Chinese Medical Sciences Journal ›› 2023, Vol. 38 ›› Issue (3): 228-234.doi: 10.24920/004252
• Original Article • Previous Articles Next Articles
In-hospital Mortality and Hospital Outcomes among Adults Hospitalized for Exacerbations of Asthma and COPD in Southern Thailand (2017-2021): A Population-Based Study
Narongwit Nakwan1, *( ), Kanittha Suansan2
), Kanittha Suansan2
- 1Division of Pulmonology, Department of Medicine, Hat Yai Medical Education Center, Hat Yai Hospital, Songkhla, Thailand
2National Heath Security Office (NHSO), Region 12, Thailand
-
Received:2023-05-05Accepted:2023-06-26Published:2023-09-30Online:2023-09-04 -
Contact:* E-mail:naronak@hotmail.com .
Cite this article
Narongwit Nakwan, Kanittha Suansan. In-hospital Mortality and Hospital Outcomes among Adults Hospitalized for Exacerbations of Asthma and COPD in Southern Thailand (2017-2021): A Population-Based Study[J].Chinese Medical Sciences Journal, 2023, 38(3): 228-234.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1.
Characteristics and overall admissions for asthma and COPD exacerbations in southern Thailand during 2017-2021"
| Iterms | All | Asthma | All | COPD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | 2021 | 2017 | 2018 | 2019 | 2020 | 2021 | |||
| Total hospital admission (n) | 19,459 | 4,126 | 4,182 | 4,316 | 3,958 | 2,877 | 66,457 | 14,419 | 14,558 | 14,692 | 12,499 | 10,289 |
| Total patients admitted (n) | 9,486 | 2,838 | 2,889 | 2,989 | 2,707 | 2,013 | 19,767 | 6,780 | 6,883 | 6,902 | 6,166 | 5,127 |
| Age [yrs, mean (SD)] | 51.8 (17.7) | 51.5 (17.1) | 51.4 (18.4) | 51.9 (17.4) | 51.5 (18.2) | 52.7 (17.5) | 69.5 (11.3) | 69.9 (11.2) | 69.5 (17.1) | 69.2 (11.2) | 69.2 (11.5) | 69.1 (11.5) |
| Age group (yrs, n) | ||||||||||||
| 15-40 | 5,085 | 1,046 | 1,132 | 1,074 | 1,093 | 740 | 662 | 116 | 142 | 137 | 158 | 111 |
| 41-60 | 7,956 | 1,759 | 1,700 | 1,807 | 1,551 | 1,139 | 13,148 | 2,693 | 2,818 | 3,971 | 2,572 | 2,904 |
| 61-75 | 4,649 | 957 | 964 | 1,050 | 940 | 738 | 31,061 | 6,731 | 6,893 | 6,909 | 5,771 | 4,757 |
| > 75 | 1,769 | 364 | 386 | 387 | 374 | 260 | 21,586 | 4,881 | 705 | 4,675 | 3,998 | 3,327 |
| Gender (%) | ||||||||||||
| Male | 22.2 | 20.9 | 21.3 | 21.3 | 23.3 | 25.3 | 78.3 | 76.9 | 77.0 | 78.3 | 79.5 | 80.1 |
| Female | 77.8 | 79.1 | 78.7 | 78.7 | 76.7 | 74.7 | 21.7 | 23.1 | 23.0 | 21.7 | 20.5 | 29.9 |
Table 2.
The in-hospital outcomes of asthma exacerbation in Southern Thailand (2017-2021)"
| Items | Average | Fiscal year | ||||
|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | 2021 | ||
| Age-adjusted asthma hospitalization per 100,000 population | 130 | 139 | 141 | 145 | 132 | 95 |
| Age-adjusted asthma mortality rate per 100,000 population | 0.44 | 0.41 | 0.44 | 0.44 | 0.47 | 0.43 |
| Case fatality rate per 1,000 hospital admissions | 3.4 | 3.2 | 2.9 | 3.3 | 3.7 | 3.7 |
| 15-40 years | 3 | 4.7 | 1.7 | 4.6 | 0 | 4.1 |
| 41-60 years | 3.4 | 1.7 | 2.9 | 1.1 | 2.5 | 8.7 |
| 61-75 years | 3.8 | 2.1 | 3.1 | 1.9 | 6.3 | 5.4 |
| >75 years | 10.7 | 5.5 | 7.7 | 10.3 | 10.6 | 19.2 |
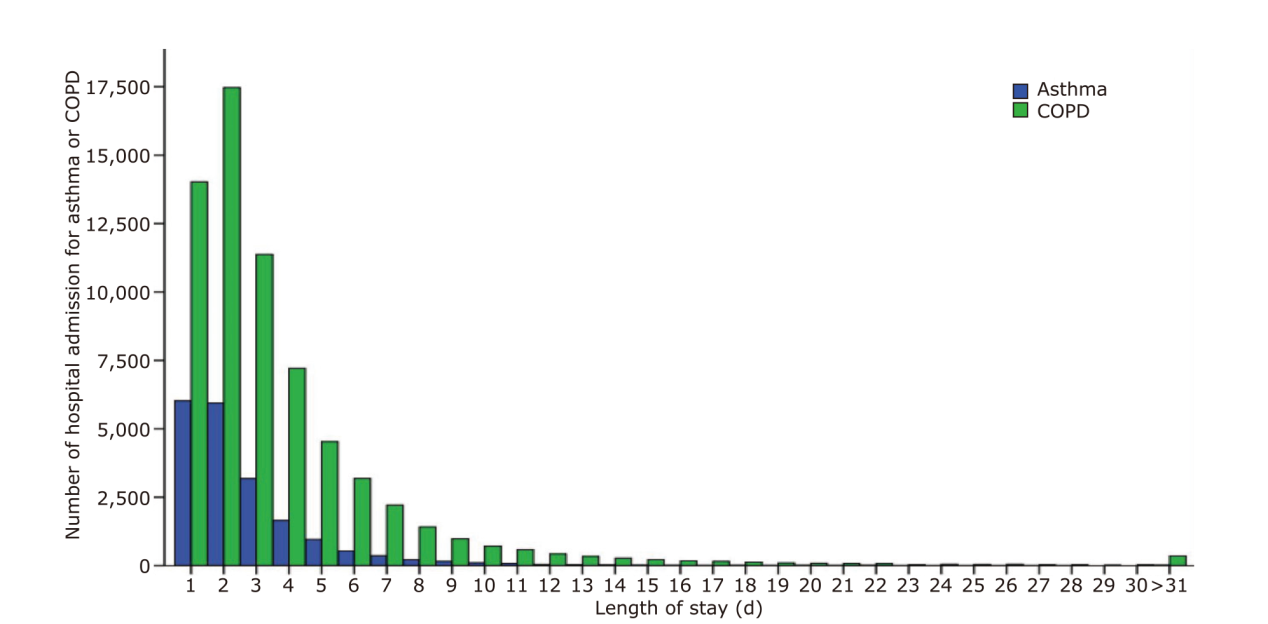
| Length of stay [d, mean (range)] | 2.77 (1-95) | 2.82 (1-57) | 2.82 (1-37) | 2.76 (1-39) | 2.68 (1-95) | 2.74 (1-48) |
| Reimbursement per admission [Baht, mean (range)] | 5,084 (963-232,454) | 4,696 (963-232,454) | 4,601 (1,116-209,531) | 5,059 (1,089-216,163) | 5,197 (1,102-216,916) | 6,227 (1,254-131,309) |
| Total reimbursement of the year (Baht) | NA | 19,368,452 | 19,242,761 | 21,835,004 | 20,571,843 | 17,916,073 |
Table 3.
The in-hospital outcomes of COPD exacerbation in southern Thailand (2017-2021)."
| Iterms | average | Fiscal year | ||||
|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | 2021 | ||
| Age-adjusted COPD hospitalization per 100,000 population | 446 | 487 | 492 | 494 | 417 | 340 |
| Age-adjusted COPD mortality rate per 100,000 population | 8.3 | 10.2 | 8.7 | 8.8 | 7.2 | 6.6 |
| Case fatality rate per 1,000 hospital admission | 18.6 | 20.3 | 17.6 | 17.8 | 16.4 | 21.8 |
| 15-40 years | 3.7 | 8.7 | 1.4 | 2.2 | 6.3 | 0 |
| 41-60 years | 9.2 | 11.5 | 7.4 | 9.7 | 9.7 | 7.6 |
| 61-75 years | 16.2 | 17.3 | 15.3 | 15.6 | 17.3 | 15.7 |
| >75 years | 27.9 | 31.5 | 27.4 | 25.8 | 22.5 | 33.1 |
| Length of stay [d, mean (range)] | 3.98 (1-228) | 4.10 (1-228) | 4.01 (1-200) | 3.93 (1-196) | 3.84 (1-186) | 3.85 (1-95) |
| Reimbursement per admission [Baht, mean (range)] | 10,045 (1,111-509,763) | 9,158 (1,020-275,488) | 9,537 (1,111-276,488) | 10,259 (1,188-255,559) | 9,868 (860-251,559) | 12,148 (1,252-509,763) |
| Total reimbursement of the year (Baht) | NA | 131,905,909 | 138,708,376 | 150,689,175 | 123,288,259 | 123,005,492 |
| 1 | Global Initiative for Asthma GINA. Global strategy for asthma management and prevention, updated 2023. Available from http://www.ginasthma.org, 2022. Accessed: November 1, 2022. |
| 2 | Global Initiative for Chronic Obstructive Lung Disease GOLD. Global strategy for prevention, diagnosis and management of copd, updated 2022. Available from https://goldcopd.org/2022-gold-report-2. Accessed: November 1, 2022. |
| 3 | Kaur BP, Lahewala S, Arora S, et al. Asthma: hospitalization trends and predictor of in-hospitality and hospitalization costs in the USA (2001-2010)[J]. Int Arch Allergy Immunol 2015; 168: 71-8. doi:10.1159/000441687. |
| 4 | Inmai PN, Liabsuetrakul T, Ichihara N, et al. Health effects of the asthma care program under the universal coverage scheme in children and young adults in Thailand[J]. Int J Environ Res Public Health. 2022; 19(7): 4130. doi:10.3390/ijerph19074130. |
| 5 |
Lima FV, Yen TY, Patel JK. Trends in in-hospital outcomes among adults hospitalized with exacerbation of chronic obstructive pulmonary disease[J]. COPD 2015; 12(6): 636-42. doi:10.3109/15412555.2015.1020151.
pmid: 26263035 |
| 6 | Krishnan V, Diette GB, Rand CS, et al. Mortality in patients hospitalized for asthma exacerbations in the United States[J]. Am J Respir Crit Care Med. 2006; 174(6): 633-8. doi:10.1164/rccm.200601-007OC. |
| 7 |
Kirenga BJ, de Jong C, Mugenyi L, et al. Rates of asthma exacerbations and mortality and associated factors in Uganda: a 2-year prospective cohort study[J]. Thorax 2018; 73(10): 983-5. doi:10.1136/thoraxjnl-2017-211157.
pmid: 29752346 |
| 8 | Shah SA, Quint JK, Sheikh A. Impact of COVID-19 pandemic on asthma exacerbations: retrospective cohort study of over 500,000 patients in a national English primary care database[J]. Lancet Reg Health Eur. 2022; 19: 100428 doi: 10.1016/j.lanepe.2022.100428. |
| 9 | Chan KF, Kwok WC, Ma TF, et al. Territory-wide study on hospital admissions for asthma exacerbations in the COVID-19 pandemic[J]. Ann Am Thorac Soc 2021; 18(10): 1624-33. doi:10.1513/AnnalsATS.202010-1247OC. |
| 10 | Poucineau J, Delory T, Lapidus N, et al. Hospital admissions and mortality for acute exacerbations of COPD during the COVID-19 pandemic: a nationwide study in France[J]. Front Med (Lausanne) 2022; 9: 995016. doi: 10.3389/fmed.2022.995016. |
| 11 | Alqahtani JS, Oyelade T, Aldhahir AM, et al. Reduction in hospitalised COPD exacerbations during COVID-19: a systematic review and meta-analysis[J]. PLoS One 2021; 16(8):e0255659. doi:10.1371/journal.pone.0255659. |
| 12 |
Ekström M, Nwaru BI, Wiklund F, et al. Risk of rehospitalization and death in patients hospitalized due to asthma[J]. J Allergy Clin Immunol Pract 2021; 9(5): 1960-8.e4. doi:10.1016/j.jaip.2020.12.030.
pmid: 33359587 |
| 13 |
Singanayagam A, Schembri S, Chalmers JD. Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease[J]. Ann Am Thorac Soc 2013; 10(2): 81-9. doi:10.1513/AnnalsATS.201208-043OC.
pmid: 23607835 |
| 14 | Sykes DL, Faruqi S, Holdsworth L, et al. Impact of COVID-19 on COPD and asthma admissions, and the pandemic from a patient’s perspective[J]. ERJ Open Res 2021; 7(1): 00822-2020. doi:10.1183/23120541.00822-2020. |
| 15 | Sunjaya AP, Allida SM, Tanna GLD, et al. Asthma and COVID-19 risk: a systematic review and meta-analysis[J]. Eur Respir J 2022; 59(3): 2101209. doi: 10.1183/13993003.01209-2021. |
| 16 | Pardhan S, Wood S, Vaughan M, et al. The Risk of COVID-19 related hospitalsation, intensive care unit admission and mortality in people with underlying asthma or COPD: a systematic review and meta-analysis[J]. Front Med (Lausanne) 2021; 8: 668808. doi: 10.3389/fmed.2021.668808. |
| 17 | Tydeman F, Pfeffer PE, Vivaldi G, et al. Rebound in asthma exacerbations following relaxation of COVID-19 restrictions: a longitudinal population-based study (COVIDENCE UK)[J]. Thorax 2023; 78(8): 752-9. doi:10.1136/thorax-2022-219591. |
| 18 |
Ehteshami-Afshar S, FitzGerald JM, Doyle-Waters MM, et al. The global economic burden of asthma and chronic obstructive pulmonary disease[J]. Int J Tuberc Lung Dis 2016; 20: 11-23. doi:10.5588/ijtld.15.0472.
pmid: 26688525 |
| 19 | Ford ES, Murphy LB, Khavjou O, et al. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥18 years in the United States for 2010 and projections through 2020[J]. Chest 2015; 147(1): 31-45. doi: 10.1378/chest.14-0972. |
| 20 |
Dalal AA, Shah M, D’Souza AO, et al. Costs of COPD exacerbations in the emergency department and inpatient setting[J]. Respir Med. 2011; 105(3): 454-60. doi:10.1183/09059180.06.00009802.
pmid: 20869226 |
| 21 |
Woo L, Smith HE, Sullivan SD. The economic burden of chronic obstructive pulmonary disease in the Asia-Pacific region: a systematic review[J]. Value Health Reg Issues 2019; 18: 121-31.
doi: S2212-1099(19)30046-9 pmid: 31051330 |
| 22 |
Lai CKW, Kim YY, Kuo SH, et al. Cost of asthma in the Asia-Pacific region[J]. Eur Respir Rev 2006; 15 (98): 10-6.
doi: 10.1183/09059180.06.00009802 |
| [1] | Yu Gu, Ting Zhang, Min Peng, Juhong Shi. Characteristics and Prognosis of Microscopic Polyangiitis Patients with Diffuse Alveolar Hemorrhage and Interstitial Lung Disease [J]. Chinese Medical Sciences Journal, 2022, 37(4): 293-302. |
| [2] | Bin Wu,Jianghua Zhou,Wenxin Wang,Huilin Yang,Meng Xia,Binghong Zhang,Zhigang She,Hongliang Li. Association Analysis of Hyperlipidemia with the 28-Day All-Cause Mortality of COVID-19 in Hospitalized Patients [J]. Chinese Medical Sciences Journal, 2021, 36(1): 17-26. |
| [3] | Zhu Weihua,Xie Wenyong,Zhang Zhedong,Li Shu,Zhang Dafang,Liu Yijun,Zhu Jiye,Leng Xisheng. Postoperative Complications and Survival Analysis of Surgical Resection for Hilar Cholangiocarcinoma: A Retrospective Study of Fifty-Nine Consecutive Patients [J]. Chinese Medical Sciences Journal, 2020, 35(2): 157-169. |
| [4] | Jing Yang, Mei-cen Zhou, Kai Feng, Ou Wang, Hua-bing Zhang, Wei Li, Fan Ping, Jing Yang, Yu-xiu Li. Clinical Characteristics of 261 Cases of Hospitalized Patients with Type 1 Diabetes Mellitus [J]. Chinese Medical Sciences Journal, 2016, 31(2): 69-75. |
| [5] | Rui-e Feng, Wen-bing Xu, Ju-hong Shi, Artin Mahmoudi, Wen-bing Mu, Wen-jie Zheng, Yuan-jue Zhu, and Hong-rui Liu. Pathological and High Resolution CT Findings in Churg-Strauss Syndrome [J]. Chinese Medical Sciences Journal, 2011, 26(1): 1-8. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|