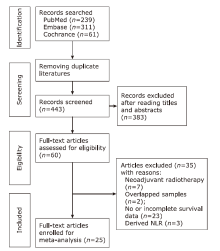
Chinese Medical Sciences Journal ›› 2020, Vol. 35 ›› Issue (3): 262-271.doi: 10.24920/003668
• Original Article • Previous Articles Next Articles
Value of Preoperative Neutrophil-to-Lymphocyte Ratio in Predicting Prognosis of Surgically Resectable Urinary Cancers: Systematic Review and Meta-Analysis
Wang Zhan, Wang Xu, Wang Wenda, Zheng Guoyang, Guo Hao, Zhang Yushi( )
)
- Department of Urology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
-
Received:2020-01-08Published:2020-09-30Online:2020-09-25 -
Contact:Zhang Yushi E-mail:beijingzhangyushi@126.com
Cite this article
Wang Zhan, Wang Xu, Wang Wenda, Zheng Guoyang, Guo Hao, Zhang Yushi. Value of Preoperative Neutrophil-to-Lymphocyte Ratio in Predicting Prognosis of Surgically Resectable Urinary Cancers: Systematic Review and Meta-Analysis[J].Chinese Medical Sciences Journal, 2020, 35(3): 262-271.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Characteristics of all the studies included in our meta-analysis"
| Author | Year | Country | Tumor type | No. of Patients | Age (yrs) | Gender (M:F) | Cut-off value | Follow-up (months) | Outcomes | Analysis type |
|---|---|---|---|---|---|---|---|---|---|---|
| Son et al.[ | 2018 | Korea | UTUC | 1137 | 69 (61-74)* | 825:312 | 3.3 | 39.1 (18.3-63.8)* | RFS, CSS | UV, MV |
| Azuma et al.[ | 2013 | Japan | UTUC | 137 | 69.4 (40-88) | 106:31 | 2.5 | 60.9 (1.9-187.3) | RFS, CSS | UV, MV |
| Kohada et al.[ | 2018 | Japan | UTUC | 148 | 71 (64-78)* | 112:36 | 3 | 35.5 (12-66)* | RFS, CSS | UV, MV |
| Tanaka et al.[ | 2014 | Japan | UTUC | 665 | 70 (62-76)* | 493:172 | 3 | 28 (14-57)* | RFS, CSS | UV, MV |
| Cao et al.[ | 2017 | China | UTUC | 656 | 68 (39-88) | 290:366 | 2.4 | 46 (12-144) | IVRFS, CSS | UV, MV |
| Cheng et al.[ | 2016 | China | UTUC | 195 | 68±10.3 | 79:116 | 2.7 | 36 | OS, CSS | UV, MV |
| Luo et al.[ | 2014 | China | UTUC | 234 | N | 102:132 | 3 | 40.7±23.8 | MFS, CSS | UV, MV |
| Tan et al.[ | 2018 | China | UTUC | 717 | 67 (59-74)* | 408:309 | 2.5 | 42 (18-76)* | OS, DFS, CSS, MFS | MV |
| Dalpiaz et al.[ | 2014 | Austria | UTUC | 202 | 69.3 (32-85) | 122:80 | 2.7 | 45 (0-199) | CSS, OS | UV, MV |
| Vartolomei et al.[ | 2017 | Austria | UTUC | 2274 | 69 (61-76) | 1527:747 | 2.7 | 40 (20-76) | RFS, CSS | UV, MV |
| Byun et al.[ | 2016 | Korea | RCC | 1284 | 55.9±12.9 | 913:371 | 3.7 | 39 (19-69)* | RFS, CSS | MV |
| Widz et al.[ | 2020 | Poland | RCC | 196 | 61 (24-85)* | 116:80 | 2.69 | 68 (44.5-78) | OS | UV, MV |
| Agizamhann et al.[ | 2018 | China | RCC | 82 | 37 (2-71) | 33:49 | 2.45 | 31 (2-108) | OS, DFS | UV, MV |
| Chen et al.[ | 2019 | China | RCC | 414 | 56.3 (24-80) | 257:157 | 2.17 | 69.2 (1-151) | OS, CSS | MV |
| Wen et al.[ | 2015 | China | RCC | 327 | 56 (3-86) | 211:116 | 1.7 | 43 (0-97) | OS, DFS | UV, MV |
| Hu et al.[ | 2017 | China | RCC | 484 | 56 (21-81) | 278:206 | 2.78 | 36 | OS | UV, MV |
| Gu et al.[ | 2016 | China | RCC | 103 | 56 (16-79) | 71:32 | 4.1 | 19.9 (10.8-35.1)* | OS | UV, MV |
| Pichler et al.[ | 2013 | Austria | RCC | 678 | N | N | 3.3 | 44 (0-130) | OS, CSS | UV, MV |
| Jang et al.[ | 2016 | Korea | Pca | 2067 | 66 (61-70) | N | 1.76 | 78 (65-6)* | BCRFS, CSS, OS | UV, MV |
| Sun et al.[ | 2018 | China | Pca | 226 | N | N | 2.31 | 24 (1-73) | OS, DFS | UV, MV |
| Viers et al.[ | 2014 | USA | Bca | 899 | 69 (62-76)* | 723:176 | 2.7 | 130.8 (99.6-166.8)* | DFS, CSS, OS | UV, MV |
| Tan et al.[ | 2017 | Singapore | Bca | 84 | 67 (37-82) | 63:21 | 2.7 | 30.1 (3.2-161.7) | DFS, OS | UV, MV |
| Kang et al.[ | 2017 | Korea | Bca | 1551 | 65 (57-72)* | 1302:249 | 2 | 52 (27-82)* | OS | UV, MV |
| Rajwa et al.[ | 2018 | Poland | Bca | 144 | N | N | 3 | 14 (7-40)* | OS, CSS | UV, MV |
| Vartolomei et al.[ | 2018 | Italy | Bca | 1046 | 70 (29-91) | 864:182 | 3 | 26 (10-47)* | OS, DFS, CSS | MV |
Table 2
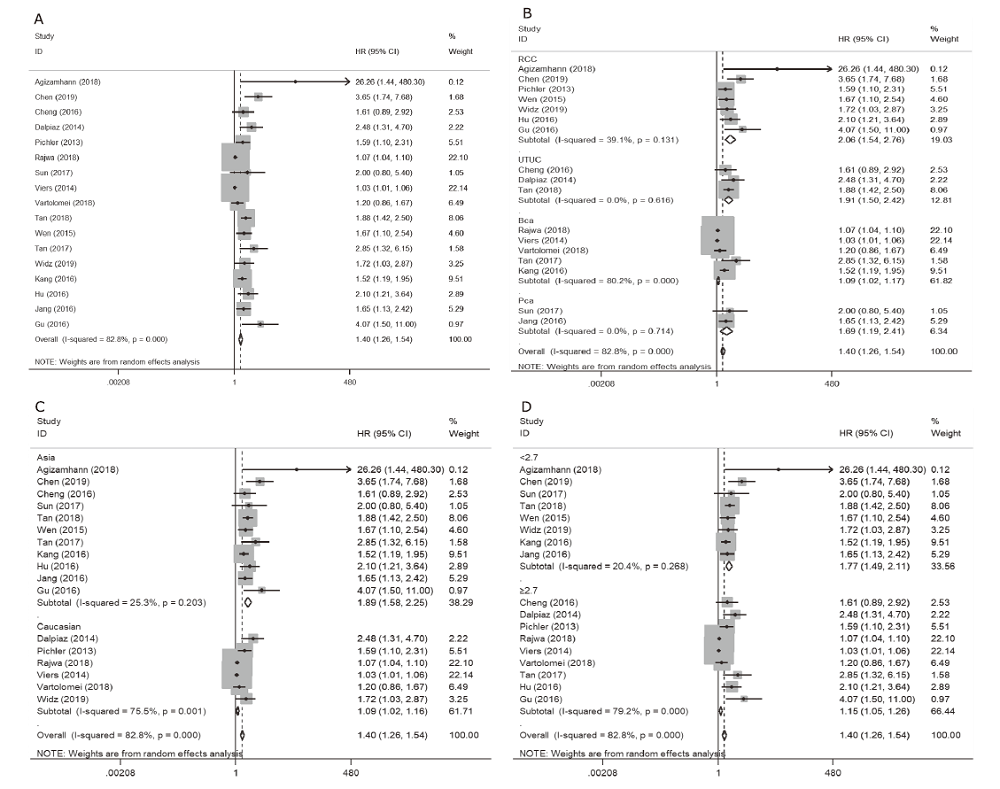
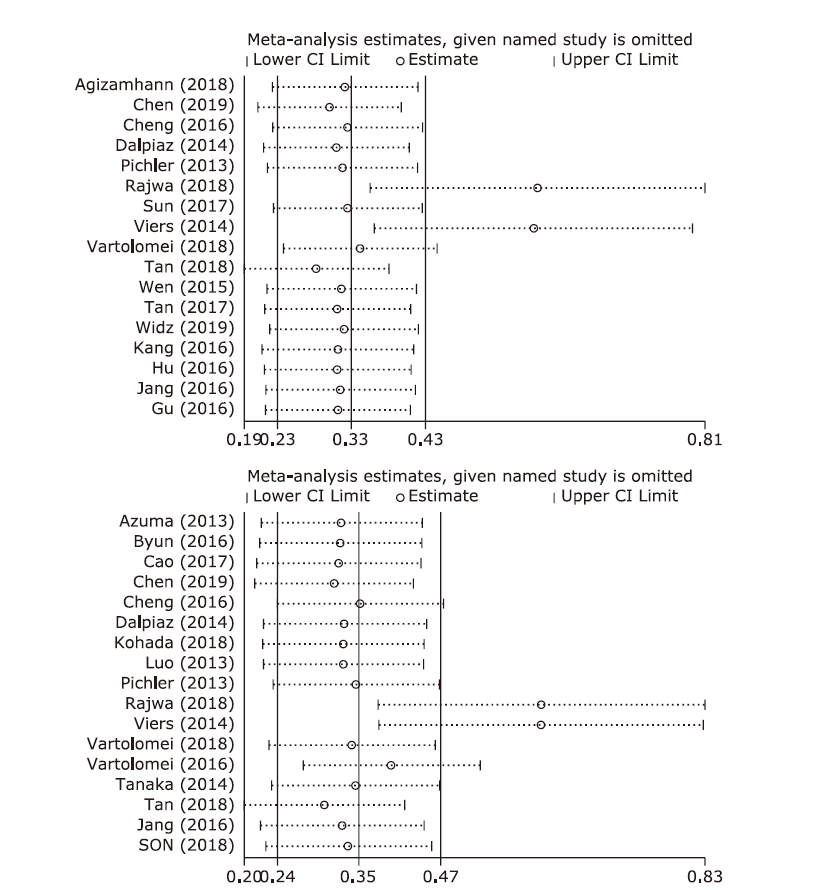
Subgroup analysis of all included articles regarding OS"
| Subgroups | No. of studies | No. of patients | HR | 95%CI | Pheterogeneity |
|---|---|---|---|---|---|
| Tumor type | |||||
| RCC | 7 | 2284 | 2.06 | 1.54-2.76 | 0.131 |
| UTUC | 3 | 1114 | 1.91 | 1.50-2.42 | 0.616 |
| Bca | 5 | 3724 | 1.09 | 1.02-1.17 | <0.001 |
| Pca | 2 | 2293 | 1.69 | 1.19-2.41 | 0.714 |
| Ethnicity | |||||
| Asian | 11 | 3165 | 1.89 | 1.58-2.25 | 0.203 |
| Caucasian | 6 | 6250 | 1.09 | 1.02-1.16 | 0.001 |
| Cut-off value | |||||
| < 2.7 | 8 | 5580 | 1.77 | 1.49-2.11 | 0.268 |
| ≥2.7 | 9 | 3835 | 1.15 | 1.05-1.26 | <0.001 |
| Overall | 17 | 9415 | 1.40 | 1.26-1.54 | <0.001 |
Table 3
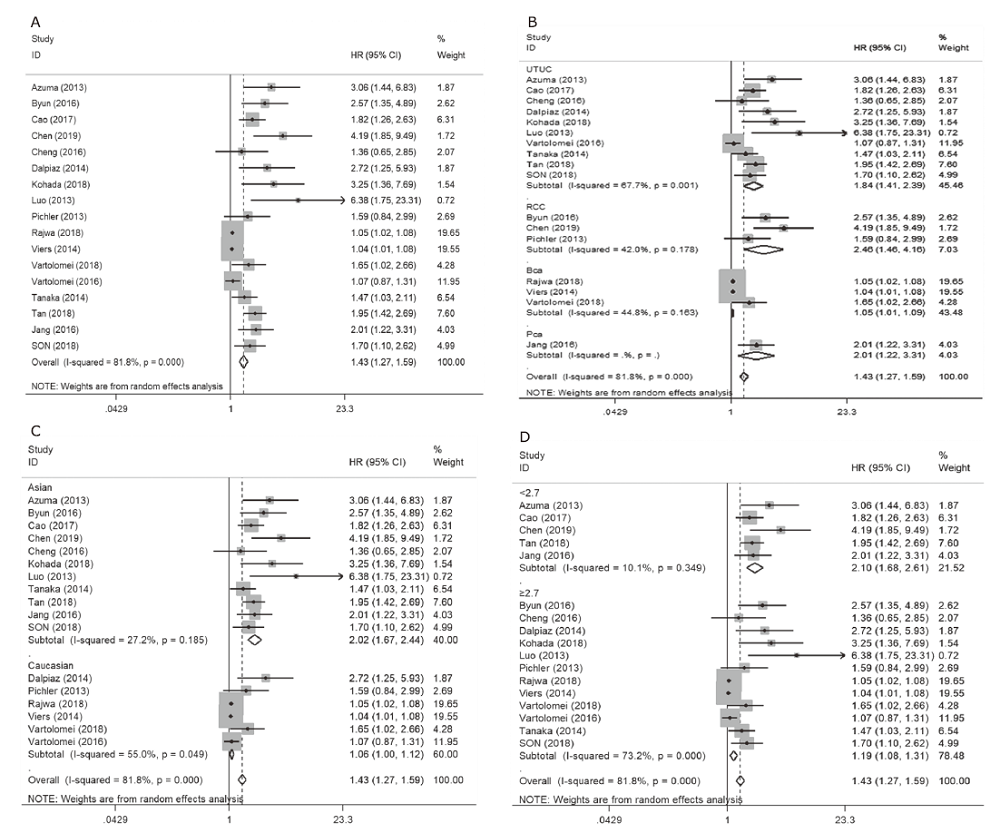
Subgroup analysis of all included articles regarding CSS"
| Subgroups | No. of studies | No. of patients | HR | 95%CI | Pheterogeneity |
|---|---|---|---|---|---|
| Tumor type | |||||
| RCC | 3 | 2376 | 2.46 | 1.46-4.16 | 0.178 |
| UTUC | 10 | 6365 | 1.84 | 1.41-2.39 | 0.001 |
| Bca | 3 | 2089 | 1.05 | 1.01-1.09 | 0.163 |
| Pca | 1 | 2067 | * | * | * |
| Ethnicity | |||||
| Asian | 11 | 7654 | 2.02 | 1.67-2.44 | 0.185 |
| Caucasian | 6 | 5243 | 1.06 | 1.00-1.12 | 0.049 |
| Cut-off value | |||||
| < 2.7 | 5 | 3991 | 2.10 | 1.68-2.61 | 0.349 |
| ≥2.7 | 12 | 8906 | 1.19 | 1.08-1.31 | <0.001 |
| Overall | 17 | 12897 | 1.43 | 1.27-1.59 | <0.001 |
| 1. |
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019; 69(1):7-34. doi: 10.3322/caac.21551.
doi: 10.3322/caac.21551 pmid: 30620402 |
| 2. |
Widz D, Mitura P, Buraczynski P, et al. Preoperative neutrophil-lymphocyte ratio as a predictor of overall survival in patients with localized renal cell carcinoma. Urol J 2020; 17(1):30-5. doi: 10.22037/uj.v0i0.4541.
doi: 10.22037/uj.v0i0.4541 pmid: 31087321 |
| 3. |
Jang WS, Cho KS, Kim KH, et al. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio after radical prostatectomy in localized prostate cancer. Prostate Cancer Prostatic Dis 2016; 19(3):298-304. doi: 10.1038/pcan.2016.20.
doi: 10.1038/pcan.2016.20 pmid: 27349499 |
| 4. |
Kang M, Jeong CW, Kwak C, et al. Preoperative neutrophil-lymphocyte ratio can significantly predict mortality outcomes in patients with non-muscle invasive bladder cancer undergoing transurethral resection of bladder tumor. Oncotarget 2017; 8(8):12891-901. doi: 10.18632/oncotarget.14179.
pmid: 28039452 |
| 5. |
Chen Z, Wang K, Lu H, et al. Systemic inflammation response index predicts prognosis in patients with clear cell renal cell carcinoma: a propensity score-matched analysis. Cancer Manag Res 2019; 11:909-19. doi: 10.2147/CMAR.S186976.
pmid: 30697081 |
| 6. |
Vartolomei MD, Ferro M, Cantiello F, et al. Validation of neutrophil-to-lymphocyte ratio in a multi-institutional cohort of patients with T1G3 non-muscle-invasive bladder cancer. Clin Genitourin Cancer 2018; 16(6):445-52. doi: 10.1016/j.clgc.2018.07.003.
doi: 10.1016/j.clgc.2018.07.003 pmid: 30077463 |
| 7. |
Tan P, Xu H, Liu L, et al. The prognostic value of preoperative neutrophil-to-lymphocyte ratio in patients with upper tract urothelial carcinoma. Clin Chim Acta 2018; 485:26-32. doi: 10.1016/j.cca.2018.06.019.
pmid: 29908941 |
| 8. |
Sun Z, Ju Y, Han F, et al. Clinical implications of pretreatment inflammatory biomarkers as independent prognostic indicators in prostate cancer. J Clin Lab Anal 2018; 32(3):e22277. doi: 10.1002/jcla.22277.
doi: 10.1002/jcla.2018.32.issue-3 |
| 9. |
Son S, Hwang EC, Jung SI, et al. Prognostic value of preoperative systemic inflammation markers in localized upper tract urothelial cell carcinoma: a large, multicenter cohort analysis. Minerva Urol Nefrol 2018; 70(3):300-9. doi: 10.23736/s0393-2249.18.02914-4.
doi: 10.23736/S0393-2249.18.02914-4 pmid: 29381018 |
| 10. |
Rajwa P, ?yczkowski M, Paradysz A, et al. Evaluation of the prognostic value of LMR, PLR, NLR, and dNLR in urothelial bladder cancer patients treated with radical cystectomy. Eur Rev Med Pharmacol Sci 2018; 22(10):3027-37. doi: 10.26355/eurrev_201805_15060.
doi: 10.26355/eurrev_201805_15060 pmid: 29863247 |
| 11. |
Kohada Y, Hayashi T, Goto K, et al. Preoperative risk classification using neutrophil-lymphocyte ratio and hydronephrosis for upper tract urothelial carcinoma. Jpn J Clin Oncol 2018; 48(9):841-50. doi: 10.1093/jjco/hyy084.
pmid: 30085174 |
| 12. |
Agizamhan S, Qu F, Liu N, et al. Preoperative neutrophil-to-lymphocyte ratio predicts the surgical outcome of Xp11.2 translocation/TFE3 renal cell carcinoma patients. BMC Urol 2018; 18(1):60. doi: 10.1186/s12894-018-0374-z.
doi: 10.1186/s12894-018-0374-z pmid: 29890986 |
| 13. |
Vartolomei MD, Mathieu R, Margulis V, et al. Promising role of preoperative neutrophil-to-lymphocyte ratio in patients treated with radical nephroureterectomy. World J Urol 2017; 35(1):121-30. doi: 10.1007/s00345-016-1848-9.
doi: 10.1007/s00345-016-1848-9 pmid: 27209168 |
| 14. |
Tan YG, Eu E, Lau Kam On W, et al. Pretreatment neutrophil-to-lymphocyte ratio predicts worse survival outcomes and advanced tumor staging in patients undergoing radical cystectomy for bladder cancer. Asian J Urol 2017; 4(4):239-46. doi: 10.1016/j.ajur.2017.01.004.
doi: 10.1016/j.ajur.2017.01.004 pmid: 29387556 |
| 15. |
Hu H, Yao X, Xie X, et al. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol 2017; 35(2):261-70. doi: 10.1007/s00345-016-1864-9.
doi: 10.1007/s00345-016-1864-9 pmid: 27255479 |
| 16. | Cao ZP, Guan B, Zhao GZ, et al. Validation of the pretreatment neutrophil-to-lymphocyte ratio as a prognostic factor in a large cohort of Chinese patients with upper tract urothelial carcinoma. Chin Med J (Engl) 2017; 130(17):2063-8. doi: 10.4103/0366-6999.213414. |
| 17. |
Gu L, Ma X, Li H, et al. Prognostic value of preoperative inflammatory response biomarkers in patients with sarcomatoid renal cell carcinoma and the establishment of a nomogram. Sci Rep 2016; 6:23846. doi: 10.1038/srep23846.
doi: 10.1038/srep23846 pmid: 27035802 |
| 18. |
Cheng YC, Huang CN, Wu WJ, et al. The prognostic significance of inflammation-associated blood cell markers in patients with upper tract urothelial carcinoma. Ann Surg Oncol 2016; 23(1):343-51. doi: 10.1245/s10434-015-4781-z.
doi: 10.1245/s10434-015-4781-z pmid: 26242371 |
| 19. |
Byun SS, Hwang EC, Kang SH, et al. Prognostic significance of preoperative neutrophil-to-Lymphocyte ratio in nonmetastatic renal cell carcinoma: a large, multicenter cohort analysis. Biomed Res Int 2016; 2016:5634148. doi: 10.1155/2016/5634148.
doi: 10.1155/2016/5634148 pmid: 27891517 |
| 20. |
Wen RM, Zhang YJ, Ma S, et al. Preoperative neutrophil to lymphocyte ratio as a prognostic factor in patients with non-metastatic renal cell carcinoma. Asian Pac J Cancer Prev 2015; 16(9):3703-8. doi: 10.7314/apjcp.2015.16.9.3703.
pmid: 25987025 |
| 21. |
Tanaka N, Kikuchi E, Kanao K, et al. A multi-institutional validation of the prognostic value of the neutrophil-to-lymphocyte ratio for upper tract urothelial carcinoma treated with radical nephroureterectomy. Ann Surg Oncol 2014; 21(12):4041-8. doi: 10.1245/s10434-014-3830-3.
pmid: 24912614 |
| 22. |
Luo HL, Chen YT, Chuang YC, et al. Subclassification of upper urinary tract urothelial carcinoma by the neutrophil-to-lymphocyte ratio (NLR) improves prediction of oncological outcome. BJU Int 2014; 113(5b):E144-9. doi: 10.1111/bju.12582.
doi: 10.1111/bju.12582 pmid: 24274691 |
| 23. |
Dalpiaz O, Ehrlich GC, Mannweiler S, et al. Validation of pretreatment neutrophil-lymphocyte ratio as a prognostic factor in a European cohort of patients with upper tract urothelial carcinoma. BJU Int 2014; 114(3):334-9. doi: 10.1111/bju.12441.
doi: 10.1111/bju.12441 |
| 24. |
Pichler M, Hutterer GC, Stoeckigt C, et al. Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer 2013; 108(4):901-7. doi: 10.1038/bjc.2013.28.
pmid: 23385728 |
| 25. |
Azuma T, Matayoshi Y, Odani K, et al. Preoperative neutrophil-lymphocyte ratio as an independent prognostic marker for patients with upper urinary tract urothelial carcinoma. Clin Genitourin Cancer 2013; 11(3):337-41. doi: 10.1016/j.clgc.2013.04.003.
doi: 10.1016/j.clgc.2013.04.003 pmid: 23665132 |
| 26. |
Viers BR, Boorjian SA, Frank I, et al. Pretreatment neutrophil-to-lymphocyte ratio is associated with advanced pathologic tumor stage and increased cancer-specific mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy. Eur Urol 2014; 66(6):1157-64. doi: 10.1016/j.eururo.2014.02.042.
doi: 10.1016/j.eururo.2014.02.042 |
| 27. |
Cho H, Hur HW, Kim SW, et al. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother 2009; 58(1):15-23. doi: 10.1007/s00262-008-0516-3.
doi: 10.1007/s00262-008-0516-3 pmid: 18414853 |
| 28. |
Fondevila C, Metges JP, Fuster J, et al. p53 and VEGF expression are independent predictors of tumour recurrence and survival following curative resection of gastric cancer. Br J Cancer 2004; 90(1):206-15. doi: 10.1038/sj.bjc.6601455.
doi: 10.1038/sj.bjc.6601455 pmid: 14710231 |
| 29. |
Hwang GI, Yoo CH, Sohn BH, et al. Predictive value of preoperative serum CEA, CA19-9 and CA125 levels for peritoneal metastasis in patients with gastric carcinoma. Cancer Res Treat 2004; 36(3):178-81. doi: 10.4143/crt.2004.36.3.178.
doi: 10.4143/crt.2004.36.3.178 pmid: 20396541 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|