Chinese Medical Sciences Journal ›› 2018, Vol. 33 ›› Issue (2): 84-90.doi: 10.24920/11810
• Original Article • Previous Articles Next Articles
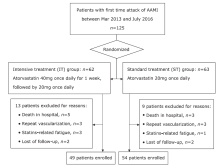
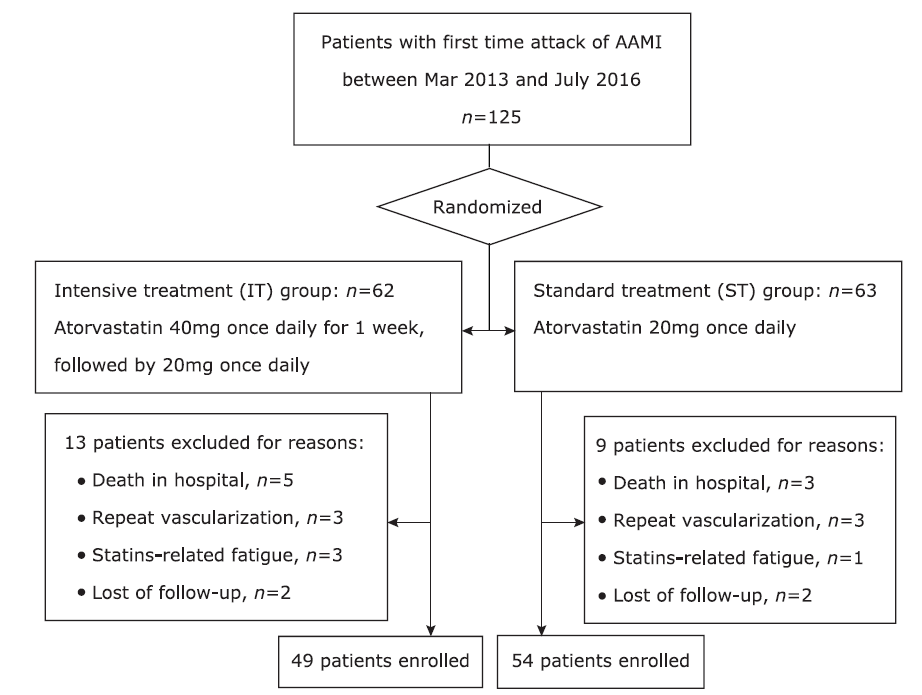
Effects of Short-term High Dose Atorvastatin on Left Ventricular Remodeling in Patients with First Time Attack of Anterior Acute Myocardial Infarction
Liu Zhijian1, Hu Gaopin1, Fei Meiying1, Yin Zao2, Shi Quanxing2, Sun Fei1, *( )
)
- 1 Department of Cardiology, the 210th Hospital of People’s Liberation Army, Dalian, Liaoning 116021, China;
2 Department of Cardiology, the 306th Hospital of People’s Liberation Army, Beijing 100101, China;
-
Received:2017-11-07Published:2018-06-30Online:2018-06-07 -
Contact:Sun Fei E-mail:doufangjie@126.com
Cite this article
Liu Zhijian, Hu Gaopin, Fei Meiying, Yin Zao, Shi Quanxing, Sun Fei. Effects of Short-term High Dose Atorvastatin on Left Ventricular Remodeling in Patients with First Time Attack of Anterior Acute Myocardial Infarction[J].Chinese Medical Sciences Journal, 2018, 33(2): 84-90.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
"
| Clinical characteristics | ST group (n=54) | IT group (n=49) | t/χ | P value |
|---|---|---|---|---|
| Age, years | 64±11 | 61±10 | 1.188 | 0.239 |
| Gender | ||||
| Male, n (%) | 35(64.8) | 33(67.3) | 0.073 | 0.682 |
| Female, n (%) | 19(35.2) | 16(32.7) | ||
| Risk factors | ||||
| Hypertension, n (%) | 15(27.8) | 16(32.7) | 0.290 | 0.590 |
| Diabetes Mellitus, n (%) | 13(24.1) | 10(20.4) | 0.199 | 0.655 |
| smoking, n (%) | 21(38.9) | 14(28.6) | 1.219 | 0.270 |
| Laboratory parameters | ||||
| HDL-C, mmol/L | 1.57±0.36 | 1.66±0.38 | 1.014 | 0.315 |
| LDL-C, mmol/L | 3.24±0.75 | 3.11±0.75 | 0.774 | 0.466 |
| Peak CK-MB, U/L | 188.8±135.5 | 221.0±141.6) | 0.872 | 0.352 |
| PCI parameters | ||||
| Time from onset to revascularization, min | 387±174 | 327±168 | 0.726 | 0.161 |
| Single-vessel /multi-vessel | 41/13 | 35/14 | 0.269 | 0.604 |
| Contrast media volume, ml | 142±29 | 154±38 | 1.512 | 0.135 |
| Medications after PCI | ||||
| Aspirin, n (%) | 54(100) | 49(100) | NA | NA |
| Clopidogrel, n (%) | 54(100) | 49(100) | NA | NA |
| Beta blockers, n (%) | 46(85.2) | 40(81.6) | 0.235 | 0.628 |
| ACE-I or ARB, n (%) | 44(81.5) | 38(77.6) | 0.245 | 0.621 |
"
| Patient group | Pro-BNP, ng/L | Fvalue | Hs-CRP, mg/L | Fvalue | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| admission | 1 week | 2 weeks | 6 months | admission | 1 week | 2 weeks | 6 months | |||
| IT group (n=49) | 438±291 | 298±222* | 311±241 | 305±209 | 14.875 | 9.6±3.2 | 6.1±2.7* | 3.6±1.8# | 3.0±1.5 | 81.369 |
| ST group (n=54) | 445±236 | 397±253 | 344±261 | 328±245 | 3.369 | 9.8±3.6 | 7.7±3.2* | 4.5±2.0# | 3.4±1.7? | 73.066 |
| F value | 0.382 | 4.603 | 1.981 | 0.413 | 0.140 | 7.718 | 5.532 | 1.172 | ||
| P value | 0.510 | 0.032 | 0.144 | 0.368 | 0.709 | 0.009 | 0.021 | 0.282 | ||
| Patient group | ET-1, ng/L | F value | MDA, nmol/l | F value | ||||||
| admission | 1 week | 2 weeks | 6 months | admission | 1 week | 2 weeks | 6 months | |||
| IT group (n=49) | 68.8±12.4 | 50.6±10.9* | 41.1±10.6# | 35.7±8.4? | 105.460 | 12.0±2.6 | 5.1±2.3* | 3.8±1.3# | 3.6±1.3 | 140.583 |
| ST group (n=54) | 66.1±11.5 | 57.7±253* | 44.5±10.7# | 37.9±9.9? | 97.477 | 11.2±2.4 | 5.3±1.8* | 4.2±1.5# | 4.0±1.5 | 138.848 |
| F value | 1.215 | 7.882 | 2.587 | 1.397 | 2.557 | 0.621 | 0.204 | 0.164 | ||
| P value | 0.273 | 0.006 | 0.111 | 0.240 | 0.113 | 0.429 | 0.604 | 0.782 | ||
| Patient group | MMP-2, μg/L | Fvalue | MMP-9, μg/L | Fvalue | ||||||
| admission | 1 week | 2 weeks | 6 months | admission | 1 week | 2 weeks | 6 months | |||
| IT group (n=49) | 270±110 | 236±103* | 241±111 | 218±88? | 2.635 | 93±47 | 57±28* | 46±25# | 39±20? | 47.039 |
| ST group (n=54) | 259±106 | 240±103* | 232±99 | 210±93? | 1.047 | 97±47 | 77±42* | 51±28# | 41±24? | 15.443 |
| F value | 0.218 | 0.104 | 0.168 | 0.142 | 0.711 | 4.834 | 0.434 | 0.551 | ||
| P value | 0.688 | 0.881 | 0.721 | 0.771 | 0.723 | 0.028 | 0.501 | 0.614 | ||
"
| Echocardiographic parameter | Time points | ST group (n=54) | IT group (n=49) | t value | P value |
|---|---|---|---|---|---|
| LVEDV, ml | Admission | 108±17 | 103±16 | 1.184 | 0.241 |
| 2 weeks | 109±17 | 104±17 | 1.079 | 0.294 | |
| 1 year | 119±17* | 115±19# | 0.722 | 0.444 | |
| Δ | 10.8±5.6 | 12.3±6.7 | 1.041 | 0.311 | |
| LVESV, ml | Admission | 55±10 | 51±11 | 1.081 | 0.207 |
| 2 weeks | 54±11 | 52±11 | 1.157 | 0.287 | |
| 1 year | 54±9 | 51±13 | 1.228 | 0.221 | |
| Δ | -0.3±4.6 | -0.4±3.5 | 0.092 | 0.927 | |
| LVEF, n(%) | Admission | 49±7 | 50±8 | 0.734 | 0.551 |
| 2 weeks | 50±7 | 51±8 | 0.423 | 0.693 | |
| 1 year | 54±7? | 56±8? | 1.354 | 0.187 | |
| Δ | 4.7±3.3 | 6.0±4.6 | 1.488 | 0.154 |
| 1. |
Gajarsa JJ, Kloner RA . Left ventricular remodeling in the post-infarction heart: A review of cellular, molecular mechanisms, and therapeutic modalities. Heart Fail Rev 2011; 16(1):13-21. doi: 10.1007/s10741-010-9181-7.
doi: 10.1007/s10741-010-9181-7 |
| 2. |
Westman PC, Lipinski MJ, Luger D , et al. Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol 2016; 67(17):2050-60. doi: 10.1016/j.jacc.2016.01.073.
doi: 10.1016/j.jacc.2016.01.073 pmid: 27126533 |
| 3. |
Nilsson L, Hallén J, Atar D , et al. Early measurements of plasma matrix metalloproteinase-2 predict infarct size and ventricular dysfunction in ST-elevation myocardial infarction. Heart 2012; 98(1):31-6. doi: 10.1136/heartjnl-2011-300079.
doi: 10.1136/heartjnl-2011-300079 pmid: 21727201 |
| 4. |
van Klei WA, Buhre WF . Anti-inflammatory effects of perioperative statin therapy. Can J Anaesth 2012; 59(6):516-21. doi: 10.1007/s12630-012-9703-y.
doi: 10.1007/s12630-012-9703-y pmid: 2 |
| 5. |
Oesterle A, Laufs U, Liao JK . Pleiotropic effects of statins on the cardiovascular system. Circ Res 2017; 120(1):229-43. doi: 10.1161/CIRCRESAHA.116.308537.
doi: 10.1161/CIRCRESAHA.116.308537 pmid: 5467317 |
| 6. |
Mao Y, Koga JI, Tokutome M , et al. Nanoparticle-mediated delivery of pitavastatin to monocytes/macrophages inhibits left ventricular remodeling after acute myocardial infarction by inhibiting monocyte-mediated inflammation. Int Heart J 2017; 58(4):615-23. doi: 10.1536/ihj.16-457.
doi: 10.1536/ihj.16-457 pmid: 28701679 |
| 7. |
Shirakabe A, Asai K, Hata N , et al. Immediate administration of atorvastatin decreased the serum MMP-2 level and improved the prognosis for acute heart failure. J Cardiol 2012; 59(3):374-82. doi: 10.1016/j.jjcc.2012.01.009.
doi: 10.1016/j.jjcc.2012.01.009 pmid: 22402418 |
| 8. |
Ansheles AA, Rvacheva AV, Sergienko IV . Effect of atorvastatin therapy on the level of CD34+CD133+CD309+ endothelial progenitor cells in patients with coronary heart disease. Bull Exp Biol Med 2017; 163(1):133-6. doi: 10.1007/s10517-017-3753-7.
doi: 10.1007/s10517-017-3753-7 pmid: 28577105 |
| 9. |
Sahebkar A, Kotani K, Serban C , et al. Statin therapy reduces plasma endothelin-1 concentrations: A meta-analysis of 15 randomized controlled trials. Atherosclerosis 2015; 241(2):433-42. doi: 10.1016/j.atherosclerosis.2015.05.022.
doi: 10.1016/j.atherosclerosis.2015.05.022 pmid: 26074317 |
| 10. |
Ishida K, Geshi T, Nakano A , et al. Beneficial effects of statin treatment on coronary microvascular dysfunction and left ventricular remodeling in patients with acute myocardial infarction. Int J Cardiol 2012; 155(3):442-7. doi: 10.1016/j.ijcard.2011.11.015.
doi: 10.1016/j.ijcard.2011.11.015 pmid: 22146235 |
| 11. |
Rebic D, Rasic S, Rebic V . Influence of endothelin-1 and nitric oxide on left ventricular remodeling in patients on peritoneal dialysis. Ren Fail 2014; 36(2):232-6. doi: 10.3109/0886022X.2013.836935.
doi: 10.3109/0886022X.2013.836935 pmid: 24059246 |
| 12. |
Lee BK, Koo BK, Nam CW , et al. Does Pre-treatment with high dose atorvastatin prevent microvascular dysfunction after percutaneous coronary intervention in patients with acute coronary syndrome? Korean Circ J 2016; 46(4):472-80. doi: 10.4070/kcj.2016.46.4.472.
doi: 10.4070/kcj.2016.46.4.472 pmid: 27482255 |
| 13. |
Masci PG, Ganame J, Francone M , et al. Relationship between location and size of myocardial infarction and their reciprocal influences on post-infarction left ventricular remodelling. Eur Heart J 2011; 32(13):1640-8. doi: 10.1093/eurheartj/ehr064.
doi: 10.1093/eurheartj/ehr064 pmid: 21398642 |
| 14. |
Schiller NB, Shah PM, Crawford M , et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2(5):358-67. doi: 10.1016/s0894-7317(89)80014-8.
doi: 10.1016/s0894-7317(89)80014-8 |
| 15. |
Casas JP, Shah T, Hingorani AD , et al. C-reactive protein and coronary heart disease: a critical review. J Intern Med 2008; 264(4):295-314. doi: 10.1111/j.1365-2796.2008.02015.x.
doi: 10.1111/j.1365-2796.2008.02015.x pmid: 18823504 |
| 16. |
Takahashi T, Anzai T, Kaneko H , et al. Increased C-reactive protein expression exacerbates left ventricular dysfunction and remodeling after myocardial infarction. Am J Physiol Heart Circ Physiol 2010; 299(6):H1795-1804. doi: 10.1152/ajpheart.00001.2010.
doi: 10.1152/ajpheart.00001.2010 pmid: 20852043 |
| 17. |
Tousoulis D, Oikonomou E, Siasos G , et al. Dose-dependent effects of short term atorvastatin treatment on arterial wall properties and on indices of left ventricular remodeling in ischemic heart failure. Atherosclerosis 2013; 227(2):367-72. doi: 10.1016/j.atherosclerosis.2013.01.015.
doi: 10.1016/j.atherosclerosis.2013.01.015 pmid: 23433403 |
| 18. |
DeLeon-Pennell KY, Meschiari CA, Jung M , et al. Matrix Metalloproteinases in Myocardial Infarction and Heart Failure. Prog Mol Biol Transl Sci 2017; 147:75-100. doi: 10.1016/bs.pmbts.2017.02.001.
doi: 10.1016/bs.pmbts.2017.02.001 |
| 19. |
Wang J, Tan GJ, Han LN , et al. Novel biomarkers for cardiovascular risk prediction. J Geriatr Cardiol 2017; 14(2):135-50. doi: 10.11909/j.issn.1671-5411.2017.02.008.
doi: 10.11909/j.issn.1671-5411.2017.02.008 pmid: 5409355 |
| [1] | Shun-hua Zhang*, Jia-liang Zhao. Impact of Combination Use of 0.004% Travoprost and 2% Pilocarpine on Matrix Metalloproteinases Synthesized by Rabbit Ciliary Muscle: a Pilot Study [J]. Chinese Medical Sciences Journal, 2013, 28(4): 229-232. |
| [2] | Wei-wei Yu, and Qin Xia. Contrary Regulation of TIMP-1 and MMP-9 by Hepatocyte Growth Factor Antibody after Lung Injury [J]. Chinese Medical Sciences Journal, 2011, 26(4): 216-220. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|