Chinese Medical Sciences Journal ›› 2019, Vol. 34 ›› Issue (3): 199-204.doi: 10.24920/003489
• Original Article • Previous Articles Next Articles
IL-36β Promotes Inflammatory Activity and Inhibits Differentiation of Keratinocytes In Vitro
Wang Wenming1, Wu Chao1, Yu Xiaoling2, Jin Hongzhong1, *( )
)
- 1 Department of Dermatology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
2 Department of Dermatology, Dermatology Hospital of Southern Medical University, Guangdong Provincial Dermatology Hospital, Guangdong 510080, China
-
Received:2018-12-28Published:2019-09-30 -
Contact:Jin Hongzhong E-mail:jinhongzhong@263.net
Cite this article
Wang Wenming, Wu Chao, Yu Xiaoling, Jin Hongzhong. IL-36β Promotes Inflammatory Activity and Inhibits Differentiation of Keratinocytes In Vitro[J].Chinese Medical Sciences Journal, 2019, 34(3): 199-204.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

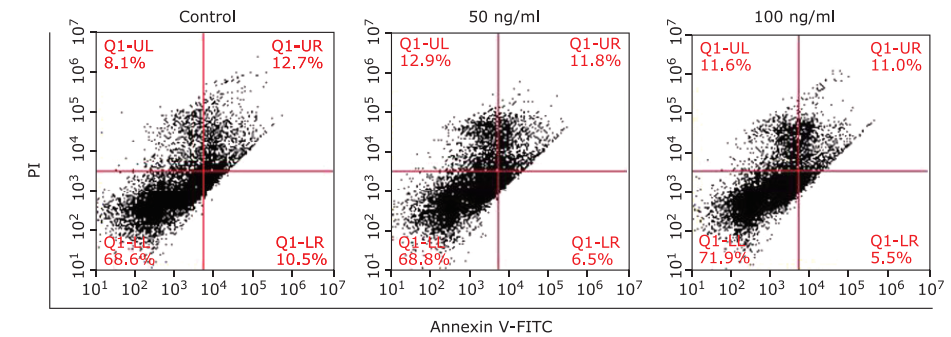
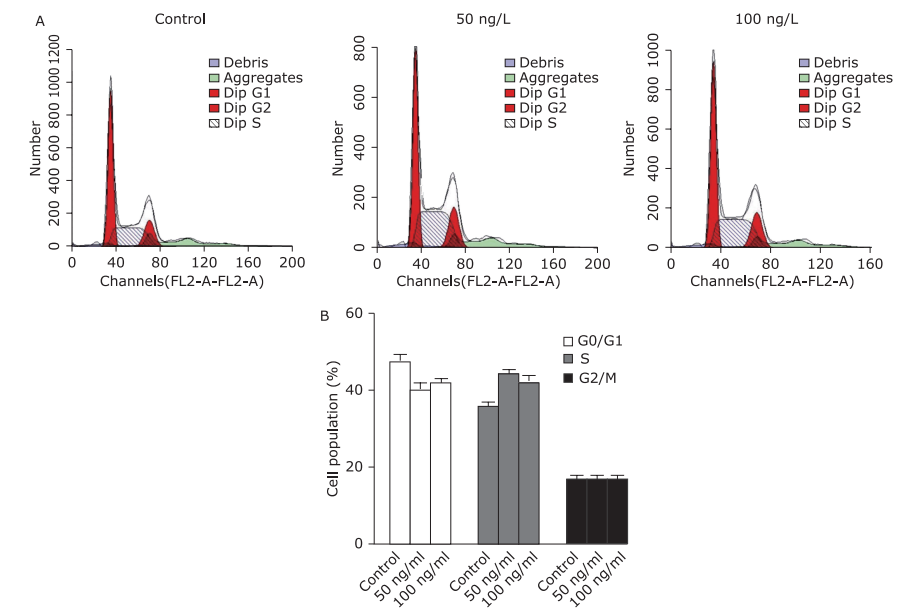
Figure 2.
Effect of IL-36β on HaCaT cell cycle. A. Representative histograms of flow cytometric analysis of HaCaT cells treated with IL-36β (0, 50 or 100 ng/ml) for 24 h. B. Results of quantitative analysis of cell cycle distribution. Data are the mean ± SEM of experiments performed in triplicate."
| 1. | Bebes A, Kovacs-Solyom F, Prihoda J , et al. Interleukin-1 receptors are differentially expressed in normal and psoriatic T cells. Mediators Inflamm 2014; 2014:472625. doi: 10.1155/2014/472625. |
| 2. | Boehncke WH, Schon MP . Psoriasis. Lancet 2015; 386(9997):983-94. doi: 10.1016/S0140-6736(14)61909-7. |
| 3. | Nestle FO, Kaplan DH, Barker J . Psoriasis. N Engl J Med 2009; 361(5):496-509. doi: 10.1056/NEJMra0804595. |
| 4. | Lowes MA, Bowcock AM, Krueger JG . Pathogenesis and therapy of psoriasis. Nature 2007; 445(7130):866-73. doi: 10.1038/nature05663. |
| 5. | Chamian F, Lowes MA, Lin SL , et al. Alefacept reduces infiltrating T cells, activated dendritic cells, and inflammatory genes in psoriasis vulgaris. Proc Natl Acad Sci U S A 2005; 102(6):2075-80. doi: 10.1073/pnas.0409569102. |
| 6. | Sticherling M . Psoriasis and autoimmunity. Autoimmun Rev 2016; 15(12):1167-70. doi: 10.1016/j.autrev.2016.09.004. |
| 7. | Sims JE, Smith DE . The IL-1 family: regulators of immunity. Nat Rev Immunol 2010; 10(2):89-102. doi: 10.1038/nri2691. |
| 8. |
Balato A, Schiattarella M, Lembo S , et al. Interleukin-1 family members are enhanced in psoriasis and suppressed by vitamin D and retinoic acid. Arch Dermatol Res 2013; 305(3):255-62. doi: 10.1007/s00403-013-1327-8.
doi: 10.1007/s00403-013-1327-8 |
| 9. | Baliwag J, Barnes DH, Johnston A . Cytokines in psoriasis. Cytokine 2015; 73(2):342-50. doi: 10.1016/j.cyto.2014.12.014. |
| 10. | Hahn M, Frey S, Hueber AJ . The novel interleukin-1 cytokine family members in inflammatory diseases. Curr Opin Rheumatol 2017; 29(2):208-13. doi: 10.1097/BOR.0000000000000361. |
| 11. | Walsh PT, Fallon PG . The emergence of the IL-36 cytokine family as novel targets for inflammatory diseases. Ann N Y Acad Sci 2018; 1417(1):23-34. doi: 10.1111/nyas.13280. |
| 12. | Balato A, Mattii M, Caiazzo G , et al. IL-36gamma is involved in psoriasis and allergic contact dermatitis. J Invest Dermatol 2016; 136(7):1520-3. doi: 10.1016/j.jid.2016.03.020. |
| 13. | Foster AM, Baliwag J, Chen CS , et al. IL-36 promotes myeloid cell infiltration, activation, and inflammatory activity in skin. J Immunol 2014; 192(12):6053-61. doi: 10.4049/jimmunol.1301481. |
| 14. | Johnston A, Xing X, Wolterink L , et al. IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis. J Allergy Clin Immunol 2017; 140(1):109-20. doi: 10.1016/j.jaci.2016.08.056. |
| 15. | Johnston A, Xing X, Guzman AM , et al. IL-1F5, -F6, -F8, and -F9: a novel IL-1 family signaling system that is active in psoriasis and promotes keratinocyte antimicrobial peptide expression. J Immunol 2011; 186(4):2613-22. doi: 10.4049/jimmunol.1003162. |
| 16. | Sehat M, Talaei R, Dadgostar E , et al. Evaluating serum levels of IL-33, IL-36, IL-37 and gene expression of IL-37 in patients with psoriasis vulgaris. Iran J Allergy Asthma Immunol 2018; 17(2):179-87. |
| 17. |
Carrier Y, Ma HL, Ramon HE , et al. Inter-regulation of Th17 cytokines and the IL-36 cytokines in vitro and in vivo: implications in psoriasis pathogenesis. J Invest Dermatol 2011; 131(12):2428-37. doi: 10.1038/jid.2011.234.
doi: 10.1038/jid.2011.234 |
| 18. | Boutet MA, Bart G, Penhoat M , et al. Distinct expression of interleukin (IL)-36alpha, beta and gamma, their antagonist IL-36Ra and IL-38 in psoriasis, rheumatoid arthritis and Crohn’s disease. Clin Exp Immunol 2016; 184(2):159-73. doi: 10.1111/cei.12761. |
| 19. | van Asseldonk EJ, Stienstra R, Koenen TB , et al. The effect of the interleukin-1 cytokine family members IL-1F6 and IL-1F8 on adipocyte differentiation. Obesity (Silver Spring) 2010; 18(11):2234-6. doi: 10.1038/oby.2010.55. |
| 20. | Magne D, Palmer G, Barton JL , et al. The new IL-1 family member IL-1F8 stimulates production of inflammatory mediators by synovial fibroblasts and articular chondrocytes. Arthritis Res Ther 2006; 8(3):R80. doi: 10.1186/ar1946. |
| 21. | Grossman RM, Krueger J, Yourish D , et al. Interleukin 6 is expressed in high levels in psoriatic skin and stimulates proliferation of cultured human keratinocytes. Proc Natl Acad Sci U S A 1989; 86(16):6367-71. doi: 10.1073/pnas.86.16.6367. |
| 22. | Tamilselvi E, Haripriya D, Hemamalini M , et al. Association of disease severity with IL-1 levels in methotrexate-treated psoriasis patients. Scand J Immunol 2013; 78(6):545-53. doi: 10.1111/sji.12117. |
| 23. | Kim TJ, Kim TH, Lee HJ , et al. Interleukin 1 polymorphisms in patients with ankylosing spondylitis in Korea. J Rheumatol 2008; 35(8):1603-8. |
| 24. | Gresnigt MS, van de Veerdonk FL . Biology of IL-36 cytokines and their role in disease. Semin Immunol 2013; 25(6):458-65. doi: 10.1016/j.smim.2013.11.003. |
| 25. | Di Caprio R, Balato A, Caiazzo G , et al. IL-36 cytokines are increased in acne and hidradenitis suppurativa. Arch Dermatol Res 2017; 309(8):673-8. doi: 10.1007/s00403-017-1769-5. |
| 26. | D’Erme AM, Wilsmann-Theis D, Wagenpfeil J , et al. IL-36gamma (IL-1F9) is a biomarker for psoriasis skin lesions. J Invest Dermatol 2015; 135(4):1025-32. doi: 10.1038/jid.2014.532. |
| 27. | Sahle FF, Gebre-Mariam T, Dobner B , et al. Skin diseases associated with the depletion of stratum corneum lipids and stratum corneum lipid substitution therapy. Skin Pharmacol Physiol 2015; 28(1):42-55. doi: 10.1159/000360009. |
| 28. |
Elsholz F, Harteneck C, Muller W , et al. Calcium—a central regulator of keratinocyte differentiation in health and disease. Eur J Dermatol 2014; 24(6):650-61. doi: 10.1684/ejd.2014.2452.
doi: 10.1684/ejd.2014.2452 |
| 29. |
Gschwandtner M, Mildner M, Mlitz V , et al. Histamine suppresses epidermal keratinocyte differentiation and impairs skin barrier function in a human skin model. Allergy 2013; 68(1):37-47. doi: 10.1111/all.12051.
doi: 10.1111/all.12051 |
| 30. |
Gutowska-Owsiak D, Ogg GS . Cytokine regulation of the epidermal barrier. Clin Exp Allergy 2013; 43(6):586-98. doi: 10.1111/cea.12023.
doi: 10.1111/cea.12023 |
| 31. | Iizuka H, Takahashi H, Honma M , et al. Unique keratinization process in psoriasis: late differentiation markers are abolished because of the premature cell death. J Dermatol 2004; 31(4):271-6. |
| 32. |
Dugu L, Nakahara T, Wu Z , et al. Neuronatin is related to keratinocyte differentiation by up-regulating involucrin. J Dermatol Sci 2014; 73(3):225-31. doi: 10.1016/j.jdermsci.2013.10.008.
doi: 10.1016/j.jdermsci.2013.10.008 |
| 33. | Kage M, Tokudome Y, Matsunaga Y , et al. Effect of hyaluronan tetrasaccharides on epidermal differentiation in normal human epidermal keratinocytes. Int J Cosmet Sci 2014; 36(1):109-15. doi: 10.1111/ics.12105. |
| 34. | Donetti E, Cornaghi L, Arnaboldi F , et al. Interleukin 22 early affects keratinocyte differentiation, but not proliferation, in a three-dimensional model of normal human skin. Exp Cell Res 2016; 345(2):247-54. doi: 10.1016/j.yexcr.2016.05.004. |
| 35. | Gelfant S . The cell cycle in psoriasis: a reappraisal. Br J Dermatol 1976; 95(6):577-90. |
| 36. | Javier AF, Bata-Csorgo Z, Ellis CN , et al. Rapamycin (sirolimus) inhibits proliferating cell nuclear antigen expression and blocks cell cycle in the G1 phase in human keratinocyte stem cells. J Clin Invest 1997; 99(9):2094-9. doi: 10.1172/JCI119382. |
| 37. | Zhang Y, Tu C, Zhang D , et al. Wnt/beta-catenin and Wnt5a/Ca pathways regulate proliferation and apoptosis of keratinocytes in psoriasis lesions. Cell Physiol Biochem 2015; 36(5):1890-902. doi: 10.1159/000430158. |
| 38. | Wrone-Smith T, Mitra RS, Thompson CB , et al. Keratinocytes derived from psoriatic plaques are resistant to apoptosis compared with normal skin. Am J Pathol 1997; 151(5):1321-9. |
| [1] | He Qiong, Wang Hui-hui, Cheng Tao, Yuan Wei-ping, Ma Yu-po, Jiang Yong-ping, Ren Zhi-hua. Genetic Correction and Hepatic Differentiation of Hemophilia B-specific Human Induced Pluripotent Stem Cells [J]. Chinese Medical Sciences Journal, 2017, 32(3): 135-144. |
| [2] | Du Tingting, Liu Na, Gu Bin, Li Ying, Yuan Yifang, Zhang Wei, Zhang Tong. Effects of Aging on the Proliferation and Differentiation Capacity of Human Periodontal Ligament Stem Cells△ [J]. Chinese Medical Sciences Journal, 2017, 32(2): 83-91. |
| [3] | Liang Wang, Zheng-yao Li, Yi-peng Wang*, Zhi-hong Wu, Bin Yu. Dynamic Expression Profiles of Marker Genes in Osteogenic Differentiation of Human Bone Marrow-derived Mesenchymal Stem Cells [J]. Chinese Medical Sciences Journal, 2015, 30(2): 108-113. |
| [4] | Yi Liu, Jian-ping Gong, Wen-fang Li. Therapeutic Effect and Safety of Ustekinumab for Plaque Psoriasis: A Meta-analysis [J]. Chinese Medical Sciences Journal, 2014, 29(3): 131-138. |
| [5] | Rui-feng Yang, Guo-wei Zhao, Shu-ting Liang, Hou-zao Chen, and De-pei Liu. Lysine-specific Demethylase 1 Represses THP-1 Monocyte-to-macrophage Differentiation025B3; [J]. Chinese Medical Sciences Journal, 2013, 28(2): 82-87. |
| [6] | Li Zhang, Li Yan, Ye Zhang, Ning-hua Wu and Yu-fei Shen. Role of Acetylated p53 in Regulating the Expression of map2 in Retinoic Acid-induced P19 Cells [J]. Chinese Medical Sciences Journal, 2010, 25(2): 71-75. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|