Chinese Medical Sciences Journal ›› 2023, Vol. 38 ›› Issue (2): 117-124.doi: 10.24920/004158
• Original Article • Previous Articles Next Articles
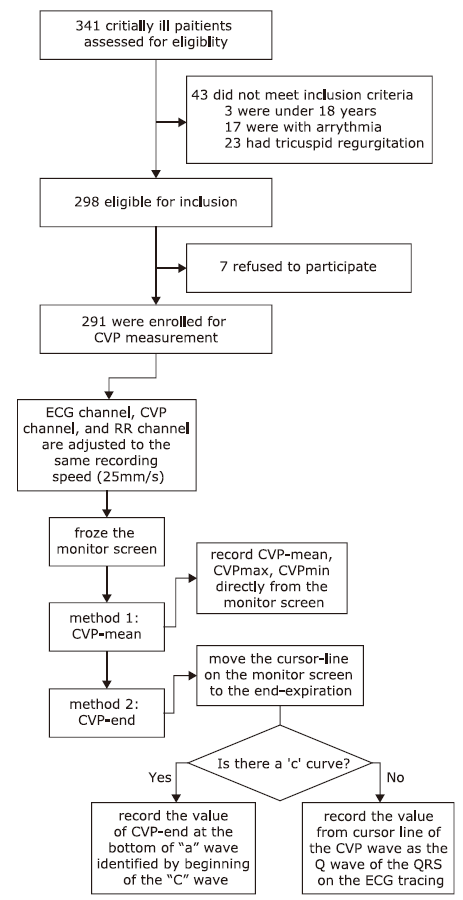
Accuracy of Mean Value of Central Venous Pressure from Monitor Digital Display: Influence of Amplitude of Central Venous Pressure during Respiration
Meng-Ru Xu1, Wang-Lin Liu1, Huai-Wu He1, *( ), Xiao-Li Lai2, Mei-Ling Zhao3, Da-Wei Liu1, Yun Long1
), Xiao-Li Lai2, Mei-Ling Zhao3, Da-Wei Liu1, Yun Long1
- 1Department of Critical Care Medicine, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Beijing 100730, China
2Department of Critical Care Medicine, Beihai People's Hosptial, Beihai 536000, Guangxi Zhuang Autonomous Region, China
3Department of Critical Care Medicine, Zibo Central Hospital, Medical College of Shandong University, Zibo 255020, Shandong Province, China
-
Received:2022-08-23Accepted:2023-03-20Published:2023-06-30Online:2023-04-13 -
Contact:*Huai-Wu He, E-mail:tjmuhhw@126.com.
These authors contributed equally to this work.
Cite this article
Meng-Ru Xu, Wang-Lin Liu, Huai-Wu He, Xiao-Li Lai, Mei-Ling Zhao, Da-Wei Liu, Yun Long. Accuracy of Mean Value of Central Venous Pressure from Monitor Digital Display: Influence of Amplitude of Central Venous Pressure during Respiration[J].Chinese Medical Sciences Journal, 2023, 38(2): 117-124.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1.
Characteristics of the subjects (n=291)"
| Parameters | Total |
|---|---|
| Age (years) | 57.32 ± 16.18 |
| Sex (male/female) | 159/132 |
| Heart rate (bpm) | 92 ± 18 |
| Mean arterial pressure (mmHg) | 90 ± 14 |
| CVP-mean (mmHg) | 7.69 ± 3.10 |
| CVP-end (mmHg) | 8.26 ± 3.23 |
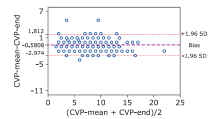
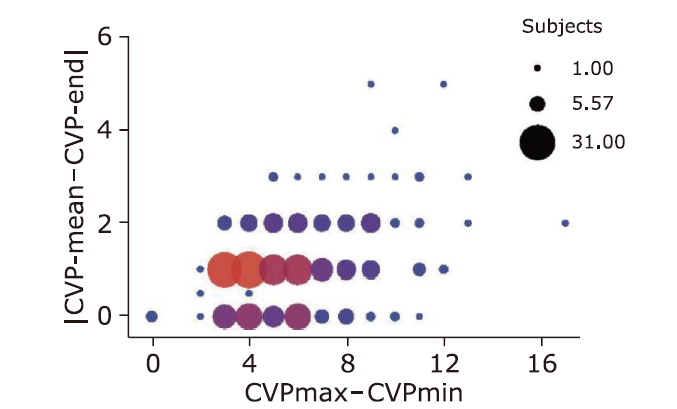
| |CVP-mean-CVP-end| (mmHg) | 1.03 ± 0.87 |
| CVPmax (mmHg) | 11.07 ± 3.58 |
| CVPmin (mmHg) | 5.36 ± 3.12 |
| CVPmax-CVPmin (mmHg) | 5.71 ± 2.48 |
Table 2.
Comparisons between consistent and inconsistent groups"
| Parameters | Inconsistent group (n=72) | Consistent group (n=219) | Statistics | P value |
|---|---|---|---|---|
| Age (years) | 56.44 ± 15.87 | 57.68 ± 16.33 | t = 0.30 | 0.544 |
| HR (bpm) | 93 ± 18 | 92 ± 18 | t = 0.13 | 0.961 |
| MAP (mmHg) | 89 ± 13 | 90 ± 14 | t = 0.51 | 0.773 |
| Pts with/without spontaneous breath | 59/13 | 146/73 | χ2 = 5.4 | 0.014* |
| CVP-mean (mmHg) | 7.72 ± 4.05 | 7.67 ± 2.74 | t = 0.15 | 0.787 |
| CVP-end (mmHg) | 9.38 ± 4.16 | 7.90 ± 2.78 | t = 3.41 | 0.004* |
| |CVP-mean-CVP-end|(mmHg) | 2.25 ± 0.63 | 0.635 ± 0.48 | t = 22.92 | <0.0001* |
| CVPmax (mmHg) | 12.04 ± 4.39 | 10.75 ± 3.22 | t = 2.67 | 0.014* |
| CVPmin (mmHg) | 4.88 ± 4.05 | 5.52 ± 2.75 | t = 1.51 | 0.196 |
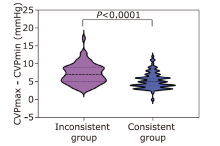
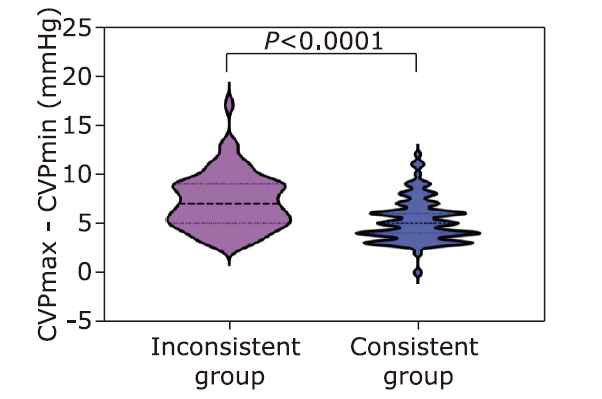
| CVPmax-CVPmin (mmHg) | 7.17 ± 2.77 | 5.24 ± 2.18 | t = 6.07 | <0.0001* |
| 1 |
Berlin DA, Bakker J. Starling curves and central venous pressure. Crit Care 2015 ; 19(1): 55. doi:10.1186/s13054-015-0776-1.
doi: 10.1186/s13054-015-0776-1 |
| 2 |
Long Y, Su LX, Zhang Q, et al. Elevated mean airway pressure and central venous pressure in the first day of mechanical ventilation indicated poor outcome. Crit Care Med 2017 ; 45(5): e485-92. doi: 10.1097/CCM.0000000000002290.
doi: 10.1097/CCM.0000000000002290 |
| 3 |
Magder S. Right atrial pressure in the critically ill how to measure, what is the value, what are the limitations? Chest 2017 ; 151(4): 908-16. doi:10.1016/j.chest.2016.10.026.
doi: 10.1016/j.chest.2016.10.026 |
| 4 |
Chen H, Zhu Z, Zhao C, et al. Central venous pressure measurement is associated with improved outcomes in septic patients: an analysis of the MIMIC-III database. Crit Care (London, England) 2020 ; 24(1):433. doi:10.1186/s13054-020-03109-9.
doi: 10.1186/s13054-020-03109-9 |
| 5 |
Wang XT, Yao B, Liu DW, et al. Central venous pressure dropped early is associated with organ function and prognosis in septic shock patients: a retrospective observational study. Shock 2015 ; 44(5):426-30. doi:10.1097/shk.0000000000000445.
doi: 10.1097/shk.0000000000000445 |
| 6 |
Li DK, Du W. Central venous pressure value can assist in adjusting norepinephrine dosage after the initial resuscitation of septic shock. Chin Med J (Engl) 2019 ; 132(10): 1159-65. doi:10.1097/cm9.0000000000000238.
doi: 10.1097/cm9.0000000000000238 |
| 7 |
Yang Q, Chen W, Wen Y, et al. Association between wait time of central venous pressure measurement and outcomes in critical patients with acute kidney injury: a retrospective cohort study. Front Public Health 2022; 10: 893683. doi:10.3389/fpubh.2022.893683.
doi: 10.3389/fpubh.2022.893683 |
| 8 |
Tang R, Peng JN, Wang DX. Central venous pressure measurement is associated with improved outcomes in patients with or at risk for acute respiratory distress syndrome: an analysis of the Medical Information Mart for Intensive Care IV Database. Front Med (Lausanne) 2022; 9: 858838. doi:10.3389/fmed.2022.858838.
doi: 10.3389/fmed.2022.858838 |
| 9 | Hu B, Xiang H, Liang H, et al. Assessment effect of central venous pressure in fluid resuscitation in the patients with shock: a multi-center retrospective research. Chin Med J (Engl) 2013 ; 126(10): 1844-9. |
| 10 |
Backer DD, Vincent JL. Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care 2018; 22. doi:10.1186/s13054-018-1959-3.
doi: 10.1186/s13054-018-1959-3 |
| 11 |
Backer DD, Cecconi M, Chew MS, et al. A plea for personalization of the hemodynamic management of septic shock. Crit Care 2022 ; 26(1):372. doi:10.1186/s13054-022-04255-y.
doi: 10.1186/s13054-022-04255-y |
| 12 |
Legrand M, Soussi S, Depret F. Cardiac output and CVP monitoring... to guide fluid removal. Crit Care 2018; 22. doi:10.1186/s13054-018-2016-y.
doi: 10.1186/s13054-018-2016-y |
| 13 |
Backer DD, Aissaoui N, Cecconi M, et al. How can assessing hemodynamics help to assess volume status? Intensive Care Med 2022 ; 48(10):1482-94. doi:10.1007/s00134-022-06808-9.
doi: 10.1007/s00134-022-06808-9 |
| 14 | Reems MM and M Aumann. Central venous pressure: principles, measurement, and interpretation. Compendium (Yardley, PA) 2012 ; 34(1): E1. |
| 15 |
Pasion E, Good L, Tizon J, et al. Evaluation of the monitor cursor-line method for measuring pulmonary artery and central venous pressures. Am J Crit Care 2010 ; 19(6):511-21. doi:10.4037/ajcc2010502.
doi: 10.4037/ajcc2010502 |
| 16 |
Kleinman B, Powell S, Kumar P, et al. The fast flush test measures the dynamic response of the entire blood pressure monitoring system. Anesthesiology 1992 ; 77(6):1215-20. doi:10.1097/00000542-199212000-00024.
doi: 10.1097/00000542-199212000-00024 |
| 17 |
Watanabe H, Yagi SI, Namiki A. Recommendation of a clinical impulse response analysis for catheter calibration-dumping coefficient and natural frequency are incomplete parameters for clinical evaluation. J Clin Monit Comput 2006 ; 20(1): 37-42. doi:10.1007/S10877-005-9008.
doi: 10.1007/S10877-005-9008 |
| 18 |
Roger C, Muller L, Riou B, et al. Comparison of different techniques of central venous pressure measurement in mechanically ventilated critically ill patients. Br J Anaesth 2017 ; 118(2):223-31. doi:10.1093/bja/aew386.
doi: 10.1093/bja/aew386 |
| 19 |
Hamzaoui O, Teboul JL. Central venous pressure (CVP). Intensive Care Med 2022 ; 48(10): 1498-500. doi:10.1007/s00134-022-06835-6.
doi: 10.1007/s00134-022-06835-6 |
| 20 |
Lakhal K, Ehrmann S, Runge I, et al. Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Medicine 2010 ; 36(6):940-8. doi:10.1007/s00134-010-1755-2.
doi: 10.1007/s00134-010-1755-2 |
| 21 | AACN practice alert: PA/CVP Monitoring in Adults. 2016; Available from: www.aacn.org/clinical-resources/practice-alerts/pulmonary-artery-pressure-measurement. |
| 22 |
Jain RK, Antonio BL, Bowton DL, et al. Variability in central venous pressure measurements and the potential impact on fluid management. Shock 2010 ; 33(3): 253-7. doi: 10.1097/SHK.0b013e3181b2bb22.
doi: 10.1097/SHK.0b013e3181b2bb22 |
| [1] | Zhang Hongmin, Wang Xiaoting, Zhang Qing, Liu Dawei. Resuscitation of Septic Patients with Target-and-endpoint Protocol: A Retrospective Study from a Chinese Tertiary Hospital ICU [J]. Chinese Medical Sciences Journal, 2018, 33(3): 135-142. |
| [2] | Liang Shan*,Rui Zhang, Lian-di Li. Effect of Timing of Tracheotomy on Clinical Outcomes: an Update Meta-analysis Including 11 Trials [J]. Chinese Medical Sciences Journal, 2013, 28(3): 159-166. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|