Chinese Medical Sciences Journal ›› 2017, Vol. 32 ›› Issue (3): 161-170.doi: 10.24920/J1001-9294.2017.023
• Original Article • Previous Articles Next Articles
Transradial Versus Transfemoral Approach for Percutaneous Coronary Intervention in Elderly Patients in China: A Retrospective Analysis
Jin Chen?, Xu Yi?, Qiao Shu-bin, Tang Xin-ran, Wu Yong-jian, Yan Hong-bing, Dou Ke-fei, Xu Bo, Yang Jin-gang, Yang Yue-jin*( )
)
- State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center of Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100037, China
-
Received:2016-12-07Published:2017-09-27Online:2017-09-27 -
Contact:Jin Chen,Xu Yi,Yang Yue-jin E-mail:yangyjfw@126.com
Cite this article
Jin Chen, Xu Yi, Qiao Shu-bin, Tang Xin-ran, Wu Yong-jian, Yan Hong-bing, Dou Ke-fei, Xu Bo, Yang Jin-gang, Yang Yue-jin. Transradial Versus Transfemoral Approach for Percutaneous Coronary Intervention in Elderly Patients in China: A Retrospective Analysis[J].Chinese Medical Sciences Journal, 2017, 32(3): 161-170.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Baseline characteristics of elderly patients undergoing TRI and TFI"
| Characteristics | TRI group | TFI group | Standardized difference |
|---|---|---|---|
| n | 1033 | 96 | 18.5 |
| Age§ (yrs) | 71.0±8.4 | 71.7±3.9 | |
| Female [n (%)] | 361 (34.9) | 98 (50.0) | 30.8 |
| Medical history | |||
| Myocardial infarction [n (%)] | 174 (16.8) | 44 (22.4) | 14.1 |
| Prior CABG [n (%)] | 12 (1.2) | 19 (9.7) | 38.3 |
| Prior PCI [n (%)] | 179 (17.3) | 56 (28.6) | 27.0 |
| Stroke [n (%)] | 107 (10.4) | 27 (13.8) | 10.5 |
| Diabetes mellitus [n (%)] | 278 (26.9) | 72 (36.7) | 21.2 |
| Hypertension [n (%)] | 711 (68.8) | 141 (71.9) | 6.8 |
| Hyperlipidemia [n (%)] | 623 (60.3) | 110 (59.2) | 2.3 |
| Diagnosis | |||
| STEMI [n (%)] | 131 (12.7) | 15 (7.7) | 16.7 |
| NSTEMI [n (%)] | 45 (4.4) | 8 (4.1) | 1.4 |
| Unstable angina [n (%)] | 554 (53.6) | 110 (56.1) | 5.0 |
| Stable angina [n (%)] | 274 (26.5) | 56 (28.6) | 4.6 |
| Vital signs | |||
| Heart rate§ (bpm) | 69.1±10.6 | 69.1±8.7 | 0.1 |
| Systolic blood pressure§ (mm Hg) | 132.2±17.8 | 132.7±18.8 | 2.6 |
| Diastolic blood pressure§ (mm Hg) | 77.3±24.0 | 76.2±9.9 | 6.0 |
| LVEF§ (%) | 62.2±7.6 | 60.8±7.9 | 17.9 |
| Creatinine§ (μmol/L) | 84.4±20.7 | 84.1±21.4 | 1.2 |
Table 2
Procedural characteristics of elderly patients undergoing TRI and TFI"
| Characteristics | TRI group | TFI group | Standardized difference |
|---|---|---|---|
| n | 1033 | 196 | |
| Artery sheath size§(F) | 6.0±0.2 | 6.1±0.3 | 33.5 |
| Diseased coronary vessels | 978 | 171 | |
| Single vessel [n (%)] | 236 (24.1) | 31 (18.1) | 14.7 |
| Double vessel [n (%)] | 344 (35.2) | 63 (36.8) | 3.5 |
| Triple vessel [n (%)] | 398 (40.7) | 77 (45.0) | 8.8 |
| Left main disease [n (%)] | 69 (7.1) | 15 (8.8) | 6.4 |
| Lesion type | |||
| De novo [n (%)] | 1334 (98.4) | 252 (95.8) | 15.3 |
| Intra stent [n (%)] | 17 (1.3) | 5 (1.9) | 5.2 |
| Restenosis [n (%)] | 5 (0.4) | 6 (2.3) | 16.8 |
| Lesion location | |||
| Ostial lesion [n (%)] | 160 (11.6) | 47 (17.6) | 16.9 |
| Bifurcation lesion [n (%)] | 430 (31.4) | 95 (35.4) | 8.6 |
| Number of treated lesion Median (IQR) | 1 (1-2) | 1 (1-2) | 9.9 |
| Number of stents used Median (IQR) | 2 (1-2) | 2 (1-2) | 4.8 |
| Stent type | 9.1 | ||
| Drug-eluting only [n (%)] | 1030 (99.7) | 194 (99.0) | |
| Drug-eluting and bare metal [n (%)] | 3 (0.3) | 2 (1.0) | |
| Domestic vs. imported stents | 7.0 | ||
| Domestic only [n (%)] | 544 (52.7) | 110 (56.1) | |
| Imported only [n (%)] | 462 (44.7) | 81 (41.3) | |
| Domestic and imported [n (%)] | 27 (2.6) | 5 (2.6) | |
| Intravascular ultrasound [n (%)] | 30 (2.9) | 14 (5.3) | 16.4 |
| Vascular closure devices [n (%)] | 0 (0) | 141 (71.9) | 226.4 |
Figure 1.
Comparisons of baseline and procedural characteristics between transradial and transfemoral intervention groups before and after IPW adjustment. A standardized difference >10 indicates significant imbalance between the two groups. MI: myocardial infarction; DES: drug-eluting stent; BMS: bare metal stent; IPW: inverse probability weighting."
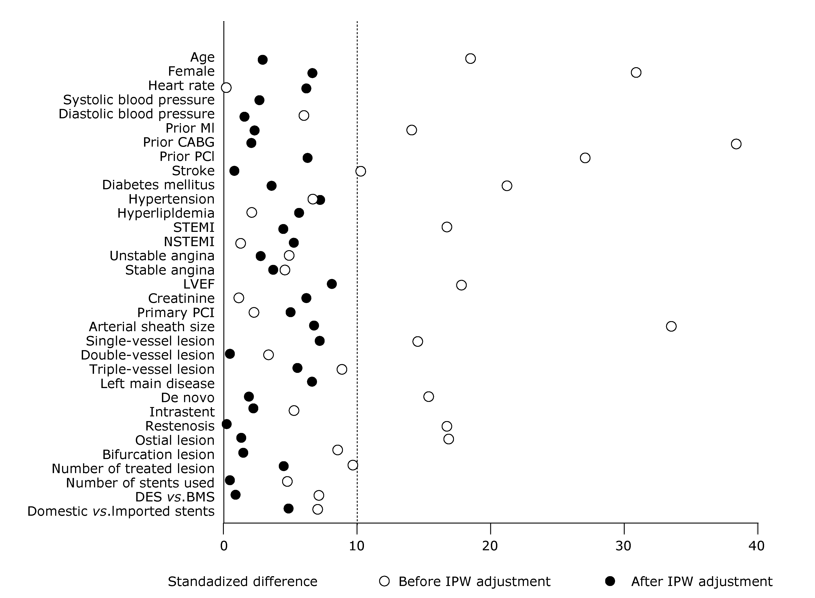
Table 3
Comparisons of hospital costs and clinical outcomes between the groups of TRI and TFI"
| Items | TRI group | TFI group | Unadjusted OR (95%CI) | Adjusted OR (95%CI) | P value |
|---|---|---|---|---|---|
| n | 1033 | 196 | |||
| Hospital costs [mean (95%CI), CNY] | |||||
| Total cost | 59 044 (54 995-63 392) | 68 997 (63 172-75 359) | -9953 (-12 610 to -7171)* | -7495 (-10 420 to -4419)* | <0.0001 |
| PCI-related costs | 44 411 (41 604-47 407) | 50 363 (46 865-54 122) | -5952 (-7770 to -4057)* | -4067 (-6321 to -1693)* | 0.0010 |
| Hospitalization costs | 4950 (4241-5777) | 6711 (5585-8062) | -1761 (-2344 to -1100)* | -1394 (-2030 to -667)* | 0.0004 |
| Medication costs | 4653 (4273-5067) | 6080 (5015-7372) | -1427 (-2015 to -754)* | -1360 (-2003 to 614)* | 0.0007 |
| Examination costs | 5028 (4496-5622) | 5833 (5144-6615) | -806 (-1243, -327)* | -671 (-1146 to -147)* | 0.0133 |
| Clinical outcomes [n (%)] | |||||
| MACE | 30 (2.9) | 11 (5.6) | 0.50 (0.35-0.73) | 0.47 (0.31-0.73) | <0.001 |
| BARC ≥2 bleeding | 80 (7.7) | 17 (8.7) | 0.88 (0.59-1.33) | 0.98 (0.64-1.52) | 0.940 |
| BARC ≥3 bleeding | 12 (1.2) | 6 (3.1) | 0.37 (0.13-1.06) | 0.34 (0.12-1.01) | 0.051 |
| Length of stay [mean (95%CI), d] | 6.7 (6.2-7.3) | 8.9 (7.6, 10.4) | -2.2 (-2.8 to -1.4)* | -1.9 (-2.7 to -1.1)* | <0.0001 |
| Post-procedural stay [mean (95%CI), d] | 3.6 (3.2-4.1) | 4.2 (3.4, 5.1) | -0.6 (-1.0 to -0.1)* | -0.7 (-1.1 to -0.3)* | 0.0017 |
Table 4
Comparisons of hospital costs and clinical outcomes between the groups of TRI and TFI: subgroup analyses by acute myocardial infarction, acute coronary syndrome, and stable angina"
| Items | TRI group | TFI group | Unadjusted OR (95%CI) | Adjusted OR (95%CI) | P value |
|---|---|---|---|---|---|
| Acute myocardial infarction | |||||
| n | 176 | 23 | |||
| Total hospital costs [mean (95%CI), CNY] | 64 002 (57 669-71 031) | 79 265 (66 717-94 173) | -15 263 (-27 826, 368)* | -9812 (-21 200, 4020)* | 0.153 |
| MACE [n (%)] | 6 (3.4) | 1 (4.3) | 0.78 (0.32, 1.86) | 0.66 (0.26, 1.71) | 0.396 |
| BARC ≥2 bleeding [n (%)] | 19 (10.8) | 3 (13.0) | 0.81 (0.31, 2.10) | 1.51 (0.51, 4.51) | 0.460 |
| BARC ≥3 bleeding [n (%)] | 4 (2.3) | 1 (4.3) | 0.51 (0.12, 2.23) | 0.42 (0.09, 2.06) | 0.284 |
| Length of stay [mean (95%CI), d] | 9.2 (8.2-10.3) | 11.2 (9.2-13.6) | -2.0 (-4.0, 0.5)* | -1.0 (-3.6, 2.5)* | 0.525 |
| Postprocedural stay [mean (95%CI), d] | 4.9 (4.1-6.0) | 6.2 (4.8-8.0) | -1.3 (-2.7, 0.7)* | -0.7 (-2.2, 1.4)* | 0.462 |
| Acute coronary syndrome | |||||
| n | 730 | 133 | |||
| Total hospital costs [mean (95%CI), CNY] | 58 225 (54 095-62 671) | 71 725 (66 068-77 866) | -13 500 (-17 101, -9661)* | -12,508 (-17,524, -7023)* | <0.001 |
| MACE [n (%)] | 20 (2.7) | 8 (6.0) | 0.44 (0.26, 0.74) | 0.41 (0.25, 0.68) | <0.001 |
| BARC ≥2 bleeding [n (%)] | 60 (8.2) | 12 (9.0) | 0.90 (0.57, 1.44) | 1.12 (0.68, 1.85) | 0.657 |
| BARC ≥3 bleeding [n (%)] | 10 (1.4) | 5 (3.8) | 0.36 (0.15, 0.82) | 0.30 (0.13, 0.74) | 0.008 |
| Length of stay [mean (95%CI), d] | 6.9 (6.4-7.5) | 9.4 (8.1-10.9) | -2.3 (-3.2, -1.7)* | -2.6 (-3.5, -1.5)* | <0.001 |
| Post procedural stay [mean (95%CI), d] | 3.7 (3.2-4.1) | 4.4 (3.7-5.3) | -0.8 (-1.2, -0.2)* | -1.0 (-1.5, -0.4)* | 0.001 |
| Stable angina | |||||
| n | 274 | 56 | |||
| Total hospital costs [ mean (95%CI), CNY] | 61 039 (56 774-65 624) | 63 460 (55 034-73 177) | -2422 (-8381, 4183)* | 3710 (-2818, 11 009)* | 0.277 |
| MACE [n (%)] | 10 (3.6) | 3 (5.4) | 0.67 (0.27, 1.69) | 0.68 (0.24, 1.90) | 0.462 |
| BARC ≥2 bleeding [n (%)] | 18 (6.6) | 5 (8.9) | 0.72 (0.28, 1.86) | 0.66 (0.18, 2.41) | 0.533 |
| BARC ≥3 bleeding [n (%)] | 2 (0.7) | 1 (1.8) | 0.40 (0.04, 3.95) | 0.73 (0.07, 7.56) | 0.791 |
| Length of stay [mean (95%CI), d] | 6.1 (5.5-6.7) | 8.1 (6.8-9.6) | -2.0 (-2.7, -1.2)* | -0.7 (-1.5, -0.2)* | 0.133 |
| Post-procedural stay [mean (95%CI), d] | 3.5 (2.9-4.1) | 3.8 (3.0-4.7) | -0.3 (-0.7, 0.1)* | -0.2 (-0.5, 0.2)* | 0.430 |
| 1. | Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, et al.Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 2011; 377(9775):1409-20. doi: 10.1016/S0140-6736(11)60404-2. |
| 2. | Yang Y-J, Kandzari DE, Gao Z, Xu B, Chen J-L, Qiao S-B, et al.Transradial versus transfemoral method of percutaneous coronary revascularization for unprotected left main coronary artery disease: comparison of procedural and late-term outcomes. JACC Cardiovasc Interv 2010; 3(10):1035-42. doi: 10.1016/j.jcin.2010.09.003. |
| 3. | Brueck M, Bandorski D, Kramer W, Wieczorek M, Höltgen R, Tillmanns H.A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv 2009; 2(11): 1047-54. doi: 10.1016/j.jcin.2009.07.016. |
| 4. | Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, et al.Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention an updated report from the National Cardiovascular Data Registry (2007-2012). Circulation 2013; 127(23):2295-306. doi: 10.1161/CIRCULATIONAHA. 112.000536. |
| 5. | Chase AJ, Fretz EB, Warburton WP, Klinke WP, Carere RG, Pi D, et al.Association of the arterial access site at angioplasty with transfusion and mortality: the MORTAL study (Mortality benefit of reduced transfusion after percutaneous coronary intervention via the arm or leg). Heart 2008; 94(8):1019-25. doi: 10.1136/hrt.2007.136390. |
| 6. | Baklanov DV, Kaltenbach LA, Marso SP, Subherwal SS, Feldman DN, Garratt KN, et al.The prevalence and outcomes of transradial percutaneous coronary intervention for ST-segment elevation myocardial infarction: analysis from the National Cardiovascular Data Registry (2007 to 2011). J Am Coll Cardiol 2013; 61(4):420-6. doi: 10.1016/j.jacc.2012.10.032. |
| 7. | Rao SV, Cohen MG, Kandzari DE, Bertrand OF, Gilchrist IC.The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol 2010; 55(20):2187-95. doi: 10.1016/j.jacc.2010.01.039. |
| 8. | Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, et al.Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol 2012; 60(24):2481-9. doi: 10.1016/j.jacc.2012.06.017. |
| 9. | Jin C, Li W, Qiao SB, Yang JG, Wang Y, He PY, et al.Costs and benefits associated with transradial versus transfemoral percutaneous coronary intervention in China. J Am Heart Assoc 2016; 5(4):e002684. doi: 10.1161/JAHA.115. 002684. |
| 10. | Arnold SV, Alexander KP, Masoudi FA, Ho PM, Xiao L, Spertus JA.The effect of age on functional and mortality outcomes after acute myocardial infarction. J Am Geriatr Soc 2009; 57(2):209-17. doi: 10.1111/j.1532-5415.2008.02106.x. |
| 11. | Feldman DN, Gade CL, Slotwiner AJ, Parikh M, Bergman G, Wong SC, et al.Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (< 60, 60 to 80, and> 80 years) (from the New York State Angioplasty Registry). Am J Cardiol 2006; 98(10):1334-9. doi: 10.1016/j.amjcard.2006.06.026. |
| 12. | Piper WD, Malenka DJ, Ryan TJ, Shubrooks SJ, T O’Connor G, Robb JF, et al. Predicting vascular complications in percutaneous coronary interventions. Am Heart J 2003; 145(6):1022-9. doi: 10.1016/S0002-8703(03)00079-6. |
| 13. | Assali AR, Moustapha A, Sdringola S, Salloum J, Awadalla H, Saikia S, et al.The dilemma of success: percutaneous coronary interventions in patients ≥ 75 years of age—successful but associated with higher vascular complications and cardiac mortality. Catheter Cardiovasc Interv 2003; 59(2):195-9. doi: 10.1002/ccd.10532. |
| 14. | Koutouzis M, Matejka G, Olivecrona G, Grip L, Albertsson P. Radial vs. femoral approach for primary percutaneous coronary intervention in octogenarians. Cardiovasc Revasc Med 2010; 11(2):79-83. doi: 10.1016/j.carrev.2009. 04.107. |
| 15. | Achenbach S, Ropers D, Kallert L, Turan N, Krähner R, Wolf T, et al.Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv 2008; 72(5): 629-35. doi: 10.1002/ccd.21696. |
| 16. | Jaffe R, Hong T, Sharieff W, Chisholm RJ, Kutryk MJB, Charron T, et al.Comparison of radial versus femoral approach for percutaneous coronary interventions in octogenarians. Catheter Cardiovasc Interv 2007; 69(6):815-20. doi: 10.1002/ccd.21021. |
| 17. | Yan ZX, Zhou YJ, Zhao YX, Liu YY, Shi DM, Guo YH, et al.Safety and feasibility of transradial approach for primary percutaneous coronary intervention in elderly patients with acute myocardial infarction. Chin Med J (Engl) 2008; 121(9):782-6. |
| 18. | He PY, Yang YJ, Qiao SB, Xu B, Yao M, Wu YJ, et al.A comparison of transradial and transfemoral approaches for percutaneous coronary intervention in elderly patients based on a propensity score analysis. Angiology 2014; 66(5):448-55. doi: 10.1177/0003319714535971. |
| 19. | Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al.Standardized bleeding definitions for cardiovascular clinical trials a consensus report from the bleeding academic research consortium. Circulation 2011; 123(23):2736-47. doi: 10.1161/CIRCULATIONAHA.110. 009449. |
| 20. | Flury BK, Riedwyl H.Standard distance in univariate and multivariate analysis. Am Stat 1986; 40(3):249-51. |
| 21. | Austin PC.Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009; 28(25):3083-107. doi: 10.1002/sim.3697. |
| 22. | Curtis LH, Hammill BG, Eisenstein EL, Kramer JM, Anstrom KJ.Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care 2007; 45(10):S103-7. doi: 10.1097/ MLR.0b013e31806518ac. |
| 23. | Austin PC.Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 2011; 10(2):150-61. doi: 10.1002/pst.433. |
| 24. | Windecker S, Kolh P, Alfonso F, Collet J-P, Cremer J, Falk V, et al.2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35(37):2541-619. doi: 10.1093/ eurheartj/ehu278. |
| 25. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al.2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2016; 133(11):1135-47. doi: 10.1161/CIR.0000000000000336. |
| 26. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al.2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58(24):e44-122. doi: 10.1016/j. jacc.2011.08.007. |
| 27. | Mehta RH, Rathore SS, Radford MJ, Wang Y, Wang Y, Krumholz HM.Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol 2001; 38(3):736-41. |
| 28. | Klein LW, Block P, Brindis RG, McKay CR, McCallister BD, Wolk M, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology-National Cardiovascular Data Registry: development of a nomogram predictive of in-hospital mortality. J Am Coll Cardiol 2002; 40(3):394-402. |
| 29. | Doyle BJ, Rihal CS, Gastineau DA, Holmes DR.Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J Am Coll Cardiol 2009; 53(22):2019-27. doi: 10.1016/j.jacc.2008.12.073. |
| 30. | Dauerman HL, Rao SV, Resnic FS,Applegate RJ.Bleeding avoidance strategies: consensus and controversy. J Am Coll Cardiol 2011; 58(1):1-10. doi: 10.1016/j.jacc.2011. 02.039. |
| 31. | Jin C, Xu Y, Qiao SB, Tang XR, Wu YJ, Yan HB, et al. Comparison of transradial and transfemoral approaches in women undergoing percutaneous coronary intervention in China: a retrospective observational study. Angiology 2017 Jan 1:3319716685670. doi: 10.1177/0003319716685670. |
| [1] | Chen Qiang, Zhang Liwei, Huang Dangsheng, Zhang Chunhong, Wang Qiushuang, Shen Dong, Xiong Minjun, Yang Feifei. Five-year Clinical Outcomes of CAD Patients Complicated with Diabetes after StentBoost-optimized Percutaneous Coronary Intervention [J]. Chinese Medical Sciences Journal, 2019, 34(3): 177-183. |
| [2] | Huang Peisen, Yu Yuan, Han Xikun, Yang Yuejin. Efficacy of Short-term Dual Antiplatelet Therapy after Implantation of Second-generation Drug-eluting Stents: A Meta-analysis and Systematic Review [J]. Chinese Medical Sciences Journal, 2017, 32(1): 1-12. |
| [3] | Wei-xian Yang,Zheng Yang,Yong-jian Wu,Shu-bin Qiao,Yue-jin Yang,Ji-lin Chen. Factors Associated with Coronary Artery Disease in Young Population (Age≤40): Analysis with 217 Cases [J]. Chinese Medical Sciences Journal, 2014, 29(1): 38-42. |
| [4] | Fei Ye, Qin Liang, Song-hui Luo, Li-feng Hong. Coronary Artery Perforation Complicated With Acute Aortic Valve Regurgitation During Percutaneous Coronary Intervention: Report of Two Cases [J]. Chinese Medical Sciences Journal, 2013, 28(4): 250-253. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|

