AMYOTROPHIC lateral sclerosis (ALS) is a progressive neurodegenerative disease with selected upper and lower motor neuron involvement.1,2 Pathological changes in cerebral cortical regions in ALS have been demonstrated as the selective involvement of the motor cortex in a postmortem study.3However, motor neuron density measurement in cortex and spinal cord suggested that corticomotoneuron loss was unlikely to be a primary event in ALS.4 More and more researchers have recognized that ALS may be a multisystem disease.2,5
Voxel-based morphometry (VBM)6 is widely used to investigate brain structure changes at voxel-level over the whole brain, and it has been widely used in evaluation of ALS patients. VBM studies demonstrated that the volume of grey matter decreased in ALS,7 and primary sensorimotor cortex atrophy was regarded as a prominent feature of the disease.8 A meta-analysis9,10 demonstrated that the asymmetric motor cortex atrophy was the main cerebral changes in ALS, but the pathophysiological mechanism has not been completely elucidated by far.
Cortical thickness measurement is an important research project for neuroimaging, and it can provide more valuable information than volume measurement in evaluation of neurodegenerative and psychological diseases. Like VBM technique, surface-based morphometry(SBM)11,12 is also a whole brain structure analysis technique, and it can provide objective and accurate information in cortical thickness changes. SBM has been widely used in clinical researches on Huntington disease,13 Parkinson’s disease,14 aging brain,15 etc. Previous studies16-18 demonstrated that motor cortex thinning was associated with ALS, and a SBM study19 suggested that the motor cortex thinning might reflect upper motor neuron impairment, whereas the extra-motor involvement may be related to the disability, progression, and duration of the disease. It has gradually come into a consensus that motor cortex atrophy is a common finding for the central nervous system damage in ALS.
Our previous voxel-wise meta-analysis of VBM study suggested that right precentral gray matter atrophy was a common finding and prominent feature of brain structural changes in ALS.12 Further VBM study in ALS subtypes demonstrated that the pattern of gray matter damage is likely to distribute wider in spinal-onset ALS than in bulbar-onset ALS.20 However, the precise cortical thinning pattern has not been elucidated in different onset subtypes of ALS. Herein, we hypothesized that some brain regions would intrinsically be suffered from cortical thinning in ALS, and different ALS subtypes (ALS-bulbar and ALS-spinal) present different cortical thinning pattern.
MATERIALS AND METHODS
Participants and study design
The study was approved by the institutional ethics committee, and written informed consents were obtained from all participants. Sixty-five patients (28 females and 37 males) were recruited from the outpatient clinic for motor neuron disease (MND) in our hospital from 2007 to 2010, including 34 diagnosed ALS cases and 31 probable ALS cases according to the revised El Escorial.21 All the subjects were right handed and had no history of cerebrovascular disease, long-standing hypertension, diabetes mellitus, inflammatory diseases of the central nervous system and cranium trauma. None of the patients were taking psychoactive drugs and hormone. Patients with brain tumors, demyelination and other brain disorders were also excluded by conventional MRI examinations. Sixty-five normal controls (NCs) were recruited from volunteers of hospital staff and local community in the same time period with the same exclusion criteria. ALS functional rating scale-revise (ALSFRS-R)22 was administered to all the patients for clinical rating of ALS symptoms,and the Mini Mental State Examination23 was applied by a dedicated neurologist with 15-years’ experience to evaluate the cognitive function of all subjects.
MRI acquisition
Image data of all patients and controls were acquired on a GE 3.0T MRI system (SIGNA EXCITE, GE Healthcare, Milwaukee, WI, USA). and a conventional eight channel quadrature head coil was used. A 3-dimensional T1-weighted fast spoiled gradient recalled echo (3D T1-FSPGR) sequence generating 118 contiguous axial slices [TR (repetition time)=6.3 ms, TE (echo time)=2.8 ms, flip angle=15°, FOV (field of view)=
24 cm×24 cm, Matrix=256×256, voxel size=0.9375×
0.9375×1 mm3, NEX (number of acquisition)=1] was used for structural images. Conventional T2-weighted image (TR=5000 ms, TE=113.4 ms, FOV=24 cm×24 cm, Matrix=384×384) and T1-FLAIR (TR=2040 ms, TE=6.9 ms, FOV=24 cm×24 cm, Matrix=384×192) were also acquired. The image protocol was identical for each subject.
Image data processing
All MR structural image data were processed on workstation of MATLAB 7.6 (The Mathworks, Natick, MA, USA) for VBM using Statistical Parametric Mapping 12 (SPM 12) and CAT12 tools (http://www.fil.ion.ucl.ac.uk/spm/). The following processing steps were carried out (Fig. 1): (1) The artifacts of raw data for each subject were inspected and image origin was set at the anterior commissure (AC); (2) structural images of each subject were normalized to the DARTEL templates space to improve inter-subject registration of structural images, and were segmented into gray matter (GM), white matter (WM) and cerebrospinal fluid (CSF); (4) projection-based thickness (PBT) was used to estimate cortical thickness and to create the central cortical surface for the left and right hemisphere;24 (5) the mean cortical thickness of 152 brain regions were computed based on FreeSurfer atlas aparc.a2009s;25 (6) after the preprocessing was finished, quality check was performed to evaluate the sample homogeneity; (7) before the statistical analysis, all the surface data was smoothed using a kernel with 15 mm full width at half maximum (FWHM).
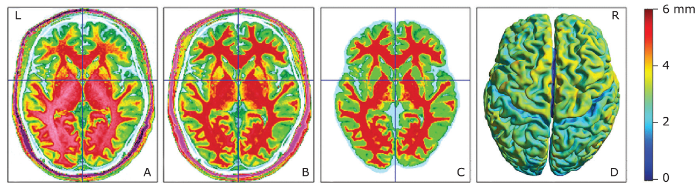
Figure 1.
The flow graph of image processing. A, original T1 image; B, normalized T1 image; C, gray and white matter segmentation; D, cortical surface creation. Color bar represents the cortical thickness.
Statistical analysis
Comparison of surface-based morphometric data between two groups was performed using two-sample t-test with age and sex as covariates. Significance was set at a P value without correction (Puncorr) of < 0.001. The minimal number of contiguous voxels was set based on the expected voxels per cluster. The quantitative data were presented as mean±standard deviation. The correlation analysis was applied between the clinical variables and the mean cortical thickness of the abnormal brain regions with age and sex as covariates. Significant difference was set at a P value of <0.05. The statistical analysis was performed using SPSS 19.0.
RESULTS
The clinical characteristics of ALS and NCs
There was no significant difference in the gender (χ2=0.03, P=0.86), but a significant difference in the age(t=1.98, P=0.002) and for MMSE (t=1.98, P=1.43) between ALS and NC group were found between the ALS patients and normal controls (Table 1). The average disease duration and ALSFRS scores for ALS patients were 17.74±21.46 days and 29.43±5.23, respectively. There was no significant difference in MMSE (t=2.00, P=0.09), diseased duration (t=2.00, P=0.50) and ALSFRS score (t=2.00, P=0.76) between ALS-bulbar and ALS-spinal patients.
Table 1 Demographic and clinical characteristics of patients and controls§
| Characteristics | ALS patients n=65 | Normal controls n=65 |
|---|---|---|
| Gender (F/M), n | 28/37 | 29/36 |
| Age,years | 49.6±10.3 | 43.5±12.2 |
| MMSE score | 27.1±2.8 | 27.5±2.3 |
| DD, months | 17.7±21.5 | |
| ALSFRS-R score | 29.4±5.2 |
§:Plus-minus values are means and standard deviation. MMSE:mini mental state examination; DD:disease duration; ALSFRS-R: ALS functional rating scale-revise.
Brain regions with altered cortical thickness in ALS, ALS-spinal, ALS-bulbar compared with NCs
Compared with that in NCs, the brain regions with decreased cortical thickness in ALS patients were locatedin the left precentral gyrus and postcentral gyrus, right gyrus rectus and medial precentral gyrus (Table 2) (Fig. 2). There was no thickening brain regions detected in ALS patients compared with NCs.
Table 2 Brain regions with cortical thinning in ALS compared with controls
| Cluster | Anatomic region | MNI-space | K value | Pvalue | tvalue | ||
|---|---|---|---|---|---|---|---|
| X | Y | Z | |||||
| ALS vs. NC | |||||||
| 1 | Left precentral gyrus | -9 | -24 | 76 | 619 | 0.000 | 4.15 |
| 2 | Left postcentral gyrus | -56 | -9 | 19 | 293 | 0.000 | 3.70 |
| 3 | Right gyrus rectus | 4 | 43 | -22 | 150 | 0.000 | 3.41 |
| 4 | Right medial precentral gyrus | 6 | -22 | 73 | 191 | 0.000 | 3.37 |
| ALS-bulbar vs. NC | |||||||
| 5 | Left precentral gyrus | -25 | -16 | 68 | 154 | 0.000 | 4.20 |
| 6 | Righ SMC | 8 | -8 | 69 | 219 | 0.000 | 4.45 |
| ALS-spinal vs. NC | |||||||
| 7 | Left posterior insula | -36 | -13 | -5 | 264 | 0.000 | 3.85 |
| 8 | Right gyrus rectus | 5 | 42 | -24 | 210 | 0.000 | 3.51 |
MNI:montreal neurological institute; SMC:supplementary motor cortex; X, Y, Z:coordinates of the primary maximum of the cluster. NC:normal control. Cluster 1 and 2 with expected 142 vertices per cluster, cluster 3 and 4 with expected 144 vertices per cluster, cluster 5 and 6 with expected 123 vertices per cluster, cluster 7 with expected 139 vertices per cluster, cluster 8 with expected 142 vertices per cluster.
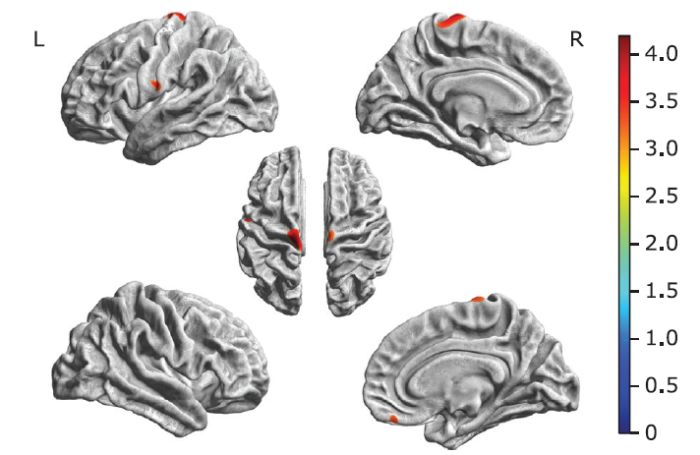
Figure 2.
Brain regions with decreased cortical thickness in ALS patients were located in the left precentral gyrus, postcentral gyrus, right gyrus rectus and medial precentral gyrus compared with NC group. Color bar represents t value.
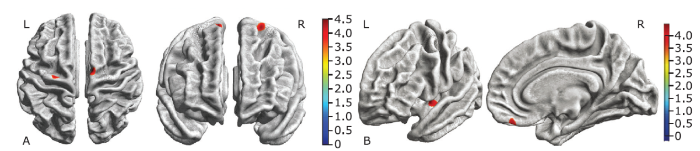
Comparing with the NC group, ALS-bulbar group presented regional thinning in the left precentral gyrus and right supplementary motor cortex (SMC), and ALS-spinal group presented regional thinning brain regions in the left posterior insular and right gyrus rectus. There was no significant difference in the cortical thickness over the whole brain between ALS-bulbar and ALS-spinal patients (Fig. 3).
Figure 3.
Brain regions with decreased cortical thickness in the ALS-bulbar patients and in the ALS-spinal patients compared with the NC group. A. Decreased cortical thickness in ALS-bulbar located in the left precentral gyrus and the right supplementary motor cortex. B. Decreased cortical thickness in the ALS-spinal located in the left posterior insula and the right gyrus rectus. Color bar represent t value.
Relationship of cortical thickness changes with clinical characteristics in ALS patients
Table 3 shows that for patients with ALS, the cortical thickness of right gyrus rectus was negatively associated with disease duration (r=-0.311, P=0.013). The positive correlation did also present between the cortical thickness of right precentral gyrus and ALSFRS-R score (r=0.271, P=0.032). For patients with ALS-bulbar, no correlation was shown between the cortical thickness of positive brain regions with either disease duration or ALSFRS-R score (both P>0.05). For patients with ALS-spinal, the partial correlation analysis demonstrated the cortical thickness of left insula (r=-0.409, P=0.004) and right gyrus rectus (r=-0.351, P=0.014) were negatively associated with the disease duration. No correlation was shown between the cortical thickness of these regions with ALSFRS-R score.
Table 3 The correlation analysis between the cortical thickness of thinning brain regions and clinical variables in ALS§
| Brain regions | Cortical thickness (mm) | Disease duration | ALSFRS-R score | |||
|---|---|---|---|---|---|---|
| r | Pvalue | r | Pvalue | |||
| ALS vs. NC | ||||||
| Left precentral gyrus | 2.77±0.22 | 0.003 | 0.979 | 0.245 | 0.053 | |
| Left postcentral gyrus | 2.26±0.19 | -0.052 | 0.684 | 0.126 | 0.326 | |
| Right gyrus rectus | 3.31±0.19 | -0.311 | 0.013 | -0.018 | 0.886 | |
| Right precentral gyrus | 2.88±0.15 | -0.081 | 0.528 | 0.271 | 0.032 | |
| ALS-spinal vs. NC | ||||||
| Left insula | 3.95±0.35 | -0.409 | 0.004 | -0.011 | 0.943 | |
| Right gyrus rectus | 3.34±0.19 | -0.351 | 0.014 | -0.022 | 0.881 | |
| ALS-bulbar vs. NC | ||||||
| Left precentral gyrus | 2.70±0.22 | -0.226 | 0.458 | 0.224 | 0.461 | |
| Right supplementary motor cortex | 2.19±0.14 | 0.071 | 0.818 | 0.204 | 0.505 | |
§:Plus-minus values are means and standard deviation.
DISCUSSION
The results in this study demonstrated that selective motor cortex and extra-motor cortex were involved in patients with ALS. The thinning of bilateral motor cortices was consistent with previous studies,16,17 and could underlie the relation between pathological characteristics in ALS and MR spectroscopy findings.26 However, meta-analysis of VBM studies 9,10,27 demonstrated that asymmetric motor cortex volume loss commonly present in ALS patients. The inconsistence of this result with our findings may be associated with the different image processing methods. SBM method we used in this study reflected the altered cortical thickness, while VBM method presented the altered cortical volume. In the current study, the thinning of bilateral motor cortices may be the main neuromechanism and served as the direct evidence for upper motor neurons damage, and it may be associated with the decreased number and shape of cortical neurons.28,29
In this study, the extra-motor cortices thinning was also observed in left postcentral gyrus and right gyrus rectus in ALS patients, which suggested the ALS involves the motor cortex but may not confine to the motor cortex. On contrast, in the previous document, motor cortex involvement was a common finding, while extra-motor cortex involvement was not commonly reported. Herein, the extra-motor cortices involvement should be carefully interpreted. It may be associated with the disease duration, cognitive state, or other clinical variables. From the pathological viewpoints, it may be related to the widespread reactive astrocytes in the cortex of ALS.30
The partial correlation analysis revealed that only right motor cortex thinning was associated to disease disability. Considering the symmetrical thinning pattern we found in this study, the asymmetrical correlation with disease disability further indicated that the right motor cortex thinning may play a key roles in ALS development and could be considered as a imaging biomarker for ALS.12 This study also demonstrated that extra-motor (right gyrus rectus) thinning was related to disease duration, which suggested that ALS was a complex degenerative disease involving multisystem beyond the motor system.9
Further clinical subtypes analysis in this study demonstrated that bulbar-onset and spinal-onset ALS had different cortical thinning patterns. For the bulbar-onset ALS, motor cortex was involved and the extra-motor cortex was spared, whereas in spinal-onset ALS, extra-motor cortex was involved, and the motor cortex was spared. This phenomenon of cortical thinning indicated that bulbar-onset ALS may only involve the upper motor neuron (UMN) and might be considered as UMN disorder with sparing of extra-motor. Meanwhile, spinal-onset ALS could be regarded as lower motor neurons (LMN) disorder with sparing of extra-motor cortex and motor cortex involvement. The findings support the viewpoint that bulbar-onset ALS is likely a simple motor neuron disorder, which is inconsistent with the conventional understanding that it is a multi-systematic disorder.2,5
Further correlation analysis revealed that bilateral motor cortex thinning was related to neither the disease duration nor the disease disability in bulbar-onset ALS, which suggested that motor cortex thinning may be the intrinsic pathophysiological changes in bulbar-onset ALS. This finding in bulbar-onset ALS was not consistent with the results in overall ALS patients, where the right motor cortex thinning was positively associated with ALS functional rating score. The small sample size and heterogeneity in the severity of the disease in this study might contribute to this inconsistence. This study also showed that in spinal-onset ALS, extra-motor cortex thinning was associated to the disease duration but not to the disease disability, which indicated that it may be the secondary pathophysiological change, and the underlying mechanism need to be further elucidated in future.
This study did not find significant difference in cortical thinning between bulbar-onset and spinal-onset ALS, which was different from our previous study where we found altered volumes of gray matter between ALS-bulbar and ALS-spinal group.20 The reason may be associated with the different imaging processing methods in these two studies. In the previous study,20 VBM method was used and the result indicated the volume changes, while in the current study, SBM method was used and the result represent the cortical thickness changes.
The limits of this study included: 1. the relatively small sample size of bulbar-onset ALS patients compared to the spinal-onset ALS in this study may cause sampling errors; 2 although MMSE was performed to exclude dementia, the mild cognitive impairment was not excluded, which could be a confounder factor besides age and sex; 3. this study only observed bulbar-onset ALS and spinal-onset ALS, and for those of bulbar-spinal-onset ALS, further studies are needed in the future.
In summary, bilateral motor cortex thinning was the MRI signature of bulbar-onset ALS patients, and extra-motor cortex thinning was the MRI signature of spinal-onset ALS patients. Bulbar- and spinal-onset ALS may be a simple MND instead of multisystem disorder. The motor cortex thinning may be the intrinsic pathophysiological change that is associated to disease disability and play a key role in brain damage for upper motor neuron disorder. Extra-motor cortex thinning may be a secondary pathophysiological change related to disease duration and act as a pivotal in brain damage of lower motor neuron disorder.
参考文献
Amyotrophic lateral sclerosis: lower motor neuron disease spreading to upper motor neurons
Upper motor neuron and extra-motor neuron involvement in amyotrophic lateral sclerosis: a clinical and brain imaging review
There is an ongoing discussion whether ALS is primarily a disease of upper motor neurons or lower motor neurons. We undertook a review to assess how new insights have contributed to solve this controversy. For this purpose we selected relevant publications from 1995 onwards focussing on (1) primary targets and disease progression in ALS and variants of ALS, (2) brain imaging markers for upper motor neuron lesion, and (3) evidence for ALS being a multisystem disorder. Clinically, upper motor and lower motor neuron symptoms can occur in any order over time. Brain imaging markers show upper motor neuron involvement in early disease. Overlap syndromes of ALS and dementia, and involvement of autonomic and sensory nerves occur frequently. PET/SPECT scans, functional MRI and voxel based morphometry studies clearly show abnormalities in extra-motor areas of the brain. Pathologically, the 43 kDa TAR DNA-binding protein (TDP-43) provides a clue to these overlapping disorders. In conclusion, evidence accumulates that ALS is a multisystem disorder rather than a pure lower and/or upper motor neuron disorder.
Primary lateral sclerosis. Clinical features, neuropathology and diagnostic criteria
Motor neuron disease: a primary disorder of corticomotoneurons?
Frontotemporal white matter changes in amyotrophic lateral sclerosis
Abstract Cognitive dysfunction can occur in some patients with amyotrophic lateral sclerosis (ALS) who are not suffering from dementia. The most striking and consistent cognitive deficit has been found using tests of verbal fluency. ALS patients with verbal fluency deficits have shown functional imaging abnormalities predominantly in frontotemporal regions using positron emission tomography (PET). This study used automated volumetric voxel-based analysis of grey and white matter densities of structural magnetic resonance imaging (MRI) scans to explore the underlying pattern of structural cerebral change in nondemented ALS patients with verbal fluency deficits. Two groups of ALS patients, defined by the presence or absence of cognitive impairment on the basis of the Written Verbal Fluency Test (ALSi, cognitively impaired, n=11; ALSu, cognitively unimpaired n=12) were compared with healthy age matched controls (n=12). A comparison of the ALSi group with controls revealed significantly (p<0.002) reduced white matter volume in extensive motor and non-motor regions, including regions corresponding to frontotemporal association fibres. These patients demonstrated a corresponding cognitive profile of executive and memory dysfunction. Less extensive white matter reductions were revealed in the comparison of the ALSu and control groups in regions corresponding to frontal association fibres. White matter volumes were also found to correlate with performance on memory tests. There were no significant reductions in grey matter volume in the comparison of either patient group with controls. The structural white matter abnormalities in frontal and temporal regions revealed here may underlie the cognitive and functional imaging abnormalities previously reported in non-demented ALS patients. The results also suggest that extra-motor structural abnormalities may be present in ALS patients with no evidence of cognitive change. The findings support the hypothesis of a continuum of extra-motor cerebral and cognitive change in this disorder.
Voxel-based morphometry—the methods
Diffusion tensor imaging and voxel based morphometry study in amyotrophic lateral sclerosis: relationships with motor disability
The aim of this study was to investigate the extent of cortical and subcortical lesions in amyotrophic lateral sclerosis (ALS) using, in combination, voxel based diffusion tensor imaging (DTI) and voxel based morphometry (VBM). We included 15 patients with definite or probable ALS and 25 healthy volunteers. Patients were assessed using the revised ALS Functional Rating Scale (ALSFRS-R). In patients, reduced fractional anisotropy was found in bilateral corticospinal tracts, the left insula/ventrolateral premotor cortex, the right parietal cortex and the thalamus, which correlated with the ALSFRS-R. Increased mean diffusivity (MD) was found bilaterally in the motor cortex, the ventrolateral premotor cortex/insula, the hippocampal formations and the right superior temporal gyrus, which did not correlate with the ALSFRS-R. VBM analysis showed no changes in white matter but widespread volume decreases in grey matter in several regions exhibiting MD abnormalities. In ALS patients, our results show that subcortical lesions extend beyond the corticospinal tract and are clinically relevant.
Widespread sensorimotor and frontal cortical atrophy in Amyotrophic Lateral Sclerosis
Voxel-wise meta-analysis of gray matter changes in amyotrophic lateral sclerosis
Background:Increasing neuroimaging studies have revealed gray matter (GM) anomalies of several brain regions by voxel-based morphometry (VBM) studies in patients with amyotrophic lateral sclerosis (ALS). A voxel-wise meta-analysis was conducted to integrate the reported studies to determine the consistent GM alterations in ALS based on VBM methods. Methods:Ovid Medline, Pubmed, Emabase, and BrainMap database were searched for relevant studies.Data were extracted by two independent researchers. Voxel-wise meta-analysis was performed using the effect-size signed differential mapping (ES-SDM) software. Results:Twenty-nine VBM studies comprising 638 subjects with ALS and 622 healthy controls (HCs) met inclusion criteria.The global GM volumes of ALS patients were significantly decreased compared with those of HCs. GM reductions in patients were mainly located in the right precentral gyrus, the left Rolandic operculum, the left lenticular nucleus and the right anterior cingulate/paracingulate gyri. The right precentral gyrus and the left inferior frontal gyrus might be potential anatomical biomarkers to evaluate the severity of the disease, and longer disease duration was associated with more GM atrophy in the left frontal aslant tract and the right precentral gyrus in ALS patients. Conclusion:The results support that ALS is a complex degenerative disease involving multisystems besides the motor system.The mechanism of asymmetric atrophy of the motor cortex and the implication of Rolandic operculum involvement in ALS need to be further elucidated in future studies.
Motor and extra-motor gray matter atrophy in amyotrophic lateral sclerosis: quantitative meta-analyses of voxel-based morphometry studies
61 We performed meta-analyses of GM anomalies with 20 VBM studies in ALS patients.61 GM atrophy was consistently found in the frontal, temporal, and somatosensory areas.61 Disease duration and severity, and age were correlated with GM loss in ALS patients.61 We provide convergent evidence that ALS is a multisystem degenerative disorder.
Surface-based morphometry of the anterior cingulate cortex in first episode schizophrenia
Grey matter volume changes over the whole brain in amyotrophic lateral sclerosis: A voxel-wise meta-analysis of voxel based morphometry studies
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease with selected both upper and lower motor neuron involvement. Although some inconsistent results exist, both pathological studies and many structural neuroimaging studies have revealed brain volume changes in ALS. To provide an objective overview of structural changes in ALS, a voxel-wise meta-analysis was performed in published voxel based morphometry (VBM) studies. A systematic search of VBM studies was applied in ALS. Five studies met the inclusion criteria, comprising 84 ALS patients and 81 normal controls. A voxel-wise meta-analysis was performed on the retrieved VBM studies using signed differential mapping. Descriptive analysis showed that 25% of ALS patients had right precentral gyrus atrophy (2373 voxels). Group analysis demonstrated regional grey matter loss over the whole brain in the right precentral gyrus (p = 7.96 0103 100908084). Sensitivity analysis showed good sensitivity (157 voxels). In conclusion, right precentral grey matter atrophy was a common finding and prominent feature of brain structural changes in ALS.
Surface-based morphometry reveals caudate subnuclear structural damage in patients with premotor Huntington disease
Abstract In patients with premotor Huntington disease (pmHD), literature has reported decreases in caudate volume. However, the regional vulnerability of the caudate nucleus to pmHD remains to be clarified. We aimed to determine whether regional structural damage of the caudate nucleus was present in pmHD and was correlated with clinical profile using a surface-based morphometric technique applied to T1-weighted MRI. The study cohort consisted of 14 volunteers with genetically confirmed pmHD (6 males; 41.8 13.2 years) and 11 age- and sex-matched controls (5 males; 46.2 卤 11.9 years, p > 0.3). On 3-T T1-weighted images, bilateral caudate volumes were manually delineated. The resulting labels were converted to a surface, triangulated with 1002 points equally distributed across subjects using SPHARM-PDM. Displacement vectors were then computed between each individual and a template surface representing the whole cohort. Computing point-wise Jacobian determinants (JD) from these vectors quantified local volumes. We found decreases in bilateral global caudate volumes in the pmHD group compared to controls (t = 3.4; p = 0.002). Point-wise analysis of local volumes mapped caudate atrophy in pmHD primarily onto medial surface (t > 2.7; FDR < 0.05), with most pronounced changes in anteromedial subdivision. In a combined group of patients and controls, volume within the area presenting significant group difference was positively correlated with scores of executive function (r = 0.7; p < 0.001) and working memory (r = 0.6; p = 0.002). In patients, the caudate atrophy was associated with increase in disease burden (r = 0.7; p = 0.005). Caudate subnuclear atrophy measured using our surface-based morphometric technique is evident in pmHD, correlates with clinical variables, and may provide a more sensitive biomarker than global volumes.
Cortical abnormalities in Parkinson’s disease patients and relationship to depression: A surface-based morphometry study
61We examined cortical abnormalities in PD patients using surface-based morphometry.61Cortical thickness was found reduced in the prefrontal cortex of PD patients.61Depressed PD patients showed increased brain area in orbitofrontal-insula region.61These results might be helpful for diagnosis and treatment of depression in PD.
The effects of apolipoprotein epsilon 4 on aging brain in cognitively normal Chinese elderly: a surface-based morphometry study
Default mode network (DMN) has been reported to be susceptible to APOEε4 genotype. However, the APOEε4-related brain changes in young carriers are different from the ones in elderly carriers. The current study aimed to evaluate the cortical morphometry of DMN subregions in cognitively normal elderly with APOEε4. 11 cognitively normal senior APOEε4 carriers and 27 matched healthy controls (HC) participated the neuropsychological tests, genotyping, and magnetic resonance imaging (MRI) scanning. Voxel-based morphometry (VBM) analysis was used to assess the global volumetric changes. Surface-based morphometry (SBM) analysis was performed to measure regional gray matter volume (GMV) and gray matter thickness (GMT). Advancing age was associated with decreased GMV of DMN subregions. Compared to HC, APOEε4 carriers presented cortical atrophy in right cingulate gyrus (R_CG) (GMV: APOE carriers: 8475.23 ± 1940.73 mm3, HC: 9727.34 ± 1311.57 mm3,t= 2.314,p= 0.026, corrected) and left insular (GMT: APOEε4 carriers: 3.83 ± 0.37 mm, HC: 4.05 ± 0.25 mm,t= 2.197,p= 0.033, corrected). Our results highlight the difference between different cortical measures and suggest that the cortical reduction of CG and insular maybe a potential neuroimaging marker for APOE 4εsenior carriers, even in the context of relatively intact cognition.
Decreased thickness of primary motor cortex in primary lateral sclerosis
Detection of motor cortex thinning and corticospinal tract involvement by quantitative MRI in amyotrophic lateral sclerosis
URL
PMID:1862277218622772
[本文引用: 1]

We prospectively investigated pathological modifications in the corticospinal tract (CST), by diffusion tensor imaging (DTI) in 14 patients with sporadic amyotrophic lateral sclerosis (ALS) and 12 healthy volunteers. We used a validated automated method to accurately measure the in vivo thickness of the cerebral cortex. We found a reduction of precentral cortical ribbon thickness in ALS patients with respect to control subjects. DTI metrics demonstrated disorganization of the CST, as characterized by decreased fractional anisotropy (FA) and increased Apparent Diffusion Coefficient in ALS patients with respect to control subjects. Decreased mean FA values along the CST significantly correlated with clinical measures of pyramidal and bulbar impairment.
High-resolution 7T MR imaging of the motor cortex in amyotrophic lateral sclerosis
Frontotemporal cortical thinning in amyotrophic lateral sclerosis
The extensive application of advanced MR imaging techniques has undoubtedly improved our knowledge of the pathophysiology of amyotrophic lateral sclerosis. Nevertheless, the precise extent of neurodegeneration throughout the central nervous system is not fully understood. In the present study, we assessed the spatial distribution of cortical damage in amyotrophic lateral sclerosis by using a cortical thickness measurement approach.Surface-based morphometry was performed on 20 patients with amyotrophic lateral sclerosis and 18 age- and sex-matched healthy control participants. Clinical scores of disability and disease progression were correlated with measures of cortical thickness.The patients with amyotrophic lateral sclerosis showed a significant cortical thinning in multiple motor and extramotor cortical areas when compared with healthy control participants. Gray matter loss was significantly related to disease disability in the left lateral orbitofrontal cortex (P = .04), to disease duration in the right premotor cortex (P = .007), and to disease progression rate in the left parahippocampal cortex (P = .03).Cortical thinning of the motor cortex might reflect upper motor neuron impairment, whereas the extramotor involvement seems to be related to disease disability, progression, and duration. The cortical pattern of neurodegeneration depicted resembles what has already been described in frontotemporal dementia, thereby providing further structural evidence of a continuum between amyotrophic lateral sclerosis and frontotemporal dementia.
Gray matter volume changes over the whole brain in the bulbar- and spinal-onset amyotrophic lateral sclerosis: a voxel-based morphometry study
The asymmetric GM atrophy of the motor cortex and extra-motor cortex represents the common MRI structural signatures of spinal-onset ALS, and sole extra-motor cortex atrophy represents the structural signatures of bulbar-onset ALS. The present study also demonstrated that the pattern of GM damage is likely to distribute wider in spinal-onset ALS than in bulbar-onset ALS.
El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis
(2000). El Escorial revisited: Revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis and Other Motor Neuron Disorders: Vol. 1, No. 5, pp. 293-299.
Study of functional rating scale for amyotrophic lateral sclerosis: revised ALSFRS(ALSFRS-R) Japanese version
Study of functional rating scale for amyotrophic lateral sclerosis : revised ALSFRS (ALSFRS-R) Japanese version No To Shinkei 53(4), 346-355, 2001
Mini-Mental State Examination (MMSE)
Patient’s Name: Date:Instructions: Ask the questions in the order listed. Score one point for each correctresponse within each question or activity.Maximum Patient’sQuestionsScore Score5 “What is the year? Season? Date? Day of the week? Month?”5 “Where are we now: State? County? Town/city? Hospital? Floor?”The examiner names three unrelated objects clearly and slowly, thenasks the patient to name all three of them. The patient’s response is3used for scoring. The examiner repeats them until patient learns all ofthem, if possible. Number of trials: ___________“I would like you to count backward from 100 by sevens.” (93, 86, 79,5 72, 65, …) Stop after five answers.Alternative: “Spell WORLD backwards.” (D-L-R-O-W)“Earlier I told you the names of three things. Can you tell me what those3were?”Show the patient two simple objects, such as a wristwatch and a pencil,2and ask the patient to name them.1 “Repeat the phrase: ‘No ifs, ands, or buts.’”“Take the paper in your right hand, fold it in half, and put it on the floor.”3(The examiner gives the patient a piece of blank paper.)“Please read this and do what it says.” (Written instruction is “Close1your eyes.”)“Make up and write a sentence about anything.” (This sentence must1contain a noun and a verb.)“Please copy this picture.” (The examiner gives the patient a blankpiece of paper and asks him/her to draw the symbol below. All 10angles must be present and two must intersect.)130 TOTAL(Adapted from Rovner & Folstein, 1987)1Source: www.medicine.uiowa.edu/igec/tools/cognitive/MMSE.pdf Provided by NHCQF, 0106-410Instructions for administration and scoring of the MMSEOrientation (10 points):61 Ask for the date. Then specifically ask for parts omitted (e.g., "Can you also tell me what season itis?"). One point for each correct answer.61 Ask in turn, "Can you tell me the name of this hospital (town, county, etc.)?" One point for eachcorrect answer.Registration (3 points):61 Say the names of three unrelated objects clearly and slowly, allowing approximately one second foreach. After you have said all three, ask the patient to repeat them. The number of objects thepatient names correctly upon the first repetition determines the score (0-3). If the patient does notrepeat all three objects the first time, continue saying the names until the patient is able to repeat allthree items, up to six trials. Record the number of trials it takes for the patient to learn the words. Ifthe patient does not eventually learn all three, recall cannot be meaningfully tested.61 After completing this task, tell the patient, "Try to remember the words, as I will ask for them in alittle while."Attention and Calculation (5 points):61 Ask the patient to begin with 100 and count backward by sevens. Stop after five subtractions (93,86, 79, 72, 65). Score the total number of correct answers.61 If the patient cannot or will not perform the subtraction task, ask the patient to spell the word "world"backwards. The score is the number of letters in correct order (e.g., dlrow=5, dlorw=3).Recall (3 points):61 Ask the patient if he or she can recall the three words you previously asked him or her toremember. Score the total number of correct answers (0-3).Language and Praxis (9 points):61 Naming: Show the patient a wrist watch and ask the patient what it is. Repeat with a pencil. Scoreone point for each correct naming (0-2).61 Repetition: Ask the patient to repeat the sentence after you ("No ifs, ands, or buts."). Allow only onetrial. Score 0 or 1.61 3-Stage Command: Give the patient a piece of blank paper and say, "Take this paper in your righthand, fold it in half, and put it on the floor." Score one point for each part of the command correctlyexecuted.61 Reading: On a blank piece of paper print the sentence, "Close your eyes," in letters large enoughfor the patient to see clearly. Ask the patient to read the sentence and do what it says. Score onepoint only if the patient actually closes his or her eyes. This is not a test of memory, so you mayprompt the patient to "do what it says" after the patient reads the sentence.61 Writing: Give the patient a blank piece of paper and ask him or her to write a sentence for you. Donot dictate a sentence; it should be written spontaneously. The sentence must contain a subjectand a verb and make sense. Correct grammar and punctuation are not necessary.61 Copying: Show the patient the picture of two intersecting pentagons and ask the patient to copy thefigure exactly as it is. All ten angles must be present and two must intersect to score one point.Ignore tremor and rotation.(Folstein, Folstein & McHugh, 1975)2Source: www.medicine.uiowa.edu/igec/tools/cognitive/MMSE.pdf Provided by NHCQF, 0106-410Interpretation of the MMSEMethod Score InterpretationSingle Cutoff
Cortical thickness and central surface estimation
78 Cortical thickness estimation and central surface reconstruction 78 Voxel-based projection scheme based on tissue segmentation 78 Phantom creation scheme for thickness and surface validation 78 Third party phantoms and real data for comparison with other software (Freesurfer)
An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest
In this study, we have assessed the validity and reliability of an automated labeling system that we have developed for subdividing the human cerebral cortex on magnetic resonance images into gyral based regions of interest (ROIs). Using a dataset of 40 MRI scans we manually identified 34 cortical ROIs in each of the individual hemispheres. This information was then encoded in the form of an atlas that was utilized to automatically label ROIs. To examine the validity, as well as the intra- and inter-rater reliability of the automated system, we used both intraclass correlation coefficients (ICC), and a new method known as mean distance maps, to assess the degree of mismatch between the manual and the automated sets of ROIs. When compared with the manual ROIs, the automated ROIs were highly accurate, with an average ICC of 0.835 across all of the ROIs, and a mean distance error of less than 1 mm. Intra- and inter-rater comparisons yielded little to no difference between the sets of ROIs. These findings suggest that the automated method we have developed for subdividing the human cerebral cortex into standard gyral-based neuroanatomical regions is both anatomically valid and reliable. This method may be useful for both morphometric and functional studies of the cerebral cortex as well as for clinical investigations aimed at tracking the evolution of disease-induced changes over time, including clinical trials in which MRI-based measures are used to examine response to treatment.
Alzheimer disease pathology in amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) is characterized by degeneration of upper and lower motor neurons. In some ALS patients, dementia or aphasia may be present (ALS-D). The dementia is most commonly a frontotemporal dementia (FTD), and many of these cases have ubiquitin-positive, tau-negative inclusions in neurons of the dentate gyrus and superficial layers of the frontal and temporal lobes. Identical inclusions have been found in cases presenting with FTD and have been designated motor neuron disease (MND)-inclusions. Cases of ALS-D without MND-inclusions have been reported to show neocortical gliosis, neuronal loss, and superficial spongiosis, but there have also been scattered case reports of ALS with Alzheimer鈥檚 disease (AD). To determine whether AD pathology may play a role in the dementia or aphasia syndromes in ALS, we reviewed 30 cases of sporadic ALS diagnosed at the University of Pittsburgh Medical Center. A clinical history of ALS-D was found in 24.1% of the cases, of which 57% had MND-inclusions. Although the ALS-D cases with MND-inclusions typically had amyloid-beta (A尾) plaques, there were no neuritic plaques. Three cases of ALS-D had no MND-inclusions, and two of these fulfilled pathological criteria for AD. One ALS-D case showed severe amyloid angiopathy but no neuritic plaques or MND-inclusions. MND-inclusions were not found in any ALS case without dementia; however, four patients without dementia or aphasia showed moderate or frequent numbers of neuritic plaques. In conclusion, we found that approximately 30% of ALS cases with dementia have AD and that some ALS cases without frank dementia have significant AD pathology.
Grey matter volume changes over the whole brain in amyotrophic lateral sclerosis: A voxel-wise meta-analysis of voxel based morphometry studies
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease with selected both upper and lower motor neuron involvement. Although some inconsistent results exist, both pathological studies and many structural neuroimaging studies have revealed brain volume changes in ALS. To provide an objective overview of structural changes in ALS, a voxel-wise meta-analysis was performed in published voxel based morphometry (VBM) studies. A systematic search of VBM studies was applied in ALS. Five studies met the inclusion criteria, comprising 84 ALS patients and 81 normal controls. A voxel-wise meta-analysis was performed on the retrieved VBM studies using signed differential mapping. Descriptive analysis showed that 25% of ALS patients had right precentral gyrus atrophy (2373 voxels). Group analysis demonstrated regional grey matter loss over the whole brain in the right precentral gyrus (p = 7.96 0103 100908084). Sensitivity analysis showed good sensitivity (157 voxels). In conclusion, right precentral grey matter atrophy was a common finding and prominent feature of brain structural changes in ALS.
Unchanged total number of neurons in motor cortex and neocortex in amyotrophic lateral sclerosis: a stereological study
Modern stereological methods provide precise and reliable estimates of the number of neurons in specific regions of the brain. The total number of neurons in the neocortex and motor cortex from eight patients suffering from amyotrophic lateral sclerosis (ALS) and nine controls was estimated. No attempt was made to estimate subpopulations of neurons such as the number of giant pyramidal cells of Betz. No difference was found in the average number of neurons in neocortex in ALS and controls, 21.7 and 22.3脳10 9, respectively, and 1.33 and 1.29脳10 9 in motor cortex, respectively. In the light of our stereological measurements, results obtained from in-vivo proton magnetic resonance spectroscopy ( 1H-MRS), suggesting neuronal loss in ALS, may instead be due to neuronal metabolic dysfunction and/or alteration in the size or the volume fraction of the neurons.
Changes in shapes of surviving motor neurons in amyotrophic lateral sclerosis
In , motor neurons in the spinal cord and brainstem shrink before they die. In 12 cases of sporadic , and in 11 control subjects, we have measured the neurons in the second sacral segment and the hypoglossal , and have calculated a 'shape index' that shows the convexity or concavity of the . (The shape index, SI = 100 x C/P, where C is the circumference of the largest circle that can be inscribed in the neuron and P is the perimeter of the perikaryon, including the bases of the dendrites as seen in a Nissl preparation. The shape index increases with increasing convexity of the cell.) In the ventral horn of segment S2 and in the hypoglossal , the surviving motor neurons in showed significantly decreased size and increased shape index (convexity) of the . By contrast, the of Onuf in segment S2, consisting of neurons that supply the pelvic floor muscles, was preserved in . Its cells did not differ significantly in size or convexity between the and control groups. In both the hypoglossal and S2 neuronal populations in , the sizes of the cells were positively correlated with the numbers of surviving motor neurons. However, there was no correlation of the shape index with numbers of cells. This is interpreted as due to shrinkage of neurons still taking place at the time of , when the changes in shape were probably largely completed. These observations indicate that the mechanism of neuronal atrophy in may involve both reduced protein synthesis and enzymatic degradation of the within the larger dendrites.
Reactive astrocytes are widespread in the cortical gray matter of amyotrophic lateral sclerosis
Abstract The distribution of reactive astrocytes was examined in the cortical gray matter of non-motor and motor regions from cases of familial and sporadic amyotrophic lateral sclerosis (ALS) and compared to that of β-amyloid deposits. By glial fibrillary acidic protein immunocytochemistry, patches of reactive astrocytes, characterized by multiple reactive astrocytes in a circular or patch-like formation, occurred in 12 of 15 ALS cases examined. These patches of reactive astrocytes were not restricted to the motor cortex but were found in the gray matter in ALS in all examined brain regions, including frontal, temporal, inferior parietal, cingulate, occipital, and motor cortices, from both familial and sporadic ALS cases. Reactive astrocytes were also found in the subpial region and at the gray/white matter junction. Because patches of astrocytes can occur in association with senile plaques, β-amyloid was localized. By immunostaining, β-amyloid deposits were observed in five of the 15 ALS cases: three cases had only early plaques, two had both early and classic plaques. The number of ALS cases with both astrocyte patches and amyloid plaques was four of 15, but typically astrocyte patches in ALS occurred without any evidence of an association with β-amyloid deposits. Therefore, the astrocyte patches in ALS are not the result of β-amyloid deposition. The widespread occurrence of reactive astrocytes, as patches in the cortical gray matter and in the subpial region and at the gray/white matter junction, is evidence of a widespread pathology in ALS cortex in both familial and sporadic forms of the disease. 08 1994 Wiley-Liss, Inc.