SEPSIS and septic shock are major health problems, affecting millions of people around the world each year. It has been demonstrated that increased compliance with the Surviving Sepsis Campaign (SSC) resuscitation bundles is associated with a reduction in mortality rates.1 However, sepsis and septic shock remain a challenge, with their high morbidity and mortality.2
Early goal-directed therapy (EGDT) has been constantly discussed and questioned by researchers since its publication.3-4 Several studies have noted that EGDT was not superior to “usual care” in the treatment of early septic shock.5-7 Nonetheless, it remains the cornerstone for the management of sepsis and septic shock patients.8 Head and Coopersmith9 suggested that although the specific EGDT protocol is not beneficial if applied to all patients with sepsis, key tenets of sepsis management are indicated in all septic patients, and the management of sepsis could evolve from EGDT to personalized care.
We also believe in the tenets of EGDT and developed a novel protocol based on them. We thought the goal should be personalized and, most importantly, should be managed on the basis of timing.10 The protocol, called “target and endpoint”, has been in development and implementation for up to 5 years in our department and has been strictly applied during daily rounds. However, how it influences the resuscitation of septic patients in the ICU has not been reported. We decided to retrospectively study the septic patients in this department and investigate what effect the target-and-endpoint protocol had on the treatment of these patients.
PATIENTS AND METHODS
Study population
We retrospectively reviewed the electronic medical database to identify septic patients with an acute onset of infection and being administered vasopressors on at least the first day in the ICU of the Peking Union Medical College Hospital. Patients were admitted to the ICU from May 1st, 2014 to May 1st, 2017.
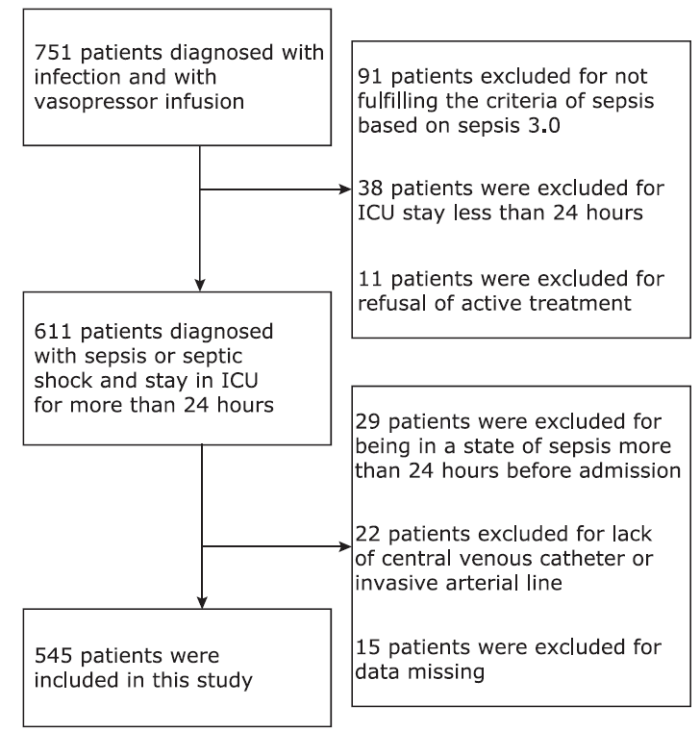
Patients were excluded if they met the following criteria: clinical presentation not consistent with the diagnosis of sepsis or septic shock, lack of central venous pressure (CVP) monitoring or invasive arterial pressure monitoring, ICU stay length shorter than 24 hours, refusal of active treatment, data missing or a state of sepsis lasting more than 24 hours before being transferred to the ICU. Finally, a total of 545 septic patients were included (Fig. 1).
The diagnosis of sepsis was made based on the new Sepsis-3 definition, which includes a suspected or confirmed infection and an acute change of ≥2 points in the patient’s total sequential organ failure assessment score (SOFA) as a result of the infection. Septic shock patients were identified by the necessity of vasopressors to maintain a mean arterial pressure of 65 mm Hg (1 mm Hg=0.133 kPa) or greater and a serum lactate level greater than 2 mmol/L in the absence of hypovolemia.11
Patients’ data were collected from the hospital’s electronic medical database. The data designated as 0-hour data were obtained at the exact time of admission. The data designated as 3-, 6- and 24-hour data were measured at 3, 6 and 24 hours after admission. Acute physiology and chronic health evaluation score II (APACHEII) and SOFA scores were calculated from the worst parameters within the first 24 hours, which were gathered from the electronic records. In-hospital mortality was defined as the proportion of patients who died during the period from ICU admission to discharge from the hospital.
The study was conducted according to the Declaration of Helsinki and was approved by the ethics committee of our institution. No informed consent was needed for this retrospective observational study.
“Target-and-endpoint” protocol
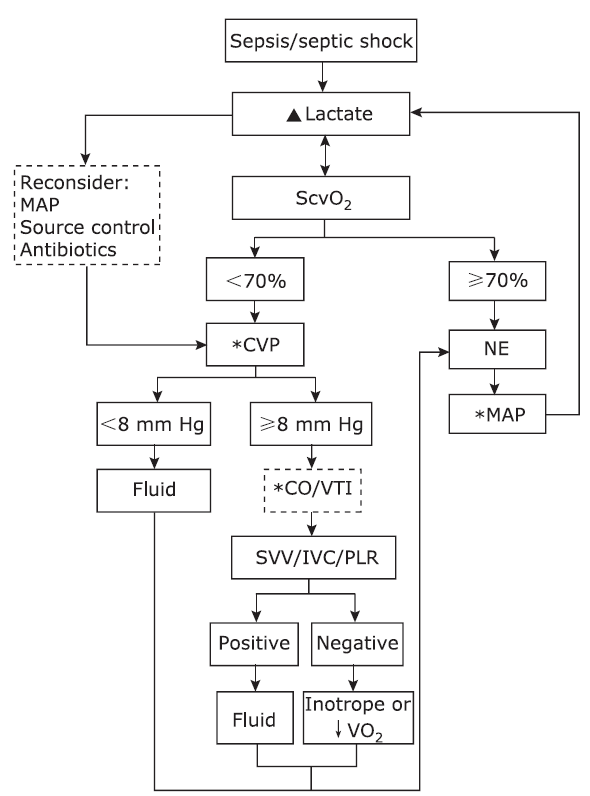
The “target-and-endpoint” protocol for resuscitation of the sepsis and septic shock patients is shown in Fig. 2. If the patient was diagnosed with sepsis or septic shock, the resuscitation protocol was indicated.
Figure 2.
The “target-and-endpoint” protocol for resuscitation of the sepsis and septic shock patients.
▲Lactate level and lactate clearance rate were set as the “endpoint” parameter.
*CVP, MAP and CO/VTI were set as the “target” parameter.
MAP: mean arterial pressure; ScvO2: saturation of central venous oxygen; CVP: central venous pressure; NE: norepinephrine; CO: cardiac output; VTI: velocity-time-integral; SVV: stroke volume variation; IVC: inferior vena cava; PLR: passive leg raising; ↓VO2: decreased oxygen consumption.
The ultimate goal (endpoint) of the treatment was the clearance of lactate, specifically, at least a 10% drop by 6 hours after admission. To accomplish the ultimate goal, we set three targets: mean arterial pressure (MAP), central venous pressure (CVP) and, if necessary, the cardiac output/velocity-time integral (VTI). A personalized value of each target was selected at 6 hours or even sooner while the patient’s condition was monitored. At any given time, a specific value of each target was mandatory for each patient. The lactate level and saturation of central venous oxygen (ScvO2) were to be measured regularly, and the target values were to be assessed and adjusted; most importantly, the actual values of those variables were to be maintained on target if such targets had been set.
If ScvO2 was below 70% and CVP was below 8 mm Hg, volume expansion was recommended. If the CVP was equal or greater than 8 mm Hg, it was left to the doctors’ discretion to monitor cardiac output. Volume responsiveness was to be assessed, whether through inferior vena cava (IVC) variability, VTI variability, stroke volume variation (SVV), pulse pressure variation (PPV), passive leg raising (PLR) or fluid challenge. If volume responsiveness was positive, fluid was to be administered. Otherwise, it was left to the doctors’ discretion to decide whether to prescribe inotrope or take measures to decrease the oxygen consumption. Then norepinephrine would be given to maintain the MAP level according to the baseline blood pressure of each specific patient.
If ScvO2 was above 70%, then the MAP goal was set and maintained. If the goal of CVP, MAP and cardiac output (if necessary) was reached, and lactate clearance still deteriorated, it was deemed acceptable to tamper MAP level and turn again to source control and antibiotic adjustment. If the lactate clearance goal was reached, the clinicians need to assess whether the CVP could be lowered any further and whether the MAP or cardiac output/VTI needed to be adjusted.
If the patient was diagnosed with sepsis but the lactate level was below 2 mmol/L, but the ScvO2 less than 60%, then there would be a high risk to develop hyperlactatemia, the resuscitation would still be proceeded. If the ScvO2 was greater than 60%, then the clinicians need to assess whether the CVP could be lowered any further and whether the MAP or cardiac output/VTI needed to be adjusted.
Statistical analysis
Statistical analysis was performed using the statistical software package SPSS 13.0 (SPSS Inc., Chicago, Illinois, USA). Continuous data were expressed as the mean ± standard deviation or as the median and the interquartile range (IQR). Categorical variables were presented as the number and percentage in each category. At admission patients were divided into the low-CVP group (CVP<8 mm Hg) and the high-CVP group (CVP≥8 mm Hg) according to CVP level, the low-MAP group (MAP<75 mm Hg) and the high-MAP group (MAP≥75 mm Hg) according to MAP level, and the low-ScvO2 group (ScvO2<70%) and the high-ScvO2 group (ScvO2≥70%) according to ScvO2 level. Group comparisons of SOFA and APACHE II scores, lactate level and in-hospital mortality were performed by Student’s t-test, Man-Whitney U test or the chi-squared test when appropriate. The variance analysis of repeated measurement data was used to compare the differences of each index within the groups and then least significant difference test was used to compare the difference between two groups. All P values were two tailed and were considered significant for P<0.05.
RESULTS
General characteristics of all patients
Their mean age of the enrolled subjects was 60.6±16.9 years old, and 59.2% (323/545) were men. The median APACHE II and SOFA scores were 22 (IQR,17- 29) and 11 (IQR, 9-14), respectively. The median maximum body temperature was 38°C. The median white blood cell count was 12.4×109/L (IQR, 7.6×109-18.3×109/L), and the median procalcitonin level was 4.0 (IQR, 0.9-21.1) ng/ml.
The sources of infection included pneumonia (60.0%), intraabdominal infection (28.6%), bacteremia (7.5%) and other infections (3.9%), such as urinary tract infection, dermal infection, and central nervous system infection etc. The comorbidities included hypertension (31.9%), coronary artery disease (4.6%), diabetes mellitus (7.2%) and chronic renal failure (10.1%).
The proportion of patients on ventilation was 87.2% (475/545). The mean positive end-expiratory pressure and plateau pressure were 7.1±2.4 cmH2O and 22.7±6.3 cmH2O respectively. The median norepinephrine dose was 0.15 (IQR, 0.10-0.42) μg/kg·min. The median ICU stay length was 11 (IQR, 5-19) days, and in-hospital mortality was 9.4% (51/545).
Arterial blood lactate level and hemodynamics
The quantities of fluid administered at 3 hours and 24 hours were 965 (IQR, 615-1566) ml and 3207 (IQR, 2495-3950) ml, respectively. Only 19.8% (n=108) of patients were administered over 30 ml/kg of fluid at 3 hours. The rate of fluid loading was 250-500 ml/30 min or faster but with close monitoring. Among all the patients, 18.7% had a negative fluid balance during the first 24 hours and the median volume was 1444 (IQR, 489-2775) ml. The patients who were administered dobutamine accounted for 11% of all patients and the median dose was 3 (IQR, 2-5) μg/kg·min.
The MAP level was much higher than the target in the EGDT protocol, with 89.7% (489/545) having MAP greater than 75 mm Hg at 6 hours. Only 68.8% (375/545) of patients had CVP greater than 8 mm Hg at 6 hours, and 70.6% (385/545) of patients had ScvO2 greater than 70.0% at 6 hours. Among all the patients, 48.1% (262/545) had a lactate level above 2 mmol/L at admission. The 6-hour lactate clearance rate was 21.6% (IQR, 8.6%-39.0%). The arterial blood lactate level on admission and 6 hours of admission were 1.8 (IQR, 1.2-3.2) mmol/L and 1.6 (IQR, 1.1-2.6) mmol/L, respectively.
Subgroup comparison
The low-CVP group displayed lower SOFA and APACHE II scores than the high-CVP group (all P<0.001). No significant difference was found in lactate level (P=0.110) and in-hospital mortality between the two groups (P=0.627). (Table 1)
Table 1 Comparisons of SOFA and APACHE II scores, 0-hour lactate level and in-hospital mortality between subgroups
| Groups | n | SOFA (score) | APACHE Ⅱ(score) | 0-hour lactate level (mmol/L) | In-hospital mortality (%) |
|---|---|---|---|---|---|
| Low-CVP group (CVP<8 mm Hg) | 187 | 11 | 20 | 1.8 | 11.3 |
| High-CVP group (CVP≥8 mm Hg) | 358 | 12 | 23 | 1.9 | 9.5 |
| P value | <0.001 | <0.001 | 0.110 | 0.627 | |
| Low-MAP group (MAP<75 mm Hg) | 148 | 11 | 24 | 1.7 | 8.8 |
| High-MAP group (MAP≥75 mm Hg) | 397 | 11 | 22 | 1.9 | 9.5 |
| P value | 0.455 | 0.019 | 0.111 | 0.807 | |
| Low-ScvO2 group (ScvO2<70%) | 185 | 12 | 23 | 1.8 | 11.4 |
| High-ScvO2 group (ScvO2≥70%) | 360 | 11 | 22 | 1.9 | 8.3 |
| P value | 0.614 | 0.227 | 0.628 | 0.250 |
SOFA: sequential organ failure assessment score; APACHE Ⅱ: acute physiology and chronic health evaluation score Ⅱ.
In comparison with the high-MAP group, the low-MAP group displayed higher APACHE II scores (P=0.019) and similar SOFA scores (P=0.455). No difference was found on 0-hour lactate level (P=0.111) and in-hospital mortality (P=0.807) between the two groups. (Table 1)
No difference was found between the low-ScvO2 group and high-ScvO2 group in terms of SOFA (P=0.614), APACHE II (P=0.227), 0-hour lactate level (P=0.628) and in-hospital mortality (P=0.250). (Table 1)
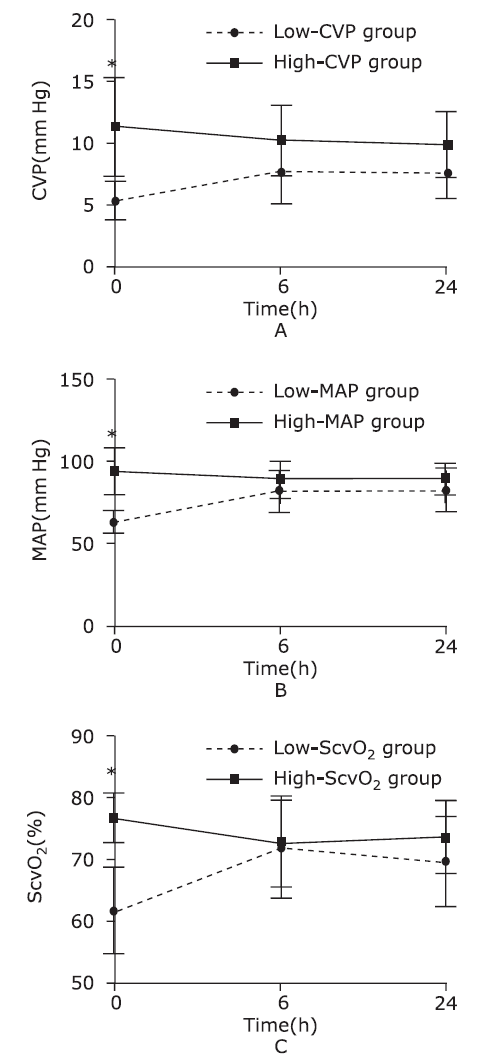
Target of CVP, MAP and ScvO2
For patients with CVP below 8 mm Hg at 0 h, the value at 0 h was significantly lower than that at 6 hours and 24 hours (P<0.001). No difference was found between the values at 6 hours and 24 hours (P=0.363). For patients with MAP below 75 mm Hg at 0 h, the value at 0 h was significantly lower than the value at 6 hours and 24 hours (P<0.001). No difference was found between the values at 6 hours and 24 hours (P=0.667). For patients with ScvO2 below 70% at 0 h, the value at 0 h was significantly lower than that at 6 hours and 24 hours (P<0.001). The value at 6 hours was slightly higher than the value at 24 hours, but the difference was not statistically significant (P=0.063). (Fig. 3)
Figure 3.
Comparisons of CVP (A), MAP (B) and ScvO2 (C) values before and after resuscitation.
*In comparison with values at 6 hours and 24 hours after admission, the corresponding values at admission were significantly lower or higher (P<0.001). No difference was found between the values at 6 hours and the corresponding values at 24 hours.
For patients with CVP greater than or equal 8 mm Hg at 0 h, the value at 0 h was significantly higher than the value at 6 hours and 24 hours (P<0.001). No difference was found between the values at 6 hours and 24 hours (P=0.452). For patients with MAP greater than or equal 75 mm Hg at 0 h, the value at 0 h was significantly higher than the value at 6 hours and 24 hours (P<0.001). No difference was found between the values at 6 hours and 24 hours (P=0.295). For patients with ScvO2 greater than or equal 70% at 0 h, the value at 0 h was significantly higher than the value at 6 hours and 24 hours (P<0.001). No difference was found between the values at 6 hours and 24 hours (P=0.116). (Fig. 3)
DISCUSSION
In this study, we found that the “target-and-endpoint” protocol was effective, with most patients surviving. However, we did not administer as much fluid as the SSC guideline recommended. We also did not set the target CVP and MAP goals as the EGDT recommended.
The protocol had been established long before this study, and its implementation was discussed during morning and evening rounds, which guaranteed the quality of the protocol. The data were all objective data collected from our electronic database. The database has been existed for 5 years, and several papers based on its data have been published.12-13 The results of this study demonstrated that the patients had rather high APACHE II and SOFA scores comparable to those of patients from prior studies including EGDT, ProCESS, and ARIZE. Nonetheless, the mortality was not as high in the present study.5-7, 14
The participants in this study were sepsis patients undergoing norepinephrine infusion. Previously, the SSC guidelines have defined septic shock as sepsis-induced hypotension persisting despite adequate fluid resuscitation.15 Hyperlactatemia and fluid-resistant hypotension requiring vasopressors are the prerequisites used to diagnose septic shock according to the new definition of Sepsis-3.16 Therefore, the study involved both sepsis and septic shock patients according to the new definition.
We chose arterial lactate level as the endpoint in our protocol as hyperlactatemia is a well-accepted marker of illness severity, with higher levels predicative of higher mortality.11, 17 The cause of hyperlactatemia might lie in altered microcirculation or disrupted mitochondrial dysfunction; the topic has attracted a great deal of interest, but there is still no adequate treatment method. Garrabou et al18 measured the mitochondrial activity of peripheral blood mononuclear cells in septic shock patients. Their study demonstrated that mitochondrial dysfunction may be responsible for cell damage in sepsis and may correlate with sepsis severity and outcome.
The SSC guidelines and their update clearly state that volume resuscitation should be performed within 3 hours.19 The notion of early resuscitation is thoroughly understood and widely accepted, and the fluid therapy or even more robust evaluation of volume status would be performed within 3 hours of admission. In our study, we found that only a small fraction of patients admitted to the ICU need more than 30 ml of fluid/kg within the first 3 hours. Because the protocol demanded that volume responsiveness should be evaluated if needed, we conclude that the reason for this is because more patients had been administered fluids in the emergency room, operating room or medical or surgical ward; therefore, they do not need as much volume at this time point. This also demonstrated an advantage of this protocol, namely, the ability to prevent volume overload and its related consequences.20 We fully agree the SSC is very valuable for patients who have not been resuscitated. However, septic shock patients are often resuscitated to some extent before being transferred to ICU. Therefore, the volume status assessment is crucial.
In this study, we found that the CVP value at 6 hours was much lower than that the EGDT protocol had suggested, meaning that much less fluid had been given, which is another indicator that the risk of volume overload is much lower.14-15 We found that high CVP at 6 hours did not mean that patients were resuscitated adequately; rather they were more severely ill, with higher APACHE II and SOFA scores and, eventually, higher mortality. Therefore, the CVP for each patient cannot be set at a fixed score; it is more reasonable to set a personalized goal. Prior research has found that increased CVP is associated with impaired renal function and all-cause mortality in a group of patients with cardiovascular diseases.21 Vellinga et al22 found that elevated CVP was associated with impairment of microcirculatory blood flow. Higher CVP means the impairment of microvascular perfusion through increases in venous pressure by venous congestion.
In our protocol, the CVP level is monitored and tapered to bring it as low as possible as long as tissue perfusion is sufficient. This is another reason the CVP level was kept slightly lower. The CVP is an indicator of the preload of the right heart; lowering it will benefit the function of the right heart, as well as kidney function and it is nevertheless useful when followed over time.23-24 Although we did not have access to the echocardiography results of these patients, the CVP value, which indicates the preload of the right heart, could be a result of cardiac dysfunction induced by septic shock. Septic cardiomyopathy, usually diagnosed through echocardiography, has a high incidence in septic shock patients, and both ventricles can be affected.25-26
A previous study noted that MAP combined with hyperlactatemia might be a strong predictor of worse prognosis.27 In the present study, the value of target MAP was slightly higher than that the SSC guidelines recommended. As in a real clinical situation, the setting of a target blood pressure level takes baseline blood pressure, urine output and lactate clearance into consideration. Nearly a third of our patients had hypertension. Asfar et al28 also concluded that septic patients with high blood pressure needed less renal replacement therapy. We found that when target blood pressure was set according to urine output in addition to lactate clearance rate, the MAP need to be higher than 65 mm Hg. Still, it is better for targets to be personalized. After admission, MAP decreased in some patients and increased in others. Higher MAP means the afterload of the heart will be increased, which should be taken into consideration as the heart is often compromised in patients with septic cardiomyopathy.29
ScvO2 plays the important role of testing the final, crucial question of whether oxygen delivery is adequate.30-31 However, the ARIZE and ProCESS study noted that mortality was not different in septic shock in a study of 300 patients when they were randomized to a target of ScvO2 of 70% versus lactate clearance of at least 10%. Although we did not follow the exact values of the goals recommended by EGDT and did not even fulfill the need for a total fluid infusion of 30 ml/kg, we argue that it is inappropriate to conclude that no protocol is necessary in these patients. Instead, we believe it is necessary to use a “personalized” protocol. We can see that fluid was administered according to each patient’s need, and MAP was slightly higher, meaning that the resuscitation was even stricter. This was consistent with the idea of Head et al.9 In this study, the high-ScvO2 group similarly showed no advantage over the low-ScvO2 group, which means that personalized protocols are needed.
The present study has several limitations. First, it is a single-center retrospective study and, therefore, is not enough to provide a definite conclusion. Although the volume restoration was known to be completed by 6 hours after admission, we were not able to define the exact moment when the patients’ volume status was adequate. Therefore, a prospective study is still needed to confirm the results. Second, due to the various measurements of cardiac output, that variable was not statistically available. Third, in contrast to other studies, the patients were not included immediately after the sepsis erupted; instead, most of them were being given fluid or even vasopressors. We believe this to be a characteristic of ICU patients. As most sepsis and septic shock patients will be transferred to the ICU, a protocol suited for ICU treatment would be meaningful. When the patients were treated, they were far from stable, most of them because of deterioration, and they were still deeply in need of resuscitation. Finally, there was no control group to demonstrate the efficacy of the protocol. Despite these limitations, we have a homogenous hemodynamic treatment protocol for the management of septic shock patients, and this study provides the general characteristics of these patients.
In conclusion, this study suggested that in the resuscitation of sepsis and septic shock patients in the ICU, the target values did not have to be within the “normal range” recommended by EGDT. The “target-and-endpoint” protocol, which aimed for personalized goals, deserves more consideration.
Conflicts of interest statement
The authors declare that they have no competing interests.
参考文献
Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study
Hospital deaths in patients with sepsis from 2 independent cohorts
1 + Levy 02MM, Fink 02MP, Marshall 02JC, 02et al; International Sepsis Definitions Conference. 022001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference.02 Intensive Care Med . 2003;29(4):530-538. PubMed 02 0202|0202 Link to Article 2 + Escobar 02GJ, Gardner 02MN, Greene 02JD, Draper 02D, Kipnis 02P. 02Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system.02 Med Care . 2013;51(5):446-453. PubMed 02 0202|0202 Link to Article 3 + Gordon 02NP. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: statistics from the 2009 California Health Interview Survey. http://www.dor.kaiser.org/external/chis_non_kp_2009 . Accessed February 1, 2014. 4 + Agency for Healthcare Research and Quality. Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2010. http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2010.jsp . Accessed February 1, 2014. 5 + Iwashyna 02TJ, Odden 02A, Rohde 02J, 02et al. 02Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the International Consensus Conference definition of severe sepsis [published online September 18, 2012].02 Med Care . doi:10.1097/MLR.0b013e318268ac86. PubMed 6 + Liu 02V, Morehouse 02JW, Soule 02J, Whippy 02A, Escobar 02GJ. 02Fluid volume, lactate values, and mortality in sepsis patients with intermediate lactate values.02 Ann Am Thorac Soc . 2013;10(5):466-473. PubMed 02 0202|0202 Link to Article
Hepatic perfusion alterations in septic shock patients: impact of early goal-directed therapy
Early goal-directed therapy (EGDT) has become an important therapeutic management in early salvage stage of septic shock. However, splenic organs possibly remained hypoperfused and hypoxic despite fluid resuscitation. This study aimed to evaluate the effect of EGDT on hepatic perfusion in septic shock patients. A prospective observational study was carried out in early septic shock patients who were admitted to Intensive Care Unit within 24 h after onset and who met all four elements of the EGDT criteria after treatment with the standard EGDT procedure within 6 h between December 1, 2012 and November 30, 2013. The hemodynamic data were recorded, and oxygen metabolism and hepatic functions were monitored. An indocyanine green clearance test was applied to detect the hepatic perfusion. The patients’ characteristics were compared before treatment (T0), immediately after EGDT (T1), and 24 h after EGDT (T2). This study is registered at ClinicalTrials.org, NCT02060773. Twenty-one patients were included in the study; however, the hepatic perfusion data were not included in the analysis for two patients; therefore, 19 patients were eligible for the study. Hemodynamics data, as monitored by pulse-indicator continuous cardiac output, were obtained from 16 patients. There were no significant differences in indocyanine green plasma disappearance rate (ICG-PDR) and 15-min retention rate (R15) at T0 (11.9 ± 5.0%/min and 20.0 ± 13.2%), T1 (11.4 ± 5.1%/min and 23.6 ± 14.9%), and T2 (11.0 ± 4.5%/min and 23.7 ± 15.3%) (allP> 0.05). Both of the alterations of ICG-PDR and R15 showed no differences at T0, T1, and T2 in the patients of different subgroups that achieved different resuscitation goal numbers when elected (P> 0.05). There were no hepatic perfusion improvements after EGDT in the early phase of patients with septic shock. Clinicaltrials.gov NCT02060773 (https://clinicaltrials.gov/ct2/show/NCT02060773).
Fluid overload in patients with severe sepsis and septic shock treated with early-goal directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death
Goal-directed resuscitation for patients with early septic shock
Abstract BACKGROUND: Early goal-directed therapy (EGDT) has been endorsed in the guidelines of the Surviving Sepsis Campaign as a key strategy to decrease mortality among patients presenting to the emergency department with septic shock. However, its effectiveness is uncertain. METHODS: In this trial conducted at 51 centers (mostly in Australia or New Zealand), we randomly assigned patients presenting to the emergency department with early septic shock to receive either EGDT or usual care. The primary outcome was all-cause mortality within 90 days after randomization. RESULTS: Of the 1600 enrolled patients, 796 were assigned to the EGDT group and 804 to the usual-care group. Primary outcome data were available for more than 99% of the patients. Patients in the EGDT group received a larger mean (卤SD) volume of intravenous fluids in the first 6 hours after randomization than did those in the usual-care group (1964卤1415 ml vs. 1713卤1401 ml) and were more likely to receive vasopressor infusions (66.6% vs. 57.8%), red-cell transfusions (13.6% vs. 7.0%), and dobutamine (15.4% vs. 2.6%) (P<0.001 for all comparisons). At 90 days after randomization, 147 deaths had occurred in the EGDT group and 150 had occurred in the usual-care group, for rates of death of 18.6% and 18.8%, respectively (absolute risk difference with EGDT vs. usual care, -0.3 percentage points; 95% confidence interval, -4.1 to 3.6; P=0.90). There was no significant difference in survival time, in-hospital mortality, duration of organ support, or length of hospital stay. CONCLUSIONS: In critically ill patients presenting to the emergency department with early septic shock, EGDT did not reduce all-cause mortality at 90 days. (Funded by the National Health and Medical Research Council of Australia and the Alfred Foundation; ARISE ClinicalTrials.gov number, NCT00975793 .).
A randomized trial of protocol-based care for early septic shock
Trial of early, goal-directed resuscitation for septic shock
BACKGROUND Early, goal-directed therapy (EGDT) is recommended in international guidelines for the resuscitation of patients presenting with early septic shock. However, adoption has been limited, and uncertainty about its effectiveness remains. METHODS We conducted a pragmatic randomized trial with an integrated cost-effectiveness analysis in 56 hospitals in England. Patients were randomly assigned to receive either EGDT (a 6-hour resuscitation protocol) or usual care. The primary clinical outcome was all-cause mortality at 90 days. RESULTS We enrolled 1260 patients, with 630 assigned to EGDT and 630 to usual care. By 90 days, 184 of 623 patients (29.5%) in the EGDT group and 181 of 620 patients (29.2%) in the usual-care group had died (relative risk in the EGDT group, 1.01; 95% confidence interval [CI], 0.85 to 1.20; P=0.90), for an absolute risk reduction in the EGDT group of 0.3 percentage points (95% CI, 5.4 to 4.7). Increased treatment intensity in the EGDT group was indicated by increased use of intravenous fluids, vasoactive drugs, and red-cell transfusions and reflected by significantly worse organ-failure scores, more days receiving advanced cardiovascular support, and longer stays in the intensive care unit. There were no significant differences in any other secondary outcomes, including health-related quality of life, or in rates of serious adverse events. On average, EGDT increased costs, and the probability that it was cost-effective was below 20%. CONCLUSIONS In patients with septic shock who were identified early and received intravenous antibiotics and adequate fluid resuscitation, hemodynamic management according to a strict EGDT protocol did not lead to an improvement in outcome.
Early goal-directed therapy in severe sepsis and septic shock: insights and comparisons to ProCESS, ProMISe, and ARISE
Evolution of sepsis management: from early goal-directed therapy to personalized care
Hemodynamic therapy: timing and targeting
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
The correlation between CVP-derived parameters and the prognosis of critically ill patients
Abstract OBJECTIVE: To investigate the effect of central venous pressure on the organ dysfunction and prognosis of critically ill patients. METHODS: We conducted a retrospective observational cohort study of 488 ICU patients with central venous pressure and its derived parameters in a half-year period in one single ICU centre to compare the length of ICU stay, critical illness scores (SOFA and APACHE II), serum creatinine and lactate levels. RESULTS: The initial, peak and mean CVP levels of critically ill patients and length of ICU stay, peak lactate levels and SOFA scores were significantly correlated. While the peak CVP and peak creatinine levels were significantly correlated, the correlation of initial and mean CVP levels with peak creatinine was not significant. Subgroup analysis showed that in the patients with a peak CVP value above 12mmHg, the length of stay was significantly prolonged, organ function was significantly worse, and the SOFA score was significantly higher. ROC analysis showed peak levels of CVP above 11.5mmHg had the greatest ability to predict mortality of critically ill patients. CONCLUSION: Exposure to higher levels of central venous pressure in critically ill patients is associated with a poorer prognosis and worse organ function. Therefore, central venous pressure should be kept as low as possible during hemodynamic therapy in critically ill patients. Copyright 2017 Elsevier Inc. All rights reserved.
Elevated mean airway pressure and central venous pressure in the first day of mechanical ventilation indicated poor outcome
Early goal-directed therapy in the treatment of severe sepsis and septic shock
Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008
Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database
OBJECTIVE:: The Surviving Campaign guidelines recommend obtaining a serum measurement within 6 hours of presentation for all patients with suspected or septic shock. A greater than 4 mmol/L qualifies for administration of early quantitative resuscitation therapy. We evaluated elevation (with special attention to values > 4 mmol/L) and presence or absence of hypotension as a marker of clinical outcome. DESIGN AND SETTING:: The Surviving Campaign developed a database to assess the overall effect of the bundles as a performance improvement tool for clinical practice and patient outcome. This analysis focuses on one element of the Surviving Campaign's resuscitation bundle, measuring serum in adult or septic shock patients and its interaction with hypotension. This analysis was conducted on data submitted from January 2005 through March 2010. SUBJECTS:: Data from 28,150 subjects at 218 sites were analyzed. INTERVENTIONS:: None. MEASUREMENTS AND MAIN RESULTS:: Unadjusted analysis of the 28,150 observations from the Surviving Campaign database demonstrated a significant mortality increase with the presence of hypotension in conjunction with serum elevation greater than 2 mmol/L. On multivariable analysis, only values greater than 4 mmol/L, in conjunction with hypotension, significantly increased mortality when compared with the referent group of values less than 2 mmol/L and not hypotensive. Mortality was 44.5% in patients with combined greater than 4 mmol/L and hypotension when compared with 29% mortality in patients not meeting either criteria. CONCLUSIONS:: Serum was commonly measured within 6 hours of presentation in the management of or septic shock in this subset analysis of the Surviving Campaign database in accordance with the Surviving Campaign guidelines. Our results demonstrate that elevated levels are highly associated with in-hospital mortality. However, only patients who presented with values greater than 4 mmol/L, with and without hypotension, are significantly associated with in-hospital mortality and is associated with a significantly higher risk than intermediate levels (2-3 and 3-4 mmol/L). This supports the use of the cutoff of greater than 4 mmol/L as a qualifier for future clinical trials in or septic shock in patient populations who use quantitative resuscitation and the Surviving Campaign bundles as standard of care.
The effects of sepsis on mitochondria
Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016
Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality
Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease
Elevated central venous pressure is associated with impairment of microcirculatory blood flow in sepsis: a hypothesis generating post hoc analysis
Understanding central venous pressure: not a preload index?
Passive leg raising in Intensive Care Medicine
Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock
Septic cardiomyopathy
Hyperlactatemia and hypotension: looking at septic shock from different perspectives
The last decade has witnessed significant improvements in the treatment of patients with severe sepsis and septic shock, and a reduction in mortality from septic syndromes has been described by several epidemiological studies. Nevertheless, different inclusion cri- teria make it difficult to interpret and compare the data of the literature.
High versus low blood-pressure target in patients with septic shock
Ventriculoarterial decoupling in human septic shock
Introduction Septic shock is the most severe manifestation of sepsis. It is characterized as a hypotensive cardiovascular state associated with multiorgan dysfunction and metabolic disturbances. Management of septic shock is targeted at preserving adequate organ perfusion pressure without precipitating pulmonary edema or massive volume overload. Cardiac dysfunction often occurs in septic shock patients and can significantly affect outcomes. One physiologic approach to detect the interaction between the heart and the circulation when both are affected is to examine ventriculoarterial coupling, which is defined by the ratio of arterial elastance (Ea) to left ventricular end-systolic elastance (Ees). In this study, we analyzed ventriculoarterial coupling in a cohort of patients admitted to ICUs who presented with vs without septic shock. Methods In this retrospective cross-sectional opportunity study, we measured routine hemodynamics using indwelling arterial and pulmonary arterial catheters and transthoracic echocardiograms in 25 septic patients (group S) and 25 non???septic shock patients (group C) upon ICU admission. Ees was measured by echocardiography using a single-beat (EesSB) method. Ea was calculated as 0.9 systolic arterial pressure/stroke volume, and then the Ea/EesSB ratio was calculated (normal value <1.36). Results In group S, 21 patients had an Ea/EesSB ratio >1.36 (uncoupled). The four patients with Ea/EesSB ratios ???1.36 had higher EesSB values than patients with Ea/EesSB ratios >1.36 (P = 0.007), although Ea measurements were similar in both groups (P = 0.4). In group C, five patients had uncoupled Ea/EesSB ratios. No correlation was found between EesSB and left ventricular ejection fraction and between Ea/EesSB ratio and mixed venous oxygen saturation in septic shock patients. Conclusions Upon admission to the ICU, patients in septic shock often display significant ventriculoarterial decoupling that is associated with impaired left ventricular performance. Because Ea/Ees decoupling alters cardiovascular efficiency and cardiac energetic requirements independently of Ea or Ees, we speculate that septic patients with ventriculoarterial uncoupling may benefit from therapy aimed at normalizing the Ea/Ees ratio.
Use of central venous oxygen saturation to guide therapy
The use of pulmonary artery catheters has diminished, so that other technologies are emerging. Central venous oxygen saturation measurement (ScvO60) as a surrogate for mixed venous oxygen saturation measurement (SvO60) is simple and clinically accessible. To maximize the clinical utility of ScvO60 (or SvO60) measurement, it is useful to review what the measurement means in a physiologic context,how the measurement is made, important limitations, and how this measurement may be helpful in common clinical scenarios. Compared with cardiac output measurement, SvO60 is more directly related to tissue oxygenation. Furthermore,when tissue oxygenation is a clinical concern, SvO60 is less prone to error compared with cardiac output, where small measurement errors may lead to larger errors in interpreting adequacy of oxygen delivery. ScvO60 should be measured from the tip of a central venous catheter placed close to, or within, the right atrium to reduce measurement error. Correct clinical interpretation of SvO60, or its properly measured ScvO60 surrogate, can be used to (1) estimate cardiac output using the Fick equation, (2) better understand whether a patient's oxygen delivery is adequate to meet their oxygen demands, (3) help guide clinical practice, particularly when resuscitating patients using validated early goal directed therapy treatment protocols, (4) understand and treat arterial hypoxemia, and (5) rapidly estimate shunt fraction (venous admixture).
My patient has received fluid. How to assess its efficacy and side effects?
Many efforts have been made to predict, before giving fluid, whether it will increase cardiac output. Nevertheless, after fluid administration, it is also essential to assess the therapeutic efficacy and to look for possible adverse effects. Like for any drug, this step should not be missed. Basically, volume expansion is aimed at improving tissue oxygenation and organ function. To assess this final result, clinical signs are often unhelpful. The increase in urine output in case of acute kidney injury is a poor marker of the kidney perfusion improvement. Even if oxygen delivery has increased with fluid, the increase in oxygen consumption is not constant. Assessing this response needs to measure markers such as lactate, central/mixed venous oxygen saturation, or carbon dioxide-derived indices. If tissue oxygenation did not improve, one should check that cardiac output has actually increased with fluid administration. To assess this response, changes in arterial pressure are not reliable enough, and direct measurements of cardiac output are required. In cases where cardiac output did not increase with fluid, one should check that it was not due to an insufficient volume of fluid administered. For this purpose, volume markers of cardiac preload sometimes lack precision. The central venous pressure, in theory at least, should not augment to a large extent in fluid responders. The worst adverse effect of fluids is the increase in the cumulative fluid balance. In patients with acute respiratory distress syndrome (ARDS), the risk of aggravating pulmonary oedema should be systematically assessed by looking for increases in extravascular lung water, or, more indirectly, increases in central venous or pulmonary artery occlusion pressure. In ARDS patients receiving fluid, one should always keep in mind the risk of inducing/aggravating right ventricular dilation, which should be confirmed through echocardiography. The risk of increasing the intra-abdominal pressure should be carefully sought in patients at risk. Finally, fluid-induced haemodilution should not be neglected. Like for any drug which has inconsistent effectiveness and may exert significant harm, the correct fluid management should include a cautious and comprehensive assessment of fluid-induced benefits and side effects.