CHOLEDOCHAL cysts (CCs) are congenital abnormality of the biliary system. It is characterized by cystic dilatation of intrahepatic duct and extrahepatic biliary tree individually or both.1 According to the modified Todani system, CCs are classified into categories I-V. Type III is a rare form of CCs, also called choledochocele, which comprises only 4%-6% of all reported cases.2 It appears as a cystic dilatation of intramural segment of distal common bile duct protruding into duodenal lumen. Choledochocele has distinctive anatomic features and a lower risk of malignancy than other types.3-4 The clinical presentations and imaging findings of choledochocele resemble duodenal duplication cysts (DDCs), making their differential diagnosis difficult.5 Imaging examinations play an important role in the initial diagnosis, differential diagnosis, surgical planning and long term surveillance of CCs.6 The purpose of this study was to demonstrate the importance of magnetic resonance cholangiopancreatography (MRCP) and biliary specific contrast agents in the diagnosis of bile duct cyst.
CASE DESCRIPTION
A 42-year-old man was admitted to the Peking Union Medical College Hospital on October 29, 2015 for having been suffering from abdominal pain over one year. There was no significant medical history or family history. Physical examination did not show obvious abnormality. Laboratory data including complete blood count, urinalysis and blood biochemistry were within the normal limits.
In order to confirm the diagnosis, he underwent a series of imaging examinations. Ultrasonography did not show significantly positive signs. After symptomatic treatment, abdominal pain still appeared intermittently. Next, the patient underwent gastroscopy and endoscopic ultrasonography to make a definitive diagnosis. The results revealed a parenteral cystic lesion in the descending section of the duodenum. It was deemed as a duodenal diverticulum (Fig. 1). The upper gastrointestinal barium study displayed a round filling defect in the second portion of the duodenum (Fig. 2). Therefore we excluded the diagnosis of duodenal diverticulum. Abdomen CT revealed a thin-walled cystic mass without nodules causing mild duodenal dilatation and multiple stones in the duodenum (Fig. 3). We considered it as a type Ⅲ CC or a DDC. In order to confirm the relationship between the cystic lesion and the intestine, MRCP was performed with pineapple juice (PJ). PJ can significantly reduce the liquid in the intestinal cavity itself on T2 signal (Fig. 4). MRCP demonstrated the cystic lesion had no communication with the duodenal lumen. But this modality could not clearly identify its communication with the bile duct. During follow-up dynamic contrast enhancement (DCE)-MRI with specific liver intake contrast agent revealed a slender tube connecting the lower common bile duct with the cystic lesion (Fig. 4). Finally the patient was diagnosed with choledochocele based on imaging findings.
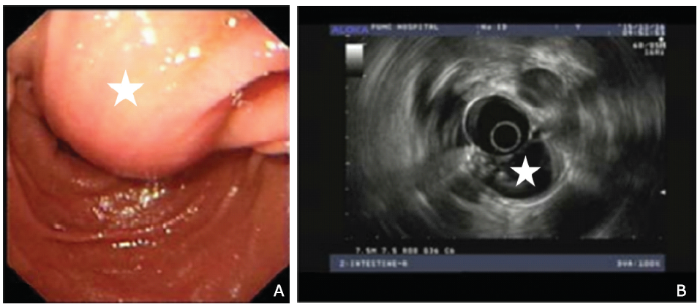
Figure 1.
Endoscopy (A) revealed a parenteral cystic lesion (star) in the descending duodenum. Endoscopic ultrasonography (B) showed a cystic lesion in the duodenal lumen with many stones (star).
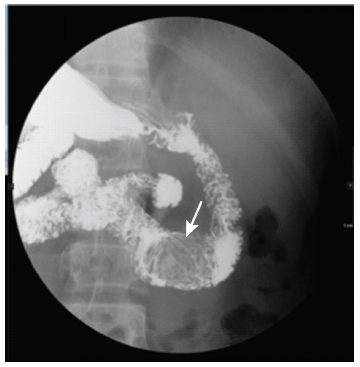
Figure 2.
The upper gastrointestinal barium study displayed a round filling defect (arrow) in the second portion of the duodenum.
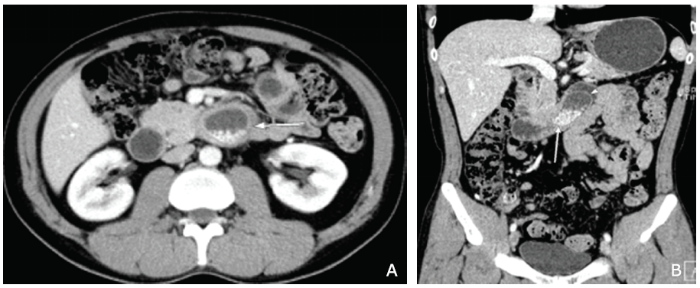
Figure 3.
Axial (A) and coronal (B) CT scan images of the abdomen revealing a cystic mass with multiple stones in the duodenum lumen (arrow). Coronal CT scan (B) showing a thin-walled cystic lesion (arrow) without nodules accompanied with mild duodenal dilatation.
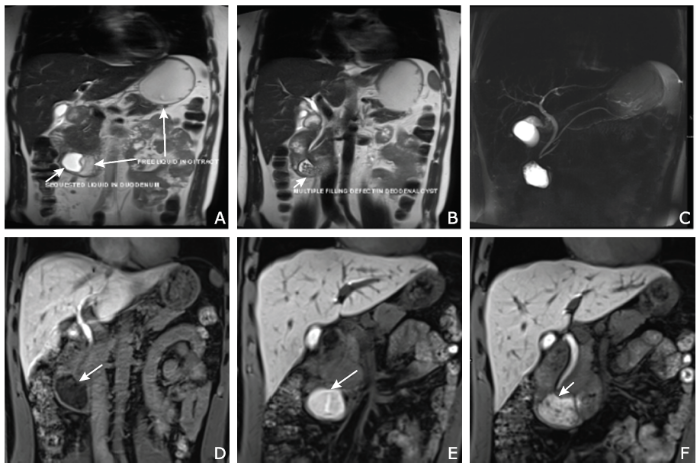
Figure 4.
Magnetic resonance cholangiopancreatography (MRCP) (A-C) and dynamic contrast enhancement (DCE)-MRI (D-F) images.
A. Pineapple juice can reduce the pre-existing gastrointestinal tract liquid (long arrow) in T2 signal and distinguish bowel water from liquid in the cystic lesion (short arrow) on T2WI.
B. MRCP showing multiple filling defects in the cystic cavity (arrow).
C. 2D MRCP.
D-F. DCE-MRI revealing the process of contrast medium excreted into the cystic lesion during discharge phase (arrows) and clearly displaying a slender tube (arrow, F) connecting the lower common bile duct with the cystic lesion.
The operation was carried out. The diagnosis was confirmed by pathological findings. He was discharged on postoperative day 10 with good health condition.
DISCUSSION
Type Ⅲ cyst is a rare type of CCs, characterized by a cystic dilatation of the bile duct terminal bulging into duodenal lumen.6-7 It is similar to DDCs, which also present as cystic structures and typically protrude into the second or third portion of the duodenum.8 DDCs are extremely rare6, 9 and account for 5% of all gastrointestinal duplications.10 DDCs are usually located in the mesenteric side and share their circumference with the intestine. They have a muscle coat and may or may not communicate with the gut lumen. Both CCs and DDCs can communicate with the bile duct. Except for connecting with the bile duct, DDCs can communicate with the pancreaticobiliary duct, especially with the pancreatic duct. They have much in common about clinical manifestations and imaging findings.11
It is difficult to distinguish them using preoperative diagnostic procedures. The key to differentiating them is to determine the relationship between the lesions and the lumen as well as bile duct. Cholangiography and upper gastrointestinal barium studies have been proposed to differentiate them. Choledochocele could be filled with contrast during cholangiography but not be filled during barium studies, whereas DDCs could not be filled when scanned with both studies.12 It may be sufficient to identify larger lesions with the two methods, but for smaller lesions the sensitivity and specificity of the two techniques are low. In addition, cholangiography is invasive. Recently the commonly used imaging techniques are ultrasonography, CT, MRCP and endoscopic retrograde cholangiopancreatography (ERCP) to verify CCs. Ultrasonography is economic, convenient and widely used, but it’s extremely susceptible to interference of bowel gas. Multi-detector computed tomography (MDCT) is very helpful in surgical planning, especially in the accurate delineation of extent of the dilated bile ducts. MDCT can also identify cyst wall thickening and intracystic masses that develop secondary to malignancy. But it’s difficult to display the relationship between cystic lesions and the bile ducts, duodenal lumen. MRCP and DCE-MRI well settle these problems with PJ and hepatocyte-specific contrast agent. PJ has shorter T1 and T2 than other juices. After oral PJ, fluid pre-existing in the lumen is suppressed, but liquid in the cystic cavity is still bright on T2WI.13 It can clearly show the relationship of the cystic lesion with the lumen. The liver specific contrast agent excreted by the bile duct can clearly show the relationship between the cystic lesion and bile ducts. Despite ERCP remains the most widely used diagnostic tool for identification of choledochocele, with a reported diagnostic sensitivity of 97%,5 it is invasive and the patients are difficult to tolerate. Nevertheless MRI is safe, non-invasive and no ionizing radiation. Furthermore, MRI does not carry the risks of ERCP including cholangitis, duodenal perforation, hemorrhage and pancreatitis. MRCP has distinct advantages to assess cyst lesions, size, site and shape of bile duct dilatation.14 The image quality of MRCP is more susceptible to motion artifacts than ERCP, which can be compensated by breath-hold sequences and respiratory triggered scanning.15 Sacher et al14 identified that MRCP has a 96%-100% detection rate for CCs, which making it the best choice for preoperative evaluation. MRI can entirely replace ERCP in assessing the relationship between the cystic lesion and bile duct, making guidance for surgical planning. This may benefit from PJ and liver specific contrast agent. It may be achieved in all patients with choledochocele who cannot be verified by ERCP. After a series of tests, the patient was diagnosed as type Ⅲ choledochal cyst by MRCP, and MRI with adminstration of the specific contrast agent of biliary tract confirmed the diagnosis. MRCP is noninvasive and convenient in the diagnosis of choledochocele.
Conflicts of interest statement
The authors have no conflicts of interest to disclose.
参考文献
Choledochal cysts: age of presentation, symptoms, and late complications related to Todani’s classification
Biliary cysts: etiology, diagnosis and management
Choledochal cysts: a review of literature
Choledochal cysts are cystic dilation of extrahepatic duct, intrahepatic duct, or both that may result in significant morbidity and mortality, unless identified early and managed appropriately. The incidence is common in Asian population compared with western counterpart with more than two third of the cases in Asia being reported from Japan. The traditional anatomic classification system is under debate with more focus on etiopathogenesis and other aspects of choledochal cysts. Even though categorized under the same roof, choledochal cysts vary with respect to their natural course, complications, and management. In this review, with the available literature on choledochal cysts, we discuss different views about the etiopathogenesis along with the natural course, complications, diagnosis, and surgical approach for choledochal cysts, which also explains why the traditional classification is questioned by some authors.
Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst
Diagnosis and treatment of choledochoceles
Choledochoceles are cystic dilatations of the intraduodenal portion of the common bile duct. Although often classified as Type III biliary cysts, choledochoceles have distinctive demographic and anatomic features and a lower risk of malignancy than other types of choledochal cysts. Type A choledochoceles are cystic dilatations of a segment of the intra-ampullary bile duct and are located proximal to the ampullary orifice. Type B choledochoceles are diverticula of the intra-ampullary common channel and are located distal to the ampullary orifice; they can bedistinguished from duodenal duplication cysts bothanatomically and histologically. Both types of choledochocele may present with pancreatitis, biliary obstruction, or nonspecific gastrointestinal symptoms. Cross-sectional imaging, endoscopic ultrasound, and endoscopic retrograde cholangiopancreatography are useful for diagnosis. Choledochoceles may be drained or resected endoscopically. Surveillance for dysplasia should be considered for lesions that are not resected.
Periampullary duodenal duplication cyst masquerading as a choledochocele
Enteric duplication cysts are rare congenital anomalies of unclear etiology. While they can occur anywhere in the gastrointestinal tract, they typically occur in the ileum or ileocecal region and very rarely in the duodenum. Here, we report a case of a periampullary duodenal duplication cyst in a 13-year-old male who presented with clinical and laboratory evidence of small bowel obstruction, hepatitis, and pancreatitis. Based on radiologic imaging, the patient was thought to have a type III choledochal cyst (choledochocele) within the duodenal lumen. Intraoperative findings and postoperative pathological evaluation, however, revealed that the lesion was a duodenal duplication cyst masquerading as a choledochal cyst. Interestingly, the duplication cyst was communicating with the common bile duct, simultaneously causing biliary and small bowel obstruction.
Adult choledochal cysts: current update on classification, pathogenesis and cross-sectional imaging findings
Ileal duplication cyst: Y-configuration on in vivo sonography
Although the double wall or muscular rim sign is considered to be a characteristic sonographic imaging finding of an enteric duplication cyst, this sign can also be produced by Meckel's diverticulum and sonographic artifacts. The Y-configuration on in vitro sonography has been reported to be useful for the definitive diagnosis of an enteric duplication cyst. Here, we report a case of an intraoperatively confirmed ileal duplication cyst that was correctly diagnosed before by identification of the Y-configuration on in vivo sonography.
Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations
A case series of symptomatic intraluminal duodenal duplication cysts: presentation, endoscopic therapy, and long-term outcome (with video)
Choledochal cysts in adults and their complications
Background Despite refinements in the management of choledochal cysts in children, an increasing number of patients present with ongoing symptoms in adult life. The aim of this study was to review the management of adult patients with choledochal cysts in a tertiary referral centre. Method A retrospective review was carried out of all adult patients presenting with choledochal cysts to this department between 1992 and 2000. Patient records were reviewed and detailed analyses were made of the clinical presentation, radiological and biochemical findings, anatomical anomalies, management, complications and outcomes. Results Of 16 patients (12 women and 4 men; median age 23 years), 8 had undergone previous upper gastrointestinal operations before referral, including 5 who had had previous cyst drainage procedures. All patients underwent elective complete cyst excision with Roux-en-Y hepaticojejunostomy. There were no operative deaths and there was a low early postoperative morbidity rate (25%). There was no evidence of biliary malignancy in any cyst. During a median postoperative follow-up of 44 months, five patients (31%) continued to experience cholangitis and two of these required additional revisional procedures, but are now symptom-free. Conclusion Patients with choledochal cysts should be referred to specialised tertiary surgical units. Total choledochal cyst excision with Roux-en-Y hepaticojejunostomy is the treatment of choice. Patients with previous inadequate cyst excisional procedures should undergo revisional surgery, to reduce recurrent symptoms and the risk of developing cholangiocarcinoma.
Colorectal duplication in adults: report of seven cases and review of the literature
Gastrointestinal duplications are uncommon congenital abnormalities, usually recognised before the age of 2 (80%). Colorectal duplications (CDDs) occur in only 6.8% of cases, rarely in adults, and are revealed by abdominal pain and intestinal obstruction. Malignant changes are uncommon, but are most often found in the colon. During the last 7 years, the authors have observed seven cases of CDD (three men) with mean age 50.7 years (range 32-73). Four cases were revealed by abdominal pain, and three by intestinal obstruction. Five duplications were located in the caecum, one in the transverse colon, and one in the sigmoid colon. All CDDs were of the cystic type (4.42 cm, range 2-7.5), and three had a communication with the intestinal lumen. All patients except one underwent 'en bloc' resection of the cyst with the adjacent colon. On microscopic examination, CDDs contained multiple layers of the bowel wall, including colonic or small intestinal mucosa. Heterotopic gastric mucosa was observed in only one case, high-grade dysplasia in one case, and low-grade dysplasia in another. No invasive carcinoma was found. Although uncommon, CDDs should be included in the differential diagnosis of all abdominal masses. The treatment approach is excision, in order to avoid any complication. En bloc resection of the colon with CDD may be necessary, because of the intimate attachments of the common wall. Thorough sampling of the specimen is mandatory in order to detect any malignant changes.
Interactive neonatal gastrointestinal magnetic resonance imaging using fruit juice as an oral contrast media
Role of magnetic resonance cholangiopancreatography in diagnosing choledochal cysts: case series and review