CEREBRAL venous sinus thrombosis (CVST) is a rare and life-threatening condition, accounting for about 0.5-1% of all strokes.1 It usually occurs in infant, young adults, and female, especially during late pregnancy and puerpe-rium, and relatively rare in early pregnancy. The expe-rience in management of such patient is limited according to the literatures available by far. Here, we present a pregnant woman requesting induced abortion who was diagnosed as CVST in the first trimester, recovered after anticoagulation therapy, and succeeded in induction of labor in the second trimester without any complication.
CASE DESCRIPTION
A 22-year-old Chinese woman, gravida 1 para 0 at 10 weeks of pregnancy, was admitted to the Family Planning ward for a request of induced abortion as she was unmarried. Three days after admission, she suffered from continuous severe headache, accompanying with nausea and vomiting. She had no other symptoms, such as abdominal pain, vaginal bleeding, fever, rash, seizure or diplopia. The headache progressed in severity the next day. The patient recalled her migraine headache occurred every summer since she was 14-year-old, but the headache was mild and automatically resolved in several days, only occasionally gastrodia was applied to relieve the pain. The patient declined any personal history of cerebral trauma, other medical diseases, and family history of similar condition.
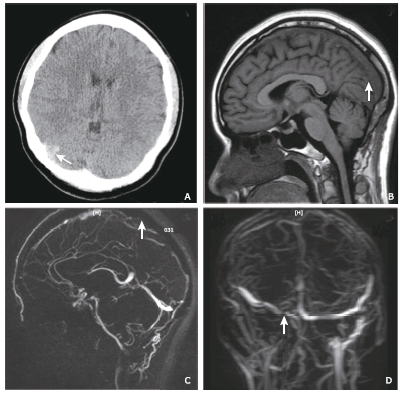
The vital signs were stable at admission. Phy-sical examination showed a stiff neck without focal neurological findings. Blood examinations excluded connective tissue diseases and infectious diseases. Anticardiolipin antibodies in serum by enzyme-linked immunosorbent assay were negative. The d-dimer was abnormally elevated to 5.01 mg/L, but her coagulation profile was normal. The general screening of thrombo- philia including protein C and protein S revealed a decreased level of protein S. Homocysteine in serum was normal. Cerebral CT showed a high intensity in the right parietal lobe (Fig. 1A). Magnetic resonance image (MRI) revealed an iso-signal intensity lesion on T1-weighted image (T1WI) (Fig. 1B) and a hypo-signal intensity lesion on T2-weighted image (T2WI) in superior sagittal sinus. Magnetic Resonance veno- graphy (MRV) showed that the superior sagittal sinus, right transverse sinus were completely occluded (Fig. 1C, 1D). Magnetic Resonance Angiography (MRA) did not show any abnormity.
Figure 1.
Medical imaging of cerebral venous sinus thrombosis of a young lady in early pregnancy.
A. Non-contrast CT image showed high density (arrow) in the area of right parietal lobe, which was suspicious for thrombosis; B. Sagittal T1WI MRI image revealed an iso-signal intensity (arrow) in superior sagittal sinus; C. Sagittal image of reconstructed MRV, a thrombus filling defect in superior sagittal sinus (arrow) was observed; D. Coronal image of reconstructed MRV, a thrombus filling defect in right transverse sinus (arrow) was observed.
The patient was diagnosed as cerebral venous sinus thrombosis after consulting with the neurology team and was transferred to the neurological ward. To control intracranial hypertension, mannitol was administrated intravenously and low molecular weight heparin (LMWH) subcutaneously with dose adjusted by her weight soon after admitted. One week after the initiation of the treatment, warfarin was added orally. The dose of warfarin was strictly adjusted according to her International Normalized Ratio (INR), targeted between 2.0 to 3.0. In the third week of anticoagulation treatment, the INR reached the targeted level. The headache started to resolve gradually. Then we stopped LMWH and only warfarin was given orally.
Post-treatment CT scan one month after the diagnosis showed the cerebral venous sinus thrombosis had disappeared. As the patients requested induced abortion, she was then transferred to the Family Planning ward again. Considering the possibility of hemorrhage during induction of labor, warfarin was replaced by LMWH. The ultrasound examination of uterus demonstrated a pregnancy at about 14-week gestation. Amniocentesis was performed and rivanol, also known as ethacridine which was a type of disinfectant, was injected into her amniotic cavity. Two days later, the patient spontaneously delivered a lifeless fetus and the placenta was delivered by vaginal with no complication. She was informed to take warfarin for 3 months after induction of labor.
DISCUSSION
CVST is an abnormal condition with a variaty of symptoms and signs, affecting about 5 people per million.1 It may lead to many emergent or life-threatening situations, such as cerebral edema, cerebral hemorrhage, hernia of brain, so early diagnosis and early therapy is crucial.
The underlying risk factors of CVST include prothrombotic conditions, hyperhomocysteinemia, pregnancy and puerperium, positive antiphospholipid antibodies, protein C and protein S deficiency, oral contraceptives, cancer, preeclampsia, etc.2 In contrast to other subtypes of stroke, the incidence of CVST decreases with age.3,4 CVST is more common seen in young adult, and pregnancy related CVST occurs in the third trimester or puerperium because of the hypercoagulation state. Besides, hypercoagulability may worsen by anemia, dehydration, preeclampsia and trauma.5 The case we present was in early pregnancy, which was a rare type. The mechanisms of CVST during pregnancy and postpartum are still unclear. A cross-section study showed that women with pregnant associated stroke had fewer vascular risk factors but were more likely to have cerebral venous thrombosis than non-pregnant women with stroke, which indicated CVST may have a unique pathophysiology related to pregnancy.6
Clinical manifestations of CVST are of diversity and depend on the location and severity of thrombosis. Because of its non-specific symptoms, it is difficult to distinguish from other diseases such as hypertension, intracranial infection, and cranial space occupying lesions. Many data have shown that headache is the most common symptom clinically, no matter with or without any other compliant.7,8 Other common signs are nausea, vomiting, blurred vision, focal neurological deficits, seizures and disturbance of consciousness. During early pregnancy, the prodromal symptom of CVST, such as nausea and vomiting, may be misdiagnosed as hyperemesis gravidarum. Imaging can reveal the occluded vessels and thrombus in cerebral veins or sinus, so it plays an important role in diagnosis of CVST. MRI/MRV, CT/CTV, and angiography are commonly used. The typical manifestation on CT for CVST, “the empty delta sign”, usually presents 7 to 10 days after symptoms onset, while it is usually normal or non-specific in up to 30% CVST cases, and CT venography is suggestive.2,4 MRI is noninvasive, more sensitive and specific compared with CT scan. The MRI signal varies with not only the localization of involved vessel or sinus, but also with aging of the thrombus. In the first 3 to 5 days, the thrombus shows isointense on T1WI and hypointense on T2WI. Then its signals increase on both T1WI and T2WI with time going on. The golden standard for CVST is the combined visualization of thrombosed vessel or sinus on MRI and absence of the vessel or sinus on MRV.2,4 Studies have demonstrated that MRI during pregnancy has no harm to the fetus.9 Therefore, MRI and MRV are recommended as the first choice of imaging examination for screening of CVST in pregnant patients. Intra-artery angiography is currently rarely performed because it’s invasive. In our case, CT, MRI, MRV and MRA were performed timely, all of which helped to make a quick and standing diagnosis of CVST.
According to the guideline of the American Heart Association/American Stroke Association, once CVST is diagnosed, anticoagulant therapy should be initiated if no major contraindications.2 The first line treatment for CVST in acute phase usually start with intravenous heparin or subcutaneous LMWH. It has been supposed that anticoagulation treatment is beneficial to prevent enlargement of thrombosis, decrease the incidence of pulmonary embolism, and promote the recanalization.2 There has been no evidence showing the treatment of anticoagulation for CVST with intracerebral hemorrhage increase the risk of bleeding.8,10 However, follow-up imaging is needed to exclude intracerebral hemorrhage during anticoagulant therapy.
The experience in the treatment for pregnant women with CVST is limited, and all data are from case reports or small sample size studies. Heparin or LMWH could be used in full dose throughout the pregnancy till delivering, because of their feature not being transferred into placenta. The dose of heparin needs to be adjusted between 3000 U to 5000 U, while the dose of LMWH be adjusted by patients’ body-weight.11,12 There is no data on the difference of outcomes between heparin and LWMH in CVST patients.
The time of using oral anticoagulation postpartum depends on the underlying etiology of CVST. For CVST patients who have transient risk factor, such as pregnancy while using oral contraceptive, warfarin should be continued for 3 to 6 months. For CVST patients related to inherited prothrombotic condition, warfarin should be continued for 6 to 12 months or indefinitely.2,13 It was recommended to continue the anticoagulation for at least 6 weeks postpartum, accompanied with oral warfarin or other vitamin k antagonist to keep a target INR between 2.0 to 3.0.10,12,13 Nonetheless, warfarin is forbidden in first trimester of pregnancy for its teratogenic effects. In this case, we gave anticoagulation therapy with combination of LMWH and warfarin. When her condition became steady, she was continually put on oral warfarin for 3 months due to the transient risk of pregnancy.
Some small cases series suggested that endovascular thrombolysis, no matter mechanical or chemical, may be safe and efficient for CVST patients who was on anticoagulation but got worse. Local injection of recombinant tissue plasminogen activator (rtPA) or urokinase was used successfully in recanalization in some case studies.14,15 Some CVST patients with severe headache and papilledema may have increased intracranial pressure (ICP), which can be reduced by diuretics and osmotherapy. If syndromes of ICP significantly progress, such as herniation, decompressive surgery should be considered as a life-saving procedure.16 There are evidences showing that CVST alone, pregnancy-related or puerperium-related CVST are not a contraindication for future pregnancies.1,17
In conclusion, CVST, although rare, can occur in early pregnancy. The clinical manifestations are divers and non-specific. MRI and MRV are recommended for a suspected CVST in pregnancy. Anticoagulation treatment with heparin or LMWH is safe and efficient for pregnant patients. CVST in early pregnant patients may have a good prognosis.
Consent
Written informed consent was obtained from the patient for publishing this case report.
Conflict of interests statement
The authors declared no conflict of interests.
参考文献
Cerebral venous thrombosis: an update
Cerebral venous thrombosis (CVT) is a rare type of cerebrovascular disease that can occur at any age, including in neonates, and it accounts for 0~5% of all stroke. The widespread use of neuroimaging now allows for early diagnosis and has completely modified our knowledge on this disorder. CVT is more common than previously thought and it is recognised as a non-septic disorder with a wide spectrum of clinical presentations, numerous causes, and usually a favourable outcome with a low mortality rate. MRI with T1, T2, fluid-attenuated inversion recovery, and T2* sequences combined with magnetic resonance angiography are the best diagnostic methods. D-dimer concentrations are raised in most patients but normal D-dimers do not rule out CVT, particularly in patients who present with isolated headache. Heparin is the first-line treatment, but in a few cases more aggressive treatments, such as local intravenous thrombolysis, mechanical thrombectomy, and decompressive hemicraniectomy, may be required.
American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Diagnosis and management of cerebral venous thrombosis. A statement for healthcare professionals from the American Heart Association/American Stroke Association
Cerebral venous thrombosis (CVT) is an uncommon cause of stroke that mainly affects young adults and children. In contrast to venous thromboembolism, women are affected three times more often than men. Baseline symptoms can vary considerably between patients, but most present with headache, seizures, or focal neurological deficits. Patients can be diagnosed with magnetic resonance imaging,... [Show full abstract]
Risk of pregnancy-associated stroke across age groups in New York state
Abstract Importance: Older age is associated with increased risk of pregnancy-associated stroke (PAS). Data are limited on age-specific incidence ratios of PAS compared with stroke risk in nonpregnant women. Objectives: To assess the risk of stroke by age group in pregnant and postpartum women compared with their nonpregnant contemporaries and to compare risk factors across age groups in the exposed (pregnant/postpartum) and unexposed (nonpregnant) populations. Design, Setting, and Participants: International Classification of Diseases, Ninth Revision, billing codes from the calendar year 2003-2012 New York State Department of Health inpatient database and population data were used to identify all women aged 12 to 55 years with cerebrovascular events, including transient ischemic attack, ischemic and hemorrhagic stroke, cerebral venous thrombosis, and nonspecified PAS. The cumulative incidence of PAS per 100090004000 pregnant/postpartum women vs nonpregnancy-associated stroke (NPAS) per 100090004000 women in age cohorts of 24 years or younger, 25 to 34, 35 to 44, and 45 years or older was calculated. Risk factors between groups were compared using logistic regression models. The study included data from calendar years 2003 through 2012. Data analysis was performed from July 11, 2015, to July 16, 2016. Exposures: Pregnancy, including the postpartum period up to 6 weeks after delivery. Main Outcomes and Measures: Incidence risk ratios (IRRs) for stroke per age cohort, defined as cumulative risk of stroke in the exposed population divided by cumulative risk of stroke in the unexposed population, were determined, and stroke risk factors and mortality were compared between populations. Results: There were 19090004146 women hospitalized with stroke during the study period; 797 of the women were pregnant/post partum. The overall median (interquartile range) age of the women was 31 (25-35) years in those with PAS and 48 (41-52) years in those with NPAS. The incidence of PAS in women aged 12 to 24 years was 14 events per 100090004000 pregnant/postpartum women vs NPAS incidence of 6.4 per 100090004000 nonpregnant women (IRR, 2.2; 95% CI, 1.9-2.6); for ages 25 to 34 years, 21.2 per 100090004000 vs 13.5 per 100090004000 (IRR, 1.6; 95% CI, 1.4-1.7); for ages 35 to 44 years, 33 per 100090004000 vs 31 per 100090004000 (IRR, 1.1; 95% CI, 0.9-1.2); and for ages 45 to 55 years, 46.9 per 100090004000 vs 73.7 per 100090004000 (IRR, 0.6; 95% CI, 0.3-1.4). PAS accounted for 18% of strokes in women younger than 35 years vs 1.4% of strokes in women aged 35 to 55 years. Women in the NPAS group vs the PAS group had more vascular risk factors, including chronic hypertension (age <35 years: 437 [15.7%] vs 60 [9.8%], P090009<090009.001; age 35-55 years: 7573 [48.6%] vs 36 [19.3%], P090009<090009.001), diabetes (age <35 years: 103 [3.7%] vs 9 [1.5%], P090009=090009.002; age 35-55 years: 2618 [16.8%] vs 12 [6.4%], P090009<090009.001), and active smoking (age <35 years: 315 [11.3%] vs 29 [4.8%], P090009<090009.001; age 35-55 years: 2789 [17.9%] vs 10 [5.3%], P090009<090009.001); and had higher mortality (age <35 years: 288 [11.3%] vs 37 [6.5%], P090009<090009.001; age 35-55 years: 2121 [13.4%] vs 14 [6.1%], P090009<090009.001). Conclusions and Relevance: Younger women, but not older women, have an increased stroke risk during pregnancy and post partum compared with their nonpregnant contemporaries. These results suggest that pregnancy does not increase the risk of stroke in older women.
Aguiar de Sousa D. Cerebral venous thrombosis
A case of cerebral sinus venous thrombosis resulting in mortality in severe preeclamptic pregnant woman
Cerebral venous sinus thrombosis (CVST) is a rarely encountered condition during pregnancy. A 21-year-old pregnant woman with labour pains was hospitalized in our clinic. Diagnosis of severe preeclampsia was made based on her clinical and laboratory findings. She suffered from convulsive episodes during postpartum period which lead to initiation of treatment for eclampsia. However neurological and radiological examinations were performed after emergence of additional neurological symptoms disclosed the diagnosis of CVST. In this paper, we aimed to present a case with CVST which diagnosis was confused with eclampsia and resulting in maternal mortality.
Mechanisms and outcomes of stroke during pregnancy and the postpartum period: a cross-sectional study
Prognosis of cerebral vein and dural sinus thrombosis: results of the international study on cerebral vein and dural sinus thrombosis (ISCVT)
Cerebral venous thrombosis: a descriptive multicenter study of patients in Pakistan and Middle East
A review of the current use of magnetic resonance imaging in pregnancy and safety implications for the fetus
http://linkinghub.elsevier.com/retrieve/pii/S0079610704001130
Cerebral venous sinus thrombosis with cerebral hemorrhage during early pregnancy
Abstract Cerebral venous sinus thrombosis (CVST) rarely induces cerebral hemorrhage, and CVST with cerebral hemorrhage during early pregnancy is extremely rare. Upon literature review, we are able to find only one case of CVST with cerebral hemorrhage in early pregnancy. In this paper, we report another case of a 27-year-old patient who developed CVST with cerebral hemorrhage in her fifth week of pregnancy. Although the optimal treatment for this infrequent condition remains controversial, we adopted anticoagulation as the first choice of treatment and obtained favorable results.
Anticoagulation for cerebral venous sinus thrombosis
Cerebral venous sinus thrombosis presenting with diplopia in pregnancy: a case report
Introduction Cerebral venous sinus thrombosis is a rare condition. The most frequent symptoms and signs are headache, focal seizures with or without secondary generalization, unilateral or bilateral paresis and papilledema. We report a case of transverse sinus and superior sagittal sinus thrombosis that presented with diplopia in a pregnant woman. Case presentation A 34-year-old Malay woman, gravida 3 para 2 at 8 weeks of pregnancy, was admitted for hyperemesis gravidarum, presented with sudden onset of diplopia, blurring of vision and headache. A magnetic resonance scan of her brain showed the presence of cerebral edema with no space occupying lesion, but magnetic resonance venography ultimately revealed right transverse sinus and superior sagittal sinus thrombosis. The patient was treated with anticoagulation for 1 year, after which the patient recovered fully. Conclusion Due to its diverse and varied neurological presentation, cerebral venous sinus thrombosis should be considered in almost any brain syndrome.
Clinical and radiological management and outcome of pregnancies complicated by cerebral venous thrombosis: a review of 19 cases
Thrombolytics for cerebral sinus thrombosis: a systematic review
Intra-arterial thrombolysis of complete deep cerebral venous thrombosis
Department of Neurology, Klinikum Grosshadern, Munich, Germany.
Decompressive surgery for severe cerebral venous sinus thrombosis
Background : Cerebral venous sinus thrombosis (CVST) is one of the common causes of stroke in young people. Mortality in CVST, in addition to progressive thrombosis, is related to elevated intracranial pressure causing transtentorial herniation. The role of decompressive surgery in CVST is not well established. Aims : We report our experience with decompressive surgery in CVST and review the literature. Settings and Design : This is a retrospective study carried out in the Stroke Unit of a multispeciality tertiary care hospital in south India. Materials and Methods : The medical records of patients admitted with the diagnosis of CVST between December 2003 and July 2009 were reviewed. The clinical presentation, etiology, medical management, indications for surgery and outcomes were assessed for patients undergoing decompressive surgery. The sensorium was assessed using the Glasgow Coma Scale (GCS), while the outcome was assessed using the modified Rankin scale (mRS). Descriptive statistics were used as appropriate. Results : One hundred and six patients were admitted with the diagnosis of CVST during the study period. Eleven patients (10%) underwent decompressive surgical procedure. Indications for surgery included a low GCS at admission with large infarct on the computed tomography scan, mass effect and midline shift, clinical and radiological signs of transtentorial herniation, deterioration in the sensorium in spite of anti-edema measures and postthrombolysis hematoma. Eight patients (73%) had a good outcome while three patients (27%) died. Of the patients who died, two had a low GCS and bilaterally nonreactive pupils before the surgery while one had thrombosis of the deep venous system. Conclusion : Decompressive surgery for patients with large cerebral venous infarcts is a life-saving procedure. Patients with CVST who develop clinical and radiological features of transtentorial herniation either at presentation or during the course of medical management may benefit from decompressive surgery.<br>
Pregnancy outcome after a first episode of cerebral vein thrombosis
Abstract Background: The risk of recurrent thrombosis and bleeding episodes in women with previous cerebral vein thrombosis (CVT) on antithrombotic prophylaxis with low-molecular weight heparin (LMWH) during pregnancy is not established and little information is available on pregnancy outcome. Objectives: Aims of this study were to evaluate the risk of obstetrical complications, recurrent venous thrombosis and bleeding and in a cohort of pregnant women on LMWH after a first episode of CVT. In addition, to estimate the relative risk of obstetrical complications, patients were compared to healthy women without thrombosis and with at least one pregnancy in their life. Patients: We studied a cohort of 52 patients and 204 healthy women. Results: The risk to develop late obstetrical complications was 24% (95% CI 18%-38%), leading to a relative risk of 6.09 (95% CI 2.46-15.05). The risk of miscarriage was not increased. The higher risk of late obstetrical complications in patients appeared unrelated to a previous history of obstetrical complications, to the carriership of thrombophilia abnormalities, or to the presence of comorbidities. A double prevalence of termination was observed in patients with thrombophilia than in those without. No recurrent thrombosis nor bleeding episodes was observed. Conclusions: Women with previous CVT on LMWH prophylaxis during pregnancy have a low risk to develop recurrent thrombosis or bleeding episodes, but seems to have an increased risk of late obstetrical complications. This article is protected by copyright. All rights reserved.