Chinese Medical Sciences Journal ›› 2021, Vol. 36 ›› Issue (1): 17-26.doi: 10.24920/003866
• Original Article • Previous Articles Next Articles
Association Analysis of Hyperlipidemia with the 28-Day All-Cause Mortality of COVID-19 in Hospitalized Patients
Bin Wu1, Jianghua Zhou1, 2, Wenxin Wang1, 2, Huilin Yang2, 3, Meng Xia2, Binghong Zhang4, Zhigang She1, 2, Hongliang Li1, 2, 3, 5, *( )
)
- 1Department of Cardiology, Renmin Hospital of Wuhan University, Wuhan 430071, China
2Institute of Model Animal, Wuhan University, Wuhan 430071, China
3Basic Medical School, Wuhan University, Wuhan 430071, China
4Department of Neonatology, Renmin Hospital of Wuhan University, Wuhan 430072, China
5Medical Science Research Center, Zhongnan Hospital of Wuhan University, Wuhan 430071, China
-
Received:2021-02-09Accepted:2021-03-05Published:2021-03-17Online:2021-03-17 -
Contact:Hongliang Li E-mail:lihl@whu.edu.cn
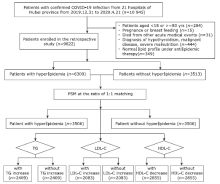
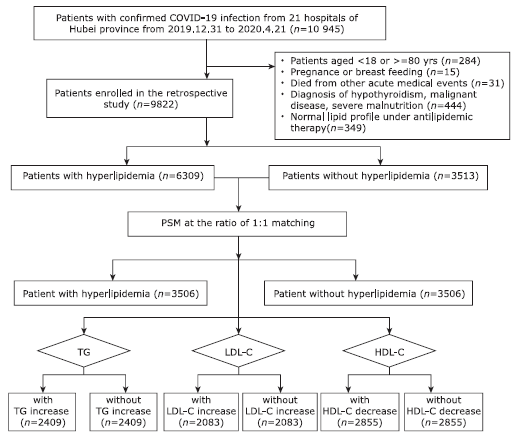
| In a cohort of 10 945 hospitalized patients with COVID-19 from Hubei Province, China, Wu et al. found that hyperlipidemia was not significantly associated with an increased risk of 28-day all-cause COVID-19 mortality. This association remained non-significant even in the subgroup analyses on patients with cardiovascular diseases or diabetes. They also found that none of the specific lipid parameters, including TG, LDL-C, and HDL-C, was significantly correlated with 28-day all-cause mortality in this COVID-19 cohort. |
Cite this article
Bin Wu,Jianghua Zhou,Wenxin Wang,Huilin Yang,Meng Xia,Binghong Zhang,Zhigang She,Hongliang Li. Association Analysis of Hyperlipidemia with the 28-Day All-Cause Mortality of COVID-19 in Hospitalized Patients[J].Chinese Medical Sciences Journal, 2021, 36(1): 17-26.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Baseline characteristics of the study cohort before and after matching"
| Characteristics | Study cohort | Cohort after matching (1:1)b | |||||
|---|---|---|---|---|---|---|---|
| Hyperlipidemia a (n=6309) | Normal (n=3513) | SD | Hyperlipidemia a (n=3506) | Normal (n=3506) | SD | ||
| Age [years, median (IQR)] | 59(48-68) | 59(45-68) | 0.083 | 58(47-67) | 59(45-68) | -0.001 | |
| Gender-male [n (%)] | 3387(53.69) | 1450(41.28) | 0.250 | 1597(45.55) | 1450(41.36) | 0.085 | |
| Heart rate [bpm, median (IQR)] | 85(78-97) | 84(78-96) | 0.049 | 85(78-96) | 84(78-96) | 0.005 | |
| Respiratory [bpm, median(IQR)] | 20(19-21) | 20(19-21) | 0.104 | 20(19-21) | 20(19-21) | -0.018 | |
| SBP [mmHg, median (IQR)] | 129(120-141) | 128(118-139) | 0.087 | 128(119-140) | 128(118-139) | 0.025 | |
| DBP [mmHg, median (IQR)] | 80(72-88) | 79(72-86) | 0.101 | 79(72-87) | 79(72-86) | 0.038 | |
| SpO2 [%, median(IQR)] | 97(95-98) | 97(96-98) | -0.06 | 98(96-98) | 97(96-98) | 0.024 | |
| Comorbidities on admission [n (%)] | |||||||
| Chronic obstructive pulmonary disease | 67(1.06) | 47(1.34) | -0.025 | 45(1.28) | 45(1.28) | 0.000 | |
| Diabetes | 1095(17.36) | 408(11.61) | 0.164 | 386(11.01) | 408(11.64) | -0.020 | |
| Heart failure | 40(0.63) | 23(0.65) | -0.003 | 20(0.57) | 23(0.66) | -0.011 | |
| Coronary heart disease | 603(9.56) | 195(5.55) | 0.152 | 204(5.82) | 195(5.56) | 0.011 | |
| Cerebrovascular diseases | 196(3.11) | 81(2.31) | 0.049 | 89(2.54) | 81(2.31) | 0.015 | |
| Chronic liver disease | 151(2.39) | 76(2.16) | 0.015 | 75(2.14) | 76(2.17) | -0.002 | |
| Chronic renal diseases | 266(4.22) | 103(2.93) | 0.002 | 112(3.19) | 103(2.94) | 0.015 | |
| Medications [n (%)] | |||||||
| Insulin | 975(15.45) | 320(9.11) | 0.194 | 332(9.47) | 320(9.13) | 0.012 | |
| Oral hypoglycemic drugs | 1352(21.43) | 456(12.98) | 0.225 | 474(13.52) | 456(13.01) | 0.015 | |
| non-ACEI/ARB antihypertensive drug | 1907(30.23) | 873(24.85) | 0.121 | 814(23.22) | 872(24.87) | -0.039 | |
| ACEI/ARB | 628(9.95) | 233(6.63) | 0.121 | 215(6.13) | 233(6.65) | -0.021 | |
| Antiplatelet | 533(8.45) | 110(3.13) | 0.229 | 89(2.54) | 110(3.14) | -0.036 | |
| Chest CT on admission [n (%)] | |||||||
| Bilateral lesions | 5154(87.05) | 2808(83.60) | 0.098 | 2718(83.35) | 2807(83.74) | -0.011 | |
| Lab tests on admission [n (%), or median(IQR)] | |||||||
| Leukocyte count > 9.5×109/L | 697(11.08) | 270(7.71) | 0.116 | 313(8.98) | 270(7.73) | 0.045 | |
| Neutrophil count > 6.3×109/L | 1062(16.89) | 412(11.77) | 0.146 | 455(13.05) | 412(11.80) | 0.038 | |
| Lymphocyte< 1.1×109/L | 2595(41.26) | 1400(40.00) | 0.026 | 1405(40.28) | 1394(39.91) | 0.008 | |
| RBC < 3.5×1012/L (female) or 4.0×1012/L (male) | 2568(40.83) | 1579(45.14) | -0.087 | 1441(41.32) | 1574(45.09) | -0.076 | |
| CRP > ULN c | 2103(52.65) | 821(46.10) | 0.131 | 1257(51.52) | 819(46.11) | 0.108 | |
| PCT > ULN c | 2479(45.06) | 1021(34.95) | 0.207 | 954(31.39) | 1020(34.99) | -0.076 | |
| ALT > 40 U/L | 1679(26.63) | 640(18.23) | 0.202 | 611(17.45) | 640(18.27) | -0.021 | |
| eGFR value (mL/min) | 103.57 (87.61-120.50) | 105.30 (89.21-122.61) | -0.073 | 107.34 (91.14-125.22) | 105.29 (89.21-122.55) | 0.043 | |
| D-dimer > ULN c | 3024(52.06) | 1351(42.26) | 0.197 | 1479(46.88) | 1351(42.32) | 0.092 | |
| cTnI > ULN c | 446(10.96) | 160(7.35) | 0.125 | 153(7.65) | 160(7.36) | 0.013 | |
Table 2
The association of hyperlipidemia with risk of 28-day all-cause mortality in total, male, and female patients with COVID-19 after propensity score matching at 1:1 ratio"
| Categories | Number of patients (n) | Deaths (n) | Adjusted HR (95% CI) | P value a |
|---|---|---|---|---|
| All patients of matched cohort b | ||||
| Hyperlipidemia group vs. non-hyperlipidemia group | 3506 vs. 3506 | 231 vs. 193 | 1.17 (0.95, 1.44) | 0.151 |
| TG ≥1.7 mmol/L group vs. TG<1.7 mmol/L group | 2409 vs. 2409 | 180 vs. 137 | 1.23 (0.98, 1.55) | 0.075 |
| LDL-C ≥3 mmol/L group vs. LDL-C<3 mmol/L group | 2083 vs. 2083 | 67 vs. 95 | 0.78 (0.57, 1.07) | 0.123 |
| HDL-C <1.0 mmol/L group vs. HDL-C ≥1.0 mmol/L group | 2855 vs. 2855 | 213 vs. 157 | 1.12 (0.90, 1.39) | 0.299 |
| Male patients in matched cohort c | ||||
| Hyperlipidemia group vs. non-hyperlipidemia group | 1449 vs. 1449 | 135 vs. 112 | 1.24 (0.91, 1.70) | 0.176 |
| TG ≥1.7 mmol/L group vs. TG<1.7 mmol/L group | 1145 vs. 1145 | 114 vs. 81 | 1.23 (0.92, 1.66) | 0.170 |
| LDL-C ≥3 mmol/L group vs. LDL-C<3 mmol/L group | 988 vs. 988 | 43 vs. 46 | 1.00 (0.65, 1.52) | 0.983 |
| HDL-C <1.0 mmol/L group vs. HDL-C ≥1.0 mmol/L group | 1499 vs. 1499 | 131 vs. 86 | 1.27 (0.94, 1.72) | 0.113 |
| Female patients in matched cohort d | ||||
| Hyperlipidemia group vs. non-hyperlipidemia group | 2014 vs. 2014 | 92 vs. 81 | 0.91 (0.66, 1.25) | 0.547 |
| TG ≥1.7 mmol/L group vs. TG<1.7 mmol/L group | 1233 vs. 1233 | 62 vs. 50 | 1.14 (0.78, 1.66) | 0.509 |
| LDL-C ≥3 mmol/L group vs. LDL-C<3 mmol/L group | 1099 vs. 1099 | 24 vs. 33 | 0.82 (0.48, 1.39) | 0.456 |
| HDL-C <1.0 mmol/L group vs. HDL-C ≥1.0 mmol/L group | 1326 vs. 1326 | 79 vs. 66 | 1.00 (0.71, 1.40) | 0.993 |
Table 3
The association of hyperlipidemia with risk of 28-day all-cause mortality among COVID-19 patients with CVDs and type 2 diabetes after propensity score matching at ratio of 1:1."
| Categories | Number of Patients (n) | Deaths (n) | Adjusted HR (95% CI) | P value a |
|---|---|---|---|---|
| Cardiovascular diseases b | ||||
| Hyperlipidemia group vs. non-hyperlipidemia group | 1242 vs. 1242 | 128 vs. 114 | 0.96 (0.73,1.26) | 0.765 |
| TG ≥1.7 mmol/L group vs. TG<1.7 mmol/L group | 1004 vs. 1004 | 115 vs. 81 | 1.19 (0.88,1.60) | 0.253 |
| LDL-C ≥3 mmol/L group vs. LDL-C<3 mmol/L group | 814 vs. 814 | 42 vs. 59 | 0.78 (0.52,1.17) | 0.235 |
| HDL-C <1.0 mmol/L group vs. HDL-C ≥1.0 mmol/L group | 1131 vs. 1131 | 124 vs. 90 | 1.00 (0.75,1.33) | 0.991 |
| Type 2 diabetes c | ||||
| Hyperlipidemia group vs. non-hyperlipidemia group | 473 vs. 473 | 52 vs. 54 | 0.74 (0.49,1.13) | 0.164 |
| TG ≥1.7 mmol/L group vs. TG<1.7 mmol/L group | 515 vs. 515 | 56 vs. 40 | 1.07 (0.70,1.64) | 0.752 |
| LDL-C ≥3 mmol/L group vs. LDL-C<3 mmol/L group | 364 vs. 364 | 20 vs. 29 | 0.72 (0.40,1.30) | 0.279 |
| HDL-C <1.0 mmol/L group vs. HDL-C ≥1.0 mmol/L group | 492 vs. 492 | 56 vs. 43 | 1.17 (0.76,1.81) | 0.468 |
| 1. |
Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin Ⅱ receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020; 126(12):1671-81. doi: 10.1161/CIRCRESAHA.120.317134.
doi: 10.1161/CIRCRESAHA.120.317134 pmid: 32302265 |
| 2. |
Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 2020;31(6):1068-77.e3. doi: 10.1016/j.cmet.2020.04.021.
doi: 10.1016/j.cmet.2020.04.021 pmid: 32369736 |
| 3. |
Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; 5(7):811-8. doi: 10.1001/jamacardio.2020.1017.
doi: 10.1001/jamacardio.2020.1017 pmid: 32219356 |
| 4. |
Bornstein SR, Rubino F, Khunti K, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol 2020; 8(6):546-50. doi: 10.1016/S2213-8587(20)30152-2.
doi: 10.1016/S2213-8587(20)30152-2 pmid: 32334646 |
| 5. | Ni WQ, Liu XL, Zhuo ZP, et al. Serum lipids and associated factors of dyslipidemia in the adult population in Shenzhen. Lipids Health Dis 2015; 14(1):1-11. doi: 10.1186/s12944-015-0073-7. |
| 6. |
Palaiodimos L, Kokkinidis DG, Li W, et al. Severe obesity is associated with higher in-hospital mortality in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020; 108:154262. doi: 10.1016/j.metabol.2020.154262.
doi: 10.1016/j.metabol.2020.154262 pmid: 32422233 |
| 7. | Abu-Farha M, Thanaraj TA, Qaddoumi MG, et al. The role of lipid metabolism in COVID-19 virus infection and as a drug target. Int J Mol Sci 2020; 21(10):3544. doi: 10.3390/ijms21103544. |
| 8. |
Tanaka S, Labreuche J, Drumez E, et al. Low HDL levels in sepsis versus trauma patients in intensive care unit. Ann Intensive Care 2017; 7(1):4-11. doi: 10.1186/s13613-017-0284-3.
doi: 10.1186/s13613-016-0231-8 pmid: 28050897 |
| 9. | Peñarrubia L, Ruiz M, Porco R, et al. Multiple assays in a real-time RT-PCR SARS-CoV-2 panel can mitigate the risk of loss of sensitivity by new genomic variants during the COVID-19 outbreak. Int J Infect Dis 2020; 97:225-9. doi: 10.1016/j.ijid.2020.06.027. |
| 10. | Official website of the National Health Commission of People’s Republic of China. The prevention and control guideline for novel coronavirus pneumonia (5th edition). . |
| 11. | Joint committee issued Chinese guideline for the management of dyslipidemia. 2016 Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2016; 44(10):833-53. Chinese. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005. |
| 12. |
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis 2019; 290:140-205. doi: 10.1016/j.atherosclerosis.2019.08.014.
doi: 10.1016/j.atherosclerosis.2019.08.014 pmid: 31591002 |
| 13. | Chinese Diabetes Society; National Office for Primary Diabetes Care. National guidelines for the prevention and control of diabetes in primary care( 2018). Zhonghua nei ke za zhi 2018; 57(12):885-93. Chinese. doi: 10.3760/cma.j.issn.0578-1426.2018.12.003. |
| 14. | Jakubowski KP, Cundiff JM, Matthews KA. Cumulative childhood adversity and adult cardiometabolic disease: A meta-analysis. Heal Psychol 2018; 37(8):701-15. doi: 10.1037/hea0000637. |
| 15. | Tay MZ, Poh CM, Rénia L, et al. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 2020; 20(6):363-74. doi: 10.1038/s41577-020-0311-8. |
| 16. |
Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol 2020; 20(5):269-70. doi: 10.1038/s41577-020-0308-3.
pmid: 32273594 |
| 17. | Touyz RM, Li H, Delles C. ACE2 the Janus-faced protein-from cardiovascular protection to severe acute respiratory syndrome-coronavirus and COVID-19. Clin Sci 2020; 134(7):747-50. doi: 10.1042/CS20200363. |
| 18. | Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020; 368(m1091):1-14. doi: 10.1136/bmj.m1091. |
| 19. |
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA 2020; 323(20):2052-9. doi: 10.1001/jama.2020.6775.
pmid: 32320003 |
| 20. |
Shao B, Heinecke JW. HDL, lipid peroxidation, and atherosclerosis. J Lipid Res 2009; 50(4):599-601. doi: 10.1194/jlr.E900001-JLR200.
doi: 10.1194/jlr.E900001-JLR200 pmid: 19141435 |
| 21. |
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352(16):1685-95. doi: 10.1056/NEJMra043430.
pmid: 15843671 |
| 22. |
Steinberg D. An interpretive history of the cholesterol controversy, part III: Mechanistically defining the role of hyperlipidemia. J Lipid Res 2005; 46(10):2037-51. doi: 10.1194/jlr.R500010-JLR200.
doi: 10.1194/jlr.R500010-JLR200 pmid: 15995167 |
| 23. |
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395(10229):1054-62. doi: 10.1016/S0140-6736(20)30566-3.
doi: 10.1016/S0140-6736(20)30566-3 pmid: 32171076 |
| 24. |
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8(5):475-81. doi: 10.1016/S2213-2600(20)30079-5.
doi: 10.1016/S2213-2600(20)30079-5 pmid: 32105632 |
| 25. | Criner GJ, Connett JE, Aaron SD, et al. Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. N Engl J Med 2014; 370(23):2201-10. doi: 10.1056/nejmoa1403086. |
| 26. |
Truwit JD, Bernard GR, Steingrub J, et al. Rosuvastatin for sepsis-associated acute respiratory distress syndrome. N Engl J Med 2014; 370(23):2191-200. doi: 10.1056/NEJMoa1401520.
doi: 10.1056/NEJMoa1401520 pmid: 24835849 |
| 27. | Zhang XJ, Qin JJ, Cheng X, et al. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab 2020; 32(2):176- 87. e4. doi: 10.1016/j.cmet.2020.06.015. |
| 28. | Liu G, Zhang S, Mao Z, et al. Clinical significance of nutritional risk screening for older adult patients with COVID-19. Eur J Clin Nutr 2020; 74(6):876-83. doi: 10.1038/s41430-020-0659-7. |
| 29. |
Deniz O, Gumus S, Yaman H, et al. Serum total cholesterol, HDL-C and LDL-C concentrations significantly correlate with the radiological extent of disease and the degree of smear positivity in patients with pulmonary tuberculosis. Clin Biochem 2007; 40(3-4):162-6. doi: 10.1016/j.clinbiochem.2006.10.015.
doi: 10.1016/j.clinbiochem.2006.10.015 pmid: 17217941 |
| 30. | Ishiyama Y, Gallagher PE, Averill DB, et al. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin Ⅱ receptors. Hypertension 2004; 43(5):970-6. doi: 10.1161/01.HYP.0000124667.34652.1a. |
| 31. | Dijkman R, Jebbink MF, Deijs M, et al. Replication-dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63. J Gen Virol 2012; 93(Pt 9):1924-9. doi: 10.1099/vir.0.043919-0. |
| 32. | Putnam K, Shoemaker R, Yiannikouris F, et al. The renin-angiotensin system: A target of and contributor to dyslipidemias, altered glucose homeostasis, and hypertension of the metabolic syndrome. Am J |
| Physiol Hear Circ Physiol 2012; 302(6):H1219-30. doi: 10.1152/ajpheart.00796.2011. | |
| 33. |
Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet 2019; 393(10170):407-15. doi: 10.1016/S0140-6736(18)31942-1.
pmid: 30712900 |
| 34. |
Lemmers RFH, van Hoek M, Lieverse AG, et al. The anti-inflammatory function of high-density lipoprotein in type II diabetes: A systematic review. J Clin Lipidol 2017; 11(3):712-24. doi: 10.1016/j.jacl.2017.03.
doi: 10.1016/j.jacl.2017.03.013 pmid: 28442299 |
|
013.
doi: 10.1016/j.jacl.2017.03.013 pmid: 28442299 |
|
| 35. | Hui N, Barter PJ, Ong KL, et al. Altered HDL metabolism in metabolic disorders: Insights into the therapeutic potential of HDL. Clin Sci 2019; 133(21):2221-35. doi: 10.1042/CS20190873. |
| 36. |
Wei X, Zeng W, Su J, et al. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol 2020; 14(3):297-304. doi: 10.1016/j.jacl.2020.04.008.
doi: 10.1016/j.jacl.2020.04.008 pmid: 32430154 |
| 37. | Guirgis FW, Donnelly JP, Dodani S, et al. Cholesterol levels and long-term rates of community-acquired sepsis. Crit Care 2016; 20(1):1-12. doi: 10.1186/s13054-016-1579-8. |
| 38. | Cirstea M, Walley KR, Russell JA, et al. Decreased high-density lipoprotein cholesterol level is an early prognostic marker for organ dysfunction and death in patients with suspected sepsis. J Crit Care 2017; 38:289-94. doi: 10.1016/j.jcrc.2016.11.041. |
| [1] | Yu Gu,Ting Zhang,Min Peng,Juhong Shi. Characteristics and Prognosis of Microscopic Polyangiitis Patients with Diffuse Alveolar Hemorrhage and Interstitial Lung Disease [J]. Chinese Medical Sciences Journal, 2022, 37(4): 293-302. |
| [2] | Zihan Chen, Zhou Zhao, Chuiwen Deng, Naishi Li. Association between Air Pollution and Type 2 Diabetes Mellitus in Developing Countries: A Systematic Review and Meta-Analysis [J]. Chinese Medical Sciences Journal, 2022, 37(3): 218-227. |
| [3] | Tieli Li, Haixuan Ding, Xinlan Zhao, Juan Luo, Kai Chen, Zhuo Tang, Lingyun Huang, Langbo Li, Li Yang. A Case Report of MODY3 Combined with Intestinal Neuroendocrine Tumor [J]. Chinese Medical Sciences Journal, 2022, 37(2): 167-170. |
| [4] | Kunrong Wu, Shufang Zhang, Ziwan Guan, Xiaoli Li, Rui Li, Ying Yin, Yan Li. Methylenetetrahydrofolate Reductase Gene Polymorphism C677T is Associated with Increased Risk of Coronary Heart Disease in Chinese Type 2 Diabetic Patients [J]. Chinese Medical Sciences Journal, 2021, 36(2): 103-109. |
| [5] | Honglin Zu,Likun Hou,Hongwei Liu,Yuanbo Zhan,Ju He. Identify Candidate Genes in the Interaction between Abdominal Aortic Aneurysm and Type 2 Diabetes Mellitus by Using Biomedical Discovery Support System [J]. Chinese Medical Sciences Journal, 2021, 36(1): 50-56. |
| [6] | Lin Ye, Wang Zhenlian, Yan Min, Zhu Feiyu, Duan Ye, Sun Zhiqin. Effect of Trimetazidine on Diabetic Patients with Coronary Heart Diseases: A Meta-Analysis of Randomized, Controlled Trials [J]. Chinese Medical Sciences Journal, 2020, 35(3): 226-238. |
| [7] | Zhu Weihua,Xie Wenyong,Zhang Zhedong,Li Shu,Zhang Dafang,Liu Yijun,Zhu Jiye,Leng Xisheng. Postoperative Complications and Survival Analysis of Surgical Resection for Hilar Cholangiocarcinoma: A Retrospective Study of Fifty-Nine Consecutive Patients [J]. Chinese Medical Sciences Journal, 2020, 35(2): 157-169. |
| [8] | Yin Ying, Li Rui, Li Xiaoli, Wu Kunrong, Li Ling, Xu Yuedong, Liao Lin, Yang Rui, Li Yan. Association Between Homocysteine Level and Methylenetetrahydrofolate Reductase Gene Polymorphisms in Type 2 Diabetes Accompanied by Dyslipidemia [J]. Chinese Medical Sciences Journal, 2020, 35(1): 85-91. |
| [9] | Chen Qiang, Zhang Liwei, Huang Dangsheng, Zhang Chunhong, Wang Qiushuang, Shen Dong, Xiong Minjun, Yang Feifei. Five-year Clinical Outcomes of CAD Patients Complicated with Diabetes after StentBoost-optimized Percutaneous Coronary Intervention [J]. Chinese Medical Sciences Journal, 2019, 34(3): 177-183. |
| [10] | Dai Yulan,Zhu Chengzhang,Shan Xi,Cheng Zhenzhen,Zou Beiji. A Survey on Intelligent Screening for Diabetic Retinopathy [J]. Chinese Medical Sciences Journal, 2019, 34(2): 120-132. |
| [11] | Chen Zhiye, Zang Xiujuan, Liu Mengqi, Liu Mengyu, Li Jinfeng, Gu Zhaoyan, Ma Lin. Abnormal Alterations of Cortical Thickness in 16 Patients with Type 2 Diabetes Mellitus: A Pilot MRI Study△ [J]. Chinese Medical Sciences Journal, 2017, 32(2): 75-82. |
| [12] | Du Junhui, Li Rong. Can Fundus Fluorescein Angiography be Performed for Diabetic Patients on Oral Metformin?△ [J]. Chinese Medical Sciences Journal, 2017, 32(2): 119-122. |
| [13] | Yang Yingying, Pan Hui, Wang Bo, Chen Shi, Zhu Huijuan. Efficacy and Safety of SGLT2 Inhibitors in Patients with Type 1 Diabetes: A Meta-analysis of Randomized Controlled Trials [J]. Chinese Medical Sciences Journal, 2017, 32(1): 22-27. |
| [14] | Jing Yang, Mei-cen Zhou, Kai Feng, Ou Wang, Hua-bing Zhang, Wei Li, Fan Ping, Jing Yang, Yu-xiu Li. Clinical Characteristics of 261 Cases of Hospitalized Patients with Type 1 Diabetes Mellitus [J]. Chinese Medical Sciences Journal, 2016, 31(2): 69-75. |
| [15] | Ying Fan, Shan-xiao Zhang, Meng Ren, Li-feng Hong, Xiao-ni Yan. Impact of 1, 25-(OH)2D3 on Left Ventricular Hypertrophy in Type 2 Diabetic Rats [J]. Chinese Medical Sciences Journal, 2015, 30(2): 114-120. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|