin L , et al. Effect of premedication with different doses of penehyclidine hydrochloride on postoperative delirium in elderly patients. J Clin Anesthesiol 2010; 26(12):1049-50. Chinese. |
| 23. | Yu LZ, Li SH, Cao ZF , et al. Comparison of different anti-cholinergic agents used in patients undergoing laryngoscopy. Guide China Med 2011; 9(4):71-2. Chinese. doi: 10.3969/j.issn.1671-8194.2011.04.043. |
| 24. | Li W, Xia Q, Yang TF , et al. Comparison of penehyclidine hydrochloride and atropine as premedication in laparoscopic cholecystectomy. China Modern Doctor 2008; 46(24):42-3. Chinese. doi: 10.3969/j.issn.1673-9701.2008.24.019. |
| 25. | Liu X, Liu HT. Effect of pre-operative small dose of penehyclidine hydrochloride on cognitive function in patients undergoing thyroidectomy under general anesthesia. Shandong Med 2015; 55(7):88-9. Chinese. doi: 10.3969/j.issn.1002-266X.2015.07.035. |
| 26. | Liu Y, Liu XF, Gu RN , et al. Effect of penehyclidine hydrochloride premedication on post-operative cognitive function in elderly patients. Hebei Med J 2013; 35(10):1469-70. Chinese. doi: 10.3969/j.issn.1002-7386.2013.10.010. |
| 27. | Shu SH, Pan JH, Fang C , et al. Effect of pre-operative penehyclidine hydrochloride on post-operative cognitive function in elderly patients. J Clin Anesthesiol 2009; 25(8):658-60. Chinese. |
| 28. | Xu KQ, Zhang T, Xiao LC , et al. Effect of penehyclidine hydrochloride on cognitive function in elderly patients during early post-operative period. Chin Arch Gen Surg 2008; 2(6):488-9. Chinese. doi: 10.3969/j.issn.1674-0793.2008.06.019. |
| 29. | Liu W, Wang XB. Effects of penequinine hydrochloride on incidence of early post-operative cognitive dysfunction in elderly non-cardiac surgery. Qinghai Med J 2009; 39(11):9-11.Chinese. |
| 30. | Zhang W, Zhang EX, Kan QC , et al. Effect of penequinine hydrochloride on cognitive dysfunction early after non-cardiac surgery in elderly patients. J Clin Anesthesiol 2012; 28(2):113-4.Chinese. |
| 31. | Li ZH, Zhou B, Zhao JS , et al. Effects of penehyclidine application before operation on postoperative mental function in the elderly patients. Clin J Med Offi 2009; 37(6):1016-8. Chinese. |
| 32. | Wang M, Gao B, Ma Y , et al. Effects and mechanism of penehyclidine hydrochloride combined with ulinastatin on post-operative cognitive function in patients undergoing thoracic surgery. Chongqing Med 2017;46(12):1602-5. Chinese. doi: 10.3969/j.issn.1671-8348.2017.12.006. |
| 33. | Wang HQ, Ma DM. Comparison of penehyclidine hydrochloride and scopolamine applied to tumor whole body hyperthermia as premedication. China Modern Med 2013; 20(30):87-9. Chinese. |
| 34. | Bi GY, Wang SY, Yang SH. Effect of penehyclidine hydrochloride as premedication of epidural anesthesia on post-cognitive function of elderly patients. Chin Med Guide 2012;14(1):47-8. Chinese. doi: 10.3969/j.issn.1009-0959.2012.01.030. |
| 35. | Lv WM, Luo YL, Yu C , et al. Effect of penehyclidine hydrochloride as premedication of general anesthesia on post-operative cognitive dysfunction of elderly patients. J Chongqing Med Univ 2009; 34(3):365-7. Chinese. |
| 36. | Xia XG, Ding HY, Yang HSZ. Effects of penehyclidine hydrochloride as general anesthesia premedication on postoperative cognitive impairment in elderly patients. China Modern Doctor 2017; 55(6):113-5.Chinese. |
| 37. | Zou JH, Zhou J. The influence of penehyclidine hydrochloride as general anesthesia premedication on postoperative cognitive in elderly patients. China J Pharmaceuti Economics 2017; 12(12):85-7. Chinese. doi: 10.12010/j.issn.1673-5846.2017.12.029. |
| 38. | Tang X, Lu KZ. Effect of penehyclidine hydrochloride as preoperative medication in extra-corporeal circulation on cognitive dysfunction. Chongqing Med 2010; 39(17):2304-6. Chinese. doi: 10.3969/j.issn.1671-8348.2010.17.025. |
| 39. | Kong L, Hu ZC, Xu PC. Comparison of penehyclidine, scopolamine and atropine on post-operative cognition in elderly patients receiving general anesthesia. Chin J Gerontology 2010; 30(10):1358-60. Chinese. doi: 10.3969/j.issn.1005-9202.2010.10.019. |
| 40. | Wu LN, Meng HB, Ding GY. Impact of penehyclibine hydrochloride on abdominal early post-operative cognitive function of elderly patients with coronary heart disease. Guide China Med 2014;11(35):15-9, 24.Chinese. |
| 41. | Ye FQ, Wu SM, Ye XX , et al. The effect of penehyclibine on post-operative cognitive function in senile patients. Modern Hospital 2011; 11(5):31-2. Chinese. doi: 10.3969/j.issn.1671-332X.2011.05.014. |
| 42. | Xiang LQ. Comparison of penehyclidine and atropine on post-operative cognition in elderly patients receiving general anesthesia. Med J West China 2011; 23(6):1110-2. Chinese. doi: 10.3969/j.issn.1672-3511.2011.06.053. |
| 43. | Yang AB, Zhang MQ. Analysis of penehyclidine and atropine on post-operative cognition in elderly patients receiving general anesthesia. China Foreign Med Treat 2011; 30(21):118. Chinese. doi: 10.16662/j.cnki.1674-0742.2011.21.083. |
| 44. | Liao SG, Li K, Zhang GH. The effects of penehyclibine on post-operative cognitive function in the elderly patients undergoing orthopedic surgery. China Contemp Med 2017; 24(35):110-2. Chinese. doi: 10.3969/j.issn.1674-4721.2017.35.037. |
| 45. | Ye XL . ( 2015). Effect of penehyclidine hydrochloride on early cognitive function in elderly patients after laparoscopic cholecystectomy (Master’s thesis). Available from CNKI Dissertation Database. Chinese. |
| 46. | Liu Y, Zhang JG, Hu YP , et al. Influence of penehyclidine hydrochloride on post-operative cognitive function. Lab Med Clin 2014; 11(18):2537-8. Chinese. doi: 10.3969/j.issn.1672-9455.2014.18.016. |
| 47. | Shu SH, Cai XQ, Zhou L , et al. Effects of different doses of penehyclidine hydrochloride on early post-operative cognitive dysfunction in elderly. J Clin Anesthesiol 2013; 29(01):28-30. Chinese. |
| 48. | Hu WL, Han WL, Yang W , et al. The effects of low dose of penehyclibine hydrochloride on post-operative cognitive function in elderly patients undergoing radical surgery for esophagus cancer. Chongqing Med 2015; 44(8):1122-3. Chinese. doi: 10.3969/j.issn.1671-8348.2015.08.040. |
| 49. | Liu XH , Chen YS. The effects of small dose of penehyclibine hydrochloride on respiratory and cognition in elderly patients receiving general anesthesia. Modern Diag Treat 2016; 27(12):2211-2. Chinese. |
| 50. | Guo F, Dong H. Effect of penehyclibine hydrochloride on post-operative cognitive function in elderly patients. Guide China Med 2014; 12(35):54-7. Chinese. doi: 10.15912/j.cnki.gocm.2014.35.035. |
| 51. |
Rautakorpi P, Manner T, Kanto J . A survey of current usage of anticholinergic drugs in paediatric anaesthesia in Finland. Acta Anaesthesiol Scand 1999; 43(10):1057-9. doi: 10.1034/j.1399-6576.1999.431015.x.
doi: 10.1034/j.1399-6576.1999.431015.x pmid: 10593471 |
| 52. | Liang P, Zhang Y, Yu H , et al. Effects of penehyclidine hydrochloride on the propofol dose requirement and Bispectral Index for loss of consciousness. Int J Clin Exp Med 2014; 7(8):2236-41. Chinese. |
| 53. |
Wang J, Ren Y, Zhu Y , et al. Effect of penehyclidine hydrochloride on the incidence of intra-operative awareness in Chinese patients undergoing breast cancer surgery during general anaesthesia. Anaesthesia 2013; 68(2):136-41. doi: 10.1111/anae.12092.
doi: 10.1111/anae.12092 |
| 54. |
Mu DL, Li LH, Wang DX , et al. High postoperative serum cortisol level is associated with increased risk of cognitive dysfunction early after coronary artery bypass graft surgery: a prospective cohort study. PLoS One 2013; 8(10):e77637. doi: 10.1371/journal.pone.0077637.
doi: 10.1371/journal.pone.0077637 pmid: 24143249 |
| 55. |
Youngblom E, DePalma G, Sands L, et al. The temporal relationship between early postoperative delirium and postoperative cognitive dysfunction in older patients: a prospective cohort study. Can J Anesth 2014; 61(12):1084-92. doi: 10.1007/s12630-014-0242-6.
doi: 10.1007/s12630-014-0242-6 pmid: 25287962 |
| 56. |
Moller JT, Cluitmans P, Rasmussen LS , et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet 1998; 351(9106):857-61. doi: 10.1016/s0140-6736(97)07382-0.
doi: 10.1016/s0140-6736(97)07382-0 pmid: 9525362 |
| 57. |
Carnero-Pardo C . Should the mini-mental state examination be retired? Neurologia 2014; 29(8):473-81. doi: 10.1016/j.nrl.2013.07.003.
doi: 10.1016/j.nrl.2013.07.003 |
| 58. | Yong XL, Li N, Du XL , et al. Study on safety and tolerability of single-dose of penehyclidine hydrochloride in healthy volunteers. Chin J New Drugs 2015; 24(7):804-7. Chinese. doi: 1003-3734(2015)07-0804-04. |
| 59. | Yu JG, Ma H, Wang DX , et al. Expert opinions on penehyclidine hydrochloride administration for peri-operative airway management. J Clin Anesthesiol 2015; 31(6):621-3. Chinese. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|