IDIOPATHIC membranous nephropathy (IMN) is the most common cause of nephrotic syndrome in adult, and its incidence shows a rising trend in recent years.1,2 Thromboembolic event, a well-recognized complication of nephrotic syndrome, occurs much more frequently in IMN than in other kidney diseases.3 Frequency of venous thromboembolic events (VTEs), including deep vein thrombosis (DVT), renal vein thrombosis (RVT), and pulmonary embolism (PE) ranged from 3% to 48% in patients with nephrotic syndrome.3-5 Patients with nephrotic syndrome are also believed to have increased risk of atherosclerosis and coronary heart disease (CHD). Most studies about the association between CHD and nephrotic syndrome were case reports or case series studies.6-8 Risk of arterial thromboembolic events (ATEs), mainly consisting of acute myocardial ischemic events and infarction, thrombotic ischemic stroke(IS), and peripheral artery disease(PAD), had been firstly described in a retrospective cohort study in European patients with nephrotic syndrome,9 but there was in lack of discussion about the risk factors of ATE. Recently, Lee et al reported that patients with IMN were at high risk of cardiovascular events.10 These findings raised our attention on thromboembolic events in Asian patients with IMN. We conducted this research aiming to explore the incidence and the characteristics of ATEs and VTEs in patients with IMN in Chinese population, and to identify the predisposing risk factors of the thromboembolic events at this situation.
MATERIALS AND METHODS
Study cohort
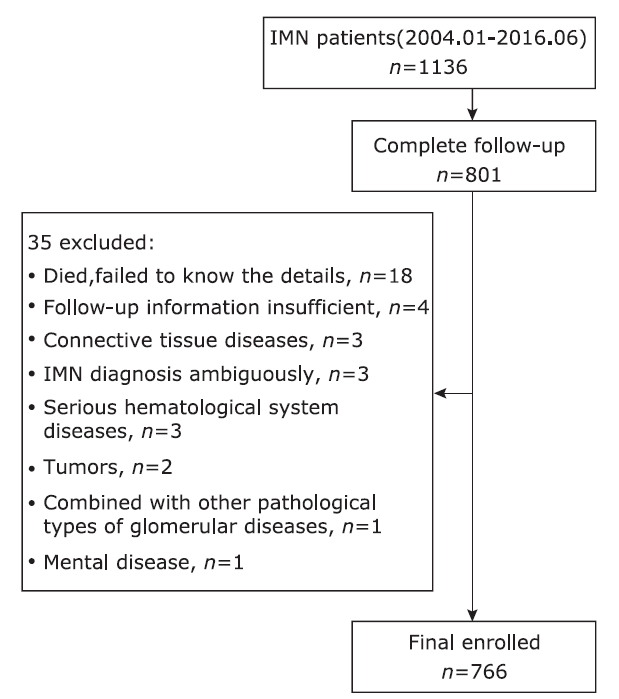
This study was approved by the ethics committee of the Peking Union Medical College Hospital, and the informed consents from participants were waived. A total of 1136 consecutive inpatients who were older than 16 years old and pathologically diagnosed as IMN by biopsy from January 2004 to June 2016 were retrospectively reviewed for this study. The follow-up was conducted till December 31, 2016. The Exclusion criteria were: 1, patients with malignant tumor, autoimmune diseases, serious mental diseases, or hematological diseases; 2, patients with comorbidity of other pathological types of glomerular diseases; 3. IMN diagnose was ambiguous; 4, insufficient follow-up information. There were 801 (70.5%) patients with complete follow-up information. Among them, 35 patients were excluded by a variety of reasons (Fig. 1). Thus 766 patients in total were enrolled in this study.
Information collection and definition of variables
Clinical information at the time of biopsy were collected as the baseline data, including gender, age, history of smoking, history of diabetes, hypertension, and previous onset of ATEs or VTEs, duration of the disease, laboratory test results of proteinuria, serum albumin, serum creatinine, cholesterol, triglycerides, and low density lipoprotein-cholesterol (LDL-C). The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.11 Nephrotic syndrome (NS) status was identified as proteinuria ≥3.5 g/24 h and hypoalbuminemia (≤30 g/L). Sub-nephrotic syndrome was defined as proteinuria >0.3 g/24 h and <3.5 g/24 h. The complete remission (CR) of the NS was identified as proteinuria ≤0.3 g/24 h, with normal serum creatinine.12
Thromboembolic events
We identified all symptomatic thromboembolic events. VTEs consisted of DVT, RVT and PE, and ATEs included CHD, IS and PAD. The diagnoses of DVT, RVT and PAD were confirmed by compression sonography and color-Doppler ultrasound. The diagnosis of PE was made by CT pulmonary angiography. CHD was diagnosed if any of myocardial infarction, angina pectoris or silent myocardial ischemia was confirmed clinically by physicians. IS was diagnosed by medical imaging of CT or MRI. Since cerebral transient ischemic attack was hard to assess, we did not take it into assessment.
Statistical analysis
Statistical analysis was performed by using SPSS (version 22, IBM, Armonk, NY, U.S.). Continuous variables were presented as mean±SD or median with interquartile ranges (IQR), and the differences were evaluated by two tailed independent sample Student t test, Mann-Whitney U test, Kruskal-Wallis test, or univariate ANOVA, depending on the normality of the data and levels of the outcome variable. Categorical variables were presented as percentages, and the differences were compared using chi-square test or Fisher’s test.
The observation time for each patient was defined as the time period from kidney biopsy to death, or to the time of the last follow-up. The incidences of ATE or VTE at 0.5, 1, 2, 3, and 5 years were defined by the percentage of patients who experienced the events in the total number of patient-years. When calculating the cumulative incidence rates of ATE, we ignored the occurrence of VTE, and vice versa. Kaplan-Meier methods were used for cumulative incidence plots. To assess risk factors for ATEs and VTEs, we used Cox proportional hazards regression models. Baseline variables were incorporated into the models. As some patients experienced at least 1 episode of thromboembolic events during the observation time, when analyzing characteristics of ATE or VTE, we treated the thromboembolic events independently. A two-tailed P value of less than 0.05 was considered statistically significant.
RESULTS
Demographic characteristics of the cohort
Of 766 patients enrolled in this study, 58.6% were male and 41.4% were female. The mean age of the cohort was 47.6±14.8 years. Median observation time period was 39.65 (24.5, 62.8) months. Patients in the study cohort presented with a median level of proteinuria 5.49 (3.29, 8.98) g/24 h, a mean serum albumin of 27.2±6.6 g/L, and a mean eGFR of 97.14±21.94 ml/min/1.73 m2. There were 453 out of 766 (59.1%) patients presented with nephrotic syndrome in this cohort.
Clinical manifestations of thromboembolic events
Of 766 enrolled patients, 78 events of ATEs occurred in 71 patients (7 patients experienced 2 episodes of ATEs), 60 events of VTEs occurred in 53 patients (7 patients experienced 2 episodes of VTEs). Besides, 8 patients experienced both episode of ATE and VTE. Of all the ATEs, 45% (35/78) were IS, 50% (39/78) were CAD, and only 5% (4/78) were PAD. DVTs were the majority of VTEs, which accounted for 60%(36/60), while RVT and PE accounted for 13% (8/60) and 27% (16/60) respectively.
Incidences and time distribution of ATE and VTE events
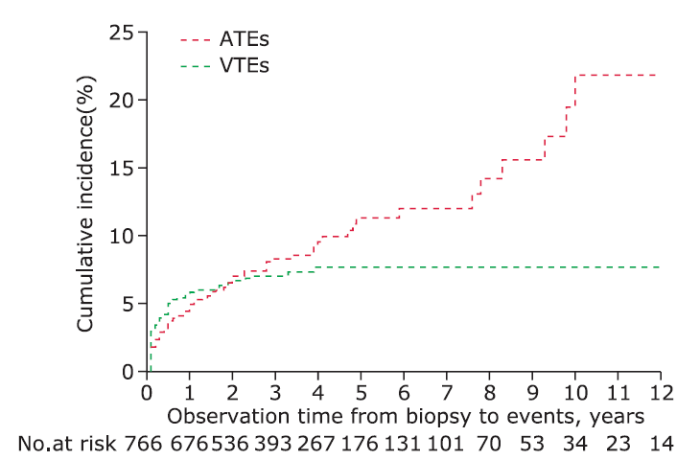
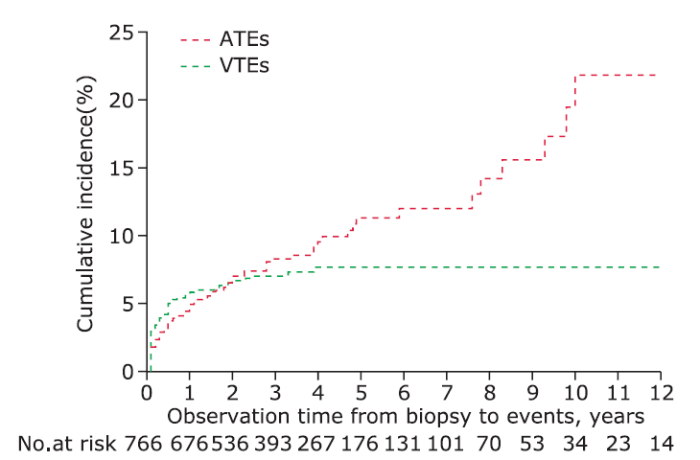
The cumulative incidence rates at 0.5, 1, 2, 3, and 5 years after biopsy were 4.3%, 5.7%, 6.3%, 7.1%, and 8.0% respectively for newly diagnosed ATEs, and 5.9%, 6.8%, 6.9%, 7.0%, and 7.1% respectively for newly diagnosed VTEs (Fig. 2). The distribution of events by years during the observing time (Fig. 3) demonstrated that both ATEs and VTEs showed a onset peak in 0.5 year after biopsy. There was as high as 77.4% (41/53) VTEs occurred in 0.5 years early after diagnosis of IMN, while 36.6% (26/71) ATEs occurred within the first 0.5 years, with the rest of ATEs occurred in almost each year during the observation time. The early onset (in 0.5 year) and delayed onset (over 0.5 year) for thromboembolic events distributed significantly different between ATEs and VTEs patients (χ2=20.3, P<0.001).
Figure 2.
Kaplan-Meier estimates of the probability of VTEs- and ATEs-cumulative incidences. ATEs, arterial thromboembolic events; VTEs, venous thromboembolic events.
Comparison of baseline characteristics between patients with ATEs and VTEs
The baseline characteristics of the IMN patients with onset of ATE and VTE were shown and compared in
Table 1. The mean age of IMN patients who experienced ATE events was significantly older than those of VTEs; patients who experienced ATE showed a significantly lower level of eGFR (88.65±22.27 vs 97.22±18.86 ml/min/1.73 m2, P=0.03). The percentage of patients with nephrotic syndrome in ATEs group and VTEs group were comparable, with no significant difference. The levels of proteinuria and serum albumin were also similar. There was no difference between two groups in smoking exposure and hypertension.
Table 1 Comparison of baseline characteristics between ATE and VTE patients§
| ATEs (n=71) | VTEs (n=53) | Pvalue | |
|---|---|---|---|
| Sex, n (%) | 0.84 | ||
| Male | 44(62.0) | 34(64.2) | |
| Female | 27(38.0) | 19(35.8) | |
| Age, year | 57.0±11.9 | 49.6±14.8 | 0.003 |
| History of | |||
| Smoking, n(%) | 31 (43.7) | 15 (28.3) | 0.08 |
| Hypertension, n (%) | 46 (64.8) | 26 (49.1) | 0.08 |
| Diabetes, n(%) | 16 (22.5) | 14 (26.4) | 0.62 |
| Prior ATE, n(%) | 4 (5.6) | 2 (3.8) | 0.63 |
| Observation time, month | 43.2 (5.4, 145.1) | 43.6 (21.5, 62.0) | 0.41 |
| Proteinuria, g/24 h | 6.38 (3.79, 10.16) | 7.30 (4.88, 10.54) | 0.15 |
| Serum albumin, g/L | 26.7±6.3 | 25.8±6.6 | 0.45 |
| eGFR, ml/min/1.73 m2 | 88.65±22.27 | 97.22±18.86 | 0.03 |
| Total cholesterol, mmol/L | 7.98±2.42 | 8.87±2.84 | 0.11 |
| Triglycerides, mmol/L | 2.43 (1.81, 3.60) | 3.32 (1.96, 4.71) | 0.10 |
| LDL-C, mmol/L | 5.41±2.19 | 5.63±2.48 | 0.68 |
| NS, n (%) | 49 (69.0) | 38 (71.7) | 0.75 |
§:Plus-minus values are means±SD; eGFR:estimated glomerular filtration rate; LDL-C:low density lipoprotein cholesterol; NS:nephrotic syndrome.
Association of thromboembolic events with clinical and laboratory characteristics
There were 58 episodes of ATEs and 56 episodes of VTEs available for analysis, because in a few cases the laboratory examinations at the time of events were left out of the medical records. The detailed clinical and laboratory data at the time of events were statistically analyzed (Table 2). When experienced thromboembolic events, patients of ATEs were significantly older than those of VTEs (mean age 59.0±11.4 vs 50.0±15.4 years, t=3.3, P=0.001), regardless the early or delayed onset. Compared to patients with ATE, patients with VTE had higher level of proteinuria (z=3.1, P=0.002), lower level of serum albumin (t=3.1, P=0.002) and higher level of triglycerides (z=2.0, P=0.04). The mean eGFR level of patients with VTE was relatively higher than those with ATE (t=-2.5, P=0.02). 81.5% (44/54) of patients with VTE were at NS status. In contrast, 42.1% (24/57) patients with ATE were at NS status. This difference was statistically significant (χ2=18.1,P<0.001).
Table 2 Comparison of the clinical characteristics at the time of events between ATEs and VTEs§
| Characteristics | ATEs (n=58) | VTEs (n=56) | P value† | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean/ Median | Early onset (n=27) | Delayed onset (n=31) | P value* | Mean/ Median | Early onset (n=48) | Delayed onset (n=8) | P value* | |||
| Age, year | 59.0±11.4 | 59.4±11.8 | 58.7±11.2 | 0.81 | 50.0±15.4 | 49.0±16.0 | 56.4±9.5 | 0.21 | 0.001 | |
| Proteinuria, g/24 h | 3.5(1.05, 7.12) | 4.5(2.0, 6.7) | 2.8(0.7, 7.8) | 0.33 | 6.2(4.5, 9.6) | 6.2(4.5, 9.8) | 6.7(4.4, 9.2) | 0.76 | 0.002 | |
| Serum albumin, g/L | 29.8±8.0 | 26.8±7.6 | 32.4±7.5 | 0.01 | 25.1±7.7 | 25.1±8.1 | 25.1±5.8 | 1.00 | 0.002 | |
| eGFR, ml/min/ 1.73m2 | 84.2±22.1 | 87.5±20.8 | 81.6±23.1 | 0.35 | 94.8±22.3 | 96.6±21.4 | 84.0±26.3 | 0.14 | 0.02 | |
| Total cholesterol, mmol/L | 7.4(5.1, 8.9) | 7.8(6.5, 8.9) | 6.1(4.9, 9.3) | 0.11 | 8.0(6.3, 9.3) | 8.4±2.7 | 7.9±1.4 | 0.66 | 0.21 | |
| Triglycerides, mmol/L | 2.1(1.7, 3.0) | 2.1(1.7, 4.3) | 2.6(1.1, 2.9) | 0.75 | 3.4(1.9, 4.4) | 3.4(2.0, 4.0) | 1.9(1.6, 4.8) | 0.63 | 0.04 | |
| LDL-C, mmol/L | 4.3(2.7, 6.5) | 5.5(2.7, 6.7) | 3.8(2.6, 6.4) | 0.27 | 4.5(3.4, 7.0) | 4.5(3.3, 7.2) | 4.51(3.45, -) | 0.87 | 0.54 | |
| NS, n (%) | < 0.001 | |||||||||
| NS status | 24 (42.1) | 16 (59.3) | 8 (26.7) | 0.01 | 44 (81.5) | 38 (79.2) | 6 (75.0) | N/A | ||
| Sub-NS | 22 (38.6) | 10 (37.0) | 12 (38.7) | 8 (14.8) | 8 (16.7) | 0 (0.0) | ||||
| CR | 11 (19.3) | 1 (3.7) | 10 (35.5) | 2 (3.7) | 2 (4.2) | 0 (0.0) | ||||
§:Plus-minus values are means±SD; *compared between events with early onset (≤0.5 years) and delayed onset (>0.5 years); †compared between ATEs and VTEs.Note:In ATEs, proteinuria, serum albumin, and eGFR were missed in 6, 8, and 8 patients, respectively; total cholesterol, triglycerides, and LDL-C were available for 35, 33, and 25 patients, respectively. In VTEs, Proteinuria was missed for 3 patients; total cholesterol, triglycerides, and LDL-C were available for 37, 36, and 29 patients, respectively. NS status were unknown in 1 patients with delayed onset ATEs and 2 patients with delayed onset VTEs.
Variables related to the early or delayed onset of thromboembolic events
Forty-eight out of 56 patients with VTE and 27 out of 58 patients with ATE had early onset of the events within 0.5 years after biopsied diagnosis. The clinical characteristics of these early onset events were compared with those of delayed onset events that occurred later than 0.5 years. As shown in Table 2, compared to patients with delayed onset of ATE, patients who experienced early onset of ATE had relatively lower serum albumin level (26.8±7.6 g/L, P=0.01), and higher proportion of NS status (59.3% vs 26.7%, P=0.01). Patients experienced the delayed onset of ATE were mainly at sub-NS status or CR status (38.7% and 35.5%, respectively). In patients with VTEs, both early and delayed onset presented with massive proteinuria and obvious hypoalbuminemia, and the majority of both were at NS status (79.2% and 75.0%, respectively). There were no differences of all variables between early and delayed onset of VTEs.
Risk factors identification for VTE and ATE in IMN patients
Associations of baseline variables with the onset of ATEs and VTEs were shown in Table 3. In the univariable risk prediction models, patients with a history of smoking, hypertension and ATEs were at higher risk of ATEs (HR=1.7, 95% CI:1.0-2.7; HR=1.8, 95% CI: 1.1-3.0; and HR=2.4, 95% CI:1.1-5.2, respextively). A higher incidence of ATEs was coincidence with aging, as the hazard ratio increased to 5.1 in patients of 35-54 years old, and reached to 13.0 (95% CI:3.1-53.3) in patients aged above 55 years old. The higher level of proteinuria was significantly associated with ATEs, with a hazard ratio of 2.2 (95% CI:1.1-4.4) when urine protein reached over 8.0 g/24 h. Severe renal dysfunction (decreased eGFR) at baseline was also associated with increased likelihood of ATEs, although the difference had no significance (P=0.10). VTEs were obviously associated with hypoalbuminemia and massive proteinuria (P=0.01 and P=0.03). The multivariable survival analysis model revealed that the age at the time of diagnosis of IMN independently predicted ATEs (P=0.001), and serum albumin level was the independent predicting factor for VTEs (P=0.03) (Table 4).
Table 3 Univariable model proportional-hazards analysis on association of clinical characteristics with VTE and ATE
| Variables | n | ATE | VTE | |||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | Pvalue | HR | 95% CI | P value | |||
| Sex, male | 449 | 1.2 | 0.8-2.0 | 0.39 | 1.6 | 0.8-2.4 | 0.29 | |
| Age, years | 766 | < 0.001 | 0.35 | |||||
| <35 | 167 | 1.0 | reference | 1.0 | reference | |||
| 35-54 | 323 | 5.1 | 1.2-21.7 | 0.8 | 0.4-1.7 | |||
| ≥55 | 276 | 13.0 | 3.1-53.3 | 1.3 | 0.6-2.6 | |||
| History of | 766 | |||||||
| Smoking | 228 | 1.7 | 1.0-2.7 | 0.03 | 0.9 | 0.5-1.7 | 0.81 | |
| Hypertension | 360 | 1.8 | 1.1-3.0 | 0.02 | 0.9 | 0.5-1.6 | 0.77 | |
| Diabetes | 90 | 1.5 | 0.8-2.8 | 0.24 | 1.3 | 0.6-2.9 | 0.44 | |
| ATE | 35 | 2.4 | 1.1-5.2 | 0.03 | 0.8 | 0.2-3.4 | 0.79 | |
| Proteinuria, g/24 h | 712 | 0.04 | 0.03 | |||||
| <3.5 | 191 | 1.0 | reference | 1.0 | reference | |||
| 3.5-8.0 | 313 | 1.3 | 0.7-2.7 | 3.6 | 1.3-10.5 | |||
| >8.0 | 208 | 2.2 | 1.1-4.4 | 4.3 | 1.5-12.8 | |||
| Serum albumin, g/L | 710 | 0.64 | 0.01 | |||||
| <20 | 73 | 1.6 | 0.6-4.4 | 5.5 | 1.5-19.9 | |||
| 20-35 | 198 | 1.4 | 0.6-3.0 | 2.3 | 0.7-7.6 | |||
| ≥35 | 246 | 1.0 | reference | 1.0 | reference | |||
| eGFR, ml/min/1.73 m2 | 760 | 0.10 | 0.27 | |||||
| ≥90 | 517 | 1.0 | reference | 1.0 | reference | |||
| 60-89 | 195 | 1.4 | 0.8-2.4 | 1.4 | 0.8-2.5 | |||
| <60 | 48 | 2.2 | 1.0-4.8 | 0.3 | 0.1-2.4 | |||
| Total cholesterol, mmol/L | 543 | 0.97 | 0.14 | |||||
| <5.18 | 43 | 1.0 | reference | 1.0 | reference | |||
| 5.18-7.76 | 240 | 0.9 | 0.3-2.4 | 2.4 | 0.3-18.3 | |||
| >7.76 | 260 | 0.9 | 0.3-2.3 | 4.1 | 0.6-30.5 | |||
Table 4 Multivariable model proportional-hazards analysis on risk factors of VTE and ATE
| ATE | VTE | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | Pvalue | Variables | HR | 95% CI | Pvalue | |
| History of | Serum albumin, g/L | 0.03 | ||||||
| Smoker | 1.4 | 0.8-2.4 | 0.19 | <20 | 3.2 | 0.8-12.5 | ||
| ATE | 1.6 | 0.7-3.5 | 0.28 | 20-35 | 1.3 | 0.4-4.5 | ||
| Hypertension | 1.1 | 0.6-1.8 | 0.84 | ≥35 | 1.0 | reference | ||
| Age, years | 0.001 | |||||||
| <35 | 1.0 | reference | ||||||
| 35-54 | 4.4 | 1.0-19.1 | ||||||
| ≥55 | 9.2 | 2.2-39.5 | ||||||
| Proteinuria, g/24 h | 0.11 | Proteinuria, g/24 h | 0.13 | |||||
| <3.5 | 1.0 | reference | <3.5 | 1.0 | reference | |||
| 3.5-8.0 | 1.1 | 0.6-2.3 | 3.5-8.0 | 3.0 | 1.0-8.9 | |||
| >8.0 | 1.9 | 0.9-3.8 | >8.0 | 3.2 | 1.0-10.1 | |||
DISCUSSION
To our knowledge, this study is the largest cohort that investigate the arterial and venous thromboembolic events among Chinese patients with IMN. The findings in this study demonstrate that patients with IMN have high incidences of thromboembolic events compared to the general population, particularly within the first 6 months after pathological diagnosis of the disease. In this Study, we systematic exhibited the cumulative incidence rates of ATEs and VTEs, provided the detail elements of each events, and further investigated the risk factors.
Nephrotic syndrome is characterized by hyperlipidemia, with elevated levels of total cholesterol and LDL-C.13 It is assumed that nephrotic syndrome related hyperlipidemia can accelerate atherosclerosis, thus increase the risk of cardiovascular diseases in patients with NS.14 This hypothesis had been verified by some studies with small specimen,6-9 but the knowledge about cardiovascular diseases risk among patients with IMN are limited.10,15-17 Lee et al demonstrated that patients with IMN were at high risk of cardiovascular events (CVEs).10 In their cohort, the cumulative incidences of CVEs were 4.4%, 5.4%, 8.2%, and 8.8% at 1, 2, 3, and 5 years respectively. Severe renal dysfunction at baseline and severity of nephrotic syndrome were statistically associated with an increased occurrence of CVEs. In our cohort, the cumulative incidences of ATEs were relatively lower compared to those in the Lee’s study.10 This difference might due to there were more patients with severe nephrosis and renal dysfunction in their cohort (proteinuria: 8.7 ± 6.2 g/d, serum albumin: 25 ± 8.0 g/L, eGFR: 68.9 ± 33.5 ml/min/1.73m2) than in ours. Low eGFR was also associated with ATEs, although this association did not reach statistical significance (P=0.10).
In our cohort, IS accounted for 45% of the ATEs, which was obviously distinguished from the results in almost all the studies from western countries, where the majority of the ATEs in their cohorts were CHD. This finding should raise attention on IS as a frequent thromboembolic event in Chinese patients with IMN.
ATEs presented a peak onset early in the 0.5 years after biopsy, with an increasing accumulate incidence over time. It seemed that the occurrence of ATEs had two types: ATE early onset (occurred within 0.5 years) and ATE delayed onset (occurred after 0.5 years). At the time of ATE events, 59.3% of patients experienced early onset of ATE were at nephrotic syndrome status, and presented very low serum albumin levels, while those experienced delayed onset of ATE were mainly at sub-nephrotic syndrome (38.7%) or in remission (35.5%). The severity of nephrotic syndrome at the time of the event was closely related to the risk of early onset ATEs. These findings were in accordance with studies of Lee et al10 and Mahmoodi et al.9 Furthermore, univariable survival analysis showed ATEs were associated with proteinuria, age, smoking, history of hypertension and prior ATE, while multivariable survival analysis model indicated that age independently predict ATEs. All these findings above in this study support the hypothesis that early onset of ATE is probably due to the thrombophilic state of NS, and delayed onset of ATEs may be caused by the accelerated atherosclerosis associated with hyperlipidemia.10
VTE is a common complication in patients with nephrotic syndrome, especially in MN. In our cohort, VTE occurred in 6.9% of IMN patients. The underlying mechanisms are incompletely understood. In nephrotic syndrome, the decreased levels of serum proteins, such as antithrombin Ⅲ, and increased production of fibrinogen in the liver due to urinary loss of pro- and anticoagulant proteins or hypoalbuminemia were considered to be involved in the hypercoagulable state, which results in the increased risk of VTEs.18 Many researchers reported RVT as the most common venous thromboembolism in patients with MN,18-20 however, there is still controversial in whether DVT or RVT occurs more frequently in this situation.5,21 This study revealed that DVTs accounted for 60% of all VTE events in our cohort.
We found that VTEs were mainly occurred within the first 0.5 years after diagnosis, and the accumulative incidence went stable after 2 years. At the time of VTEs events, majority of patients were at NS status (81.5%), with no difference between the early and the delayed onset (79.2% and 75.0%). Previous studies demonstrated that proteinuria, hypoalbuminemia, and the ratio of proteinuria to serum albumin were risk factors for the onset of VTE.4,19,20,22 Recently, Lionaki et al reported that each 10 g/L reduction in serum albumin was associated with a 2.13 fold increased risk of VTE; an albumin level of 28 g/L was the threshold below which the risk for a venous thromboembolic event was the greatest. The authors concluded that hypoalbuminemia at diagnosis of IMN independently predicted a venous thromboembolic event.20 Our study found that the hazard ratio reached to 5.5 for VTE when serum albumin <20 g/L,which further confirmed that hypoalbuminemia was the dominant independent risk factor for VTE. However, proteinuria was not shown to independently predict VTE by multivariable analysis. As most patients can reach remission after efficient therapy in 2 years,23 patients achieved remission in our cohort were about 70%, thus might explain the stable accumulate incidence of VTE after 2 years of diagnosis.
At the time of events, 78.6% of IMN patients who experienced VTEs were at NS status, compared to 41.4% of IMN patients with ATE were at NS status. This finding suggested that severe nephrotic syndrome status may be prone to the onset of VTE. Besides, history of ATE suggested a high risk of a repeated ATE, but had no association with the VTEs.
There are several limitations in our study. As a retrospective study, some baseline laboratory data and follow-up laboratory data were not gainable in all patients. Patients with asymptomatic VTEs did not routinely followed up, and patients with mild symptoms of ATEs were ignored. The absence of these data could lead to the underestimate of the incidences. Although it is the largest cohort that investigate thromboembolic events in Asian patients with IMN by far, the wide confidence intervals of hazard ratios weaken the power of the results. Besides, we failed to further analyze the influence of medications in the cohort, such as glucocorticoids, immunosuppressors, aspirin, and warfarin. Whether prophylactic anticoagulation therapy could lower the risks of events is still unclear and need to be elucidated by further investigations.
In summary, this study reveals that patients with IMN have increased incidences of ATEs and VTEs, especially within the first 6 months of the disease. The majority of ATEs were cardiovascular diseases and thrombotic ischemic stroke, and for VTEs were deep vein thrombosis. IS accounted for 45% of ATEs, which should raise attention for the clinical management of patients with IMN in Chinese population. Proteinuria, aging, history of smoking, hypertension and prior ATE were associated with ATEs. Hypoalbuminemia was the dominant independent risk factor for VTE. Both ATEs and VTEs occured frequently at the status of nephrotic syndrome, but VTEs tend to be more likely to occur than ATEs among patients with nephrotic syndrome. Clinical management to prevent thromboembolic events in the early stage of IMN should gain particular attention in patients who are at the status of nephrotic syndrome.
参考文献
Management of membranous nephropathy: when and what for treatment
Management of Membranous Nephropathy: When and What for Treatment
Changing spectrum of biopsy-proven primary glomerular diseases over the past 15 years: a single-center study in China
Disease-specific risk of venous thromboembolic events is increased in idiopathic glomerulonephritis
The risk of venous thromboembolic events is thought to be highest in patients with membranous nephropathy. This association has been recently questioned, and it is not known whether this simply reflects the severity of proteinuria. To better understand the relationship between histologic diagnosis and the risk of venous thromboembolic events we evaluated patients in the Toronto Glomerulonephritis Registry. Of 1313 patients with idiopathic glomerulonephritis, 395 were diagnosed with membranous nephropathy, 370 with focal segmental glomerulosclerosis (FSGS), and 548 with immunoglobulin-A nephropathy (IgAN). Risk factors were evaluated by Cox proportional hazards for 53 image-confirmed venous thromboembolic events in 44 patients during a median follow-up of 63 months. The risk was highest in patients with membranous nephropathy and FSGS (hazard ratios of 22 and 7.8, respectively) referenced to patients with IgAN. Following adjustment for gender, cancer history, proteinuria, and serum albumin by multivariable analysis, the histologic subtype remained an independent risk for venous thromboembolic events. This risk was still highest in patients with membranous nephropathy followed by FSGS with adjusted hazard ratios of 10.8 and 5.9, respectively. Thus, in this large cohort, histologic diagnosis was an independent risk factor for venous thromboembolic events. Further studies are needed to discover mechanisms responsible for this high risk in patients with membranous nephropathy.
Prophylactic anticoagulation in nephrotic syndrome: a clinical conundrum
Abstract It has long been recognized that nephrotic syndrome is associated with an increased risk for thromboembolic complications, including deep venous thrombosis, renal vein thrombosis, and pulmonary embolism. This risk varies with the nature of the underlying disease and seems to be greatest for membranous nephropathy. Other factors, including the level of serum albumin, previous thromboembolic episodes, and a genetically determined predisposition to thrombosis, may also be involved. Prevention of thromboembolic events with oral anticoagulants in nephrotic syndrome requires a careful case-by-case analysis of the risks for thromboembolic events balanced by the risks for anticoagulant induced bleeding. Markov-based decision analysis using literature-based assumptions regarding these risks has suggested that prophylactic anticoagulants may be indicated in certain circumstances. Such decisions need to take into account the nature of the underlying disease, the severity of the nephrotic syndrome (as assessed by serum albumin concentration), preexisting thrombophilic states, and the overall likelihood of serious bleeding events consequent to oral anticoagulation (as assessed by the international normalized ratio for prothrombin time). The optimal duration of prophylactic anticoagulation is unknown but very likely extends to the duration of the nephrotic state per se.
Venous thromboembolism in patients hospitalized with nephrotic syndrome
Whether pulmonary embolism in patients with the nephrotic syndrome is caused by deep venous thrombosis or renal vein thrombosis is controversial. To determine which is the likely cause of pulmonary embolism in patients with the nephrotic syndrome, we investigated data from the National Hospital Discharge Survey. The number of patients discharged from nonfederal short-stay hospitals in the United States with a diagnostic code of nephrotic syndrome, deep venous thrombosis, renal vein thrombosis, and pulmonary embolism was obtained using ICD-9-M (International Classification of Diseases, Ninth Revision, Clinical Modification) codes. From 1979 to 2005, 925,000 patients were discharged from hospitals with the nephrotic syndrome and 898,253,000 patients did not have the nephrotic syndrome. With the nephrotic syndrome, 5000 (0.5%) had pulmonary embolism, 14,000 (1.5%) had deep venous thrombosis, and fewer than 5000 had renal vein thrombosis. The relative risk of pulmonary embolism comparing patients with the nephrotic syndrome to those who did not have it was 1.39, and the relative risk of deep venous thrombosis was 1.72. Among patients aged 18-39 years, the relative risk of deep venous thrombosis was 6.81. From 1991-2005, after venous ultrasound was generally available, the relative risk of deep venous thrombosis (all ages) was 1.77. The nephrotic syndrome is a risk factor for venous thromboembolism. This is strikingly apparent in young adults. Renal vein thrombosis was uncommon. Therefore, pulmonary embolism, if it occurs, is likely to be due to deep venous thrombosis and not renal vein thrombosis.
Letter: Incidence of coronary heart disease associated with nephrotic syndrome
Gilboa N.
The increased risk of coronary heart disease associated with nephrotic syndrome
The increased risk of coronary heart disease associated with nephrotic syndrome. Patients with nephrotic syndrome (NS) are believed to be at increased risk of atherosclerosis and coronary heart disease (CHD), although existing evidence for this association has not been persuasive. The risk of CHD among 142 persons with NS documented by proteinuria 3.5 g daily was compared with that among 142 matched controls randomly selected from the membership of a large Northern California health plan. Controls were matched for sex, year of birth, and presence in the health plan when the referent case was diagnosed. No diabetics were included in this study. Mean follow-up for nonfatal CHD events was 5.6 years for NS subjects and 11.2 years for controls. Among the NS subjects myocardial infarction (MI) developed in 11, and there were 58 deaths, seven because of CHD. Among the controls, there were four MIs and 10 deaths, three because of CHD. In matched-pair analysis, there were 11 MIs among NS subjects and none among controls [P = 0.001, lower bound of 95% confidence interval for relative risk (CI), 2.8]. In an unmatched analysis adjusted for hypertension and smoking at diagnosis of NS, the relative risk of MI was 5.5 (95% CI 1.6 to 18.3) and the relative risk of coronary death was 2.8 (95% CI 0.7 to 11.3). Omitting data of NS subjects with minimal change disease and systemic lupus erythematosus yielded similar results. These data suggest that persons with NS are at increased risk of CHD.
Does the nephrotic syndrome increase the risk of cardiovascular disease?
Cardiovascular mortality and morbidity were assessed, after a mean follow-up period of 5 years, in an unselected series of 159 adults presenting with the nephrotic syndrome between 1972 and 1975. 60% of the deaths were attributed to terminal renal failure, and the incidence of deaths from isch03mic heart-disease (IHD) was not significantly above normal. The proportion of patients experiencing angina and intermittent claudication and the prevalence of isch03mic electrocardiographic changes did not differ significantly from those of a London control population. At follow-up, hypertension was significantly more common (p<0·001) in male nephrotic patients than in controls. Earlier reports of a greatly increased incidence of IHD in unselected patients with the nephrotic syndrome were not confirmed. Routine treatment of hyperlipid03mia in the nephrotic syndrome is not, therefore, recommended.
High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study
Abstract BACKGROUND: No data are available on the absolute risk of either venous thromboembolism (VTE) or arterial thromboembolism (ATE) in patients with nephrotic syndrome. Reported risks are based on multiple case reports and small studies with mostly short-term follow-up. We assessed the absolute risk of VTE and ATE in a large, single-center, retrospective cohort study and attempted to identify predictive factors in these patients. METHODS AND RESULTS: A total of 298 consecutive patients with nephrotic syndrome (59% men; mean age, 42+/-18 years) were enrolled. Mean follow-up was 10+/-9 years. Nephrotic syndrome was defined by proteinuria > or =3.5 g/d, and patients were classified according to underlying histological lesions accounting for nephrotic syndrome. Objectively verified symptomatic thromboembolic events were the primary study outcome. Annual incidences of VTE and ATE were 1.02% (95% confidence interval, 0.68 to 1.46) and 1.48% (95% confidence interval, 1.07 to 1.99), respectively. Over the first 6 months of follow-up, these rates were 9.85% and 5.52%, respectively. Proteinuria and serum albumin levels tended to be related to VTE; however, only the predictive value of the ratio of proteinuria to serum albumin was significant (hazard ratio, 5.6; 95% confidence interval, 1.2 to 26.2; P=0.03). In contrast, neither the degree of proteinuria nor serum albumin levels were related to ATE. Sex, age, hypertension, diabetes, smoking, prior ATE, and estimated glomerular filtration rate predicted ATE (P< or =0.02). CONCLUSIONS: This study verifies high absolute risks of symptomatic VTE and ATE that were remarkably elevated within the first 6 months. Whereas the ratio of proteinuria to serum albumin predicted VTE, estimated glomerular filtration rate and multiple classic risk factors for atherosclerosis were predictors of ATE.
Patients with primary membranous nephropathy are at high risk of cardiovascular events
Here we conducted a retrospective study to examine the risk of cardiovascular events (CVEs) relative to that of end-stage renal disease (ESRD) in patients with primary membranous nephropathy, in a discovery cohort of 404 patients. The cumulative incidence of CVEs was estimated in the setting of the competing risk of ESRD with risk factors for CVEs assessed by multivariable survival analysis. The observed cumulative incidences of CVEs were 4.4%, 5.4%, 8.2%, and 8.8% at 1, 2, 3, and 5 years respectively in the primary membranous nephropathy cohort. In the first 2 years after diagnosis, the risk for CVEs was similar to that of ESRD in the entire cohort, but exceeded it among patients with preserved renal function. Accounting for traditional risk factors and renal function, the severity of聽nephrosis at the time of the event (hazard ratio 2.1, 95% confidence interval 1.1 to 4.3) was a significant independent risk factor of CVEs. The incidence and risk factors of CVEs were affirmed in an external validation cohort of 557 patients with primary membranous nephropathy. Thus early in the course of disease, patients with primary membranous nephropathy have an increased risk of CVEs commensurate to, or exceeding that of ESRD. Hence, reduction of CVEs should be considered as a therapeutic outcome measure and focus of intervention in primary membranous nephropathy.
A new equation to estimate glomerular filtration rate
Abstract BACKGROUND: Equations to estimate glomerular filtration rate (GFR) are routinely used to assess kidney function. Current equations have limited precision and systematically underestimate measured GFR at higher values. OBJECTIVE: To develop a new estimating equation for GFR: the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. DESIGN: Cross-sectional analysis with separate pooled data sets for equation development and validation and a representative sample of the U.S. population for prevalence estimates. SETTING: Research studies and clinical populations ("studies") with measured GFR and NHANES (National Health and Nutrition Examination Survey), 1999 to 2006. PARTICIPANTS: 8254 participants in 10 studies (equation development data set) and 3896 participants in 16 studies (validation data set). Prevalence estimates were based on 16,032 participants in NHANES. MEASUREMENTS: GFR, measured as the clearance of exogenous filtration markers (iothalamate in the development data set; iothalamate and other markers in the validation data set), and linear regression to estimate the logarithm of measured GFR from standardized creatinine levels, sex, race, and age. RESULTS: In the validation data set, the CKD-EPI equation performed better than the Modification of Diet in Renal Disease Study equation, especially at higher GFR (P < 0.001 for all subsequent comparisons), with less bias (median difference between measured and estimated GFR, 2.5 vs. 5.5 mL/min per 1.73 m(2)), improved precision (interquartile range [IQR] of the differences, 16.6 vs. 18.3 mL/min per 1.73 m(2)), and greater accuracy (percentage of estimated GFR within 30% of measured GFR, 84.1% vs. 80.6%). In NHANES, the median estimated GFR was 94.5 mL/min per 1.73 m(2) (IQR, 79.7 to 108.1) vs. 85.0 (IQR, 72.9 to 98.5) mL/min per 1.73 m(2), and the prevalence of chronic kidney disease was 11.5% (95% CI, 10.6% to 12.4%) versus 13.1% (CI, 12.1% to 14.0%). LIMITATION: The sample contained a limited number of elderly people and racial and ethnic minorities with measured GFR. CONCLUSION: The CKD-EPI creatinine equation is more accurate than the Modification of Diet in Renal Disease Study equation and could replace it for routine clinical use. PRIMARY FUNDING SOURCE: National Institute of Diabetes and Digestive and Kidney Diseases.
Idiopathic membranous nephropathy: definition and relevance of a partial remission
A partial remission is an important therapeutic target with implications for both progression rate and renal survival.
The nephrotic syndrome, lipids, and risk factors for cardiovascular disease
The hyperlipidemia associated with the nephrotic syndrome is well characterized. There is, however, a paucity of data in humans on the risk factors for atherosclerotic heart disease and the role of hyperlipidemia on the risk of progression of renal disease in this population. In our study, we retrospectively evaluated a large uniform population of patients (mean creatinine, 1.78 mg/dL; mean 24-hour proteinuria, 7.1 g) with idiopathic nephrotic syndrome for the presence of risk factors for coronary artery disease. One hundred patients with either focal segmental glomerulosclerosis (n = 56) or membranous nephropathy (n = 44) were assessed for the following cardiovascular risk factors: male sex or postmenopausal female, hyperlipidemia, hypertension, smoking history, and left ventricular hypertrophy. Sixty-six percent of the patients were either male or postmenopausal females; 35% were smokers. Hypertension and left ventricular hypertrophy were present in 53% and 13% of patients, respectively. Eighty-seven percent, 53%, and 25% of patients had a total cholesterol of more than 200 mg/dL, more than 300 mg/dL, and more than 400 mg/dL, respectively. Low-density lipoprotein cholesterol was greater than 130 mg/dL and greater than 160 mg/dL in 77.2% and 64.9% of patients, respectively. Virtually all patients (99%) had at least one risk factor for cardiovascular disease; over two thirds (68%) had two risk factors and over one quarter (26%) had three risk factors. In comparing the group that progressed to renal failure with the groups that did not, the initial mean serum cholesterol was lower in the group that progressed (292 mg/dL v 388 mg/dL, P < 0.01).(ABSTRACT TRUNCATED AT 250 WORDS)
Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences
Nephrotic syndrome results in hyperlipidemia and profound alterations in lipid and lipoprotein metabolism. Serum cholesterol, triglycerides, apolipoprotein B (apoB)–containing lipoproteins (very low-density lipoprotein [VLDL], immediate-density lipoprotein [IDL], and low-density lipoprotein [LDL]), lipoprotein(a) (Lp[a]), and the total cholesterol/high-density lipoprotein (HDL) cholesterol ratio are increased in nephrotic syndrome. This is accompanied by significant changes in the composition of02various lipoproteins including their cholesterol-to-triglyceride, free cholesterol–to-cholesterol ester, and phospholipid-to-protein ratios. These abnormalities are mediated by changes in the expression and activities of the02key proteins involved in the biosynthesis, transport, remodeling, and catabolism of lipids and lipoproteins including apoproteins A, B, C, and E; 3-hydroxy-3-methylglutaryl-coenzyme A reductase; fatty acid synthase; LDL receptor; lecithin cholesteryl ester acyltransferase; acyl coenzyme A cholesterol acyltransferase; HDL docking receptor (scavenger receptor class B, type 1 [SR-B1]); HDL02endocytic receptor; lipoprotein lipase; and hepatic lipase, among others. The disorders of lipid and lipoprotein metabolism in nephrotic syndrome contribute to the development and progression of cardiovascular and kidney disease. In addition, by limiting delivery of lipid fuel to the02muscles for generation of energy and to the adipose tissues for storage of energy, changes in lipid metabolism contribute to the reduction of body mass and impaired exercise capacity. This article provides an overview of the02mechanisms, consequences, and treatment of lipid disorders in nephrotic syndrome.
Renal artery thrombosis with renal infarction: a rare cause of acute abdomen
Renal artery thrombosis with renal infarction is a rare entity. Due to the nonspecific clinical presentation, the diagnosis is usually delayed. We describe such a case in a middle-aged man with membranous nephropathy who was in remission and presented with severe abdominal pain. He was managed with selective intra-arterial thrombolysis with a good outcome.
Arterial thrombosis in nephrotic syndrome
過度凝血是腎病症候群患者常見的併發症。靜脈系統較常受影響,而動脈栓塞則較少見。患者截肢率及死亡率均相當高。多種因素都與此狀況下的血栓栓塞有關。我們報告一自發性之股動脈椎塞,手術去除栓塞之後又復發的病例。再次手術併使用新鮮冷凍血漿才成功地治癒此病例。我們建議,在治療腎病症候群患者之動脈椎塞時除了積極地血栓去除術及足量的抗凝血劑外,還應以新鮮冷凍血漿補充抗凝血酶。
Carotid thromboembolism associated with nephrotic syndrome treated with dabigatran
Nephrotic syndrome (NS) may be complicated by thromboembolism, which occasionally manifests as stroke. Although the optimal, standardized approach to the prophylaxis and management of thromboembolic complications associated with NS has not been established, anticoagulation with heparin and subsequent warfarin is the de facto standard of treatment. Dabigatran, a novel direct thrombin inhibitor, has become a substitute for warfarin and heparin for many indications, including the prophylaxis of stroke associated with nonvalvular atrial fibrillation and postoperative thromboprophylaxis in orthopedic patients. We report a 35-year-old male with NS due to membranous nephropathy (MN) that presented with carotid thromboembolism. Because the patient developed drug-induced hepatitis due to warfarin, we attempted treatment with dabigatran and were successful in continuing the medication without any complications. We also reviewed the literature on stroke associated with NS. Twenty-one prior cases have been reported, and the review of these cases revealed some interesting points. The age of onset ranged from 19 to 59 years. Most of the reported cases sustained a stroke at earlier ages than patients with atherosclerosis and atrial fibrillation, which suggests that NS may independently predispose individuals to arterial and venous thromboses. MN was the most common underlying pathology. Given that a standardized approach to the prophylaxis and management of thrombotic complications associated with NS has not been established, our experience suggests that dabigatran is a valid new treatment option for thrombotic complications of NS. u00a9 2014 S. Karger AG, Basel
Thromboembolic complications in the nephrotic syndrome: pathophysiology and clinical management
Patients with the nephrotic syndrome are at increased risk of developing venous and arterial thromboembolism, the most common of which is renal vein thrombosis. There are several unanswered or controversial issues relating to the nephrotic syndrome and thromboembolism, which include the mechanism of thromboembolism, and optimal diagnostic and anticoagulant management strategies. This review will discuss several of these issues: the epidemiology and clinical spectrum of thromboembolic disease occurring in patients with the nephrotic syndrome; the pathophysiology of the hypercoagulable state associated with the nephrotic syndrome; the diagnosis of renal vein thrombosis in the nephrotic syndrome; and the evidence for prophylactic and therapeutic anticoagulation strategies in such patients.
Thromboembolic complications in membranous nephropathy patients with nephrotic syndrome-a prospective study
Venous thromboembolism (VTE) is one of the most serious complications in membranous nephropathy (MN). We investigate the incidence of VTE in MN patients with nephrotic syndrome (NS). A total of 100 MN patients with NS were enrolled into this prospective study. The diagnosis of VTE was based on contrast-enhanced dual source computed tomography angiography. Venous thromboembolism was demonstrated in 36 patients (36%). 33 patients (33%) had renal vein thrombosis (RVT), 17 patients (17%) had pulmonary embolism (PE). Flank pain was noted in 5 patients and gross hematuria in 2 patients with RVT. Dyspnea and chest pain were present in 9 patients with PE. The positive predictive value for D-dimer level was 69.4%, negative predictive value for D-dimer level was 96.1% in patients with MN. Of all the risk factors presented, D-dimer level, proteinuria, the ratio of proteinuria to serum albumin were independent risk factors for the development of VTE (P<0.05), but the plasma level of antithrombin was not correlated with VTE in this study. In follow up, venous thrombosis disappeared after anticoagulant treatment with low-molecular-weight heparins in 28 patients. Venous thromboembolism was confirmed in 36% of MN patients with NS. Renal vein thrombosis and pulmonary embolism are common and usually asymptomatic. Computed tomography angiography can be used effectively to examine suspected patients. Measurement of D-dimer is helpful in VTE diagnosis. It is important that clinicians are aware that VTE should be considered as a common complication in MN patients with NS.
Venous thromboembolism in patients with membranous nephropathy
The aims of this study were to determine the frequency of venous thromboembolic events in a large cohort of patients with idiopathic membranous nephropathy and to identify predisposing risk factors. We studied patients with biopsy-proven membranous nephropathy from the Glomerular Disease Collaborative Network (n=412) and the Toronto Glomerulonephritis Registry (n=486) inception cohorts. The cohorts were pooled after establishing similar baseline characteristics (total n=898). Clinically apparent and radiologically confirmed venous thromboembolic events were identified. Potential risk factors were evaluated using multivariable logistic regression models. Sixty-five (7.2%) subjects had at least one venous thromboembolic event, and this rate did not differ significantly between registries. Most venous thromboembolic events occurred within 2 years of first clinical assessment (median time to VTE = 3.8 months). After adjusting for age, sex, proteinuria, and immunosuppressive therapy, hypoalbuminemia at diagnosis was the only independent predictor of a venous thromboembolic event. Each 1.0 g/dl reduction in serum albumin was associated with a 2.13-fold increased risk of VTE. An albumin level <2.8 g/dl was the threshold below which risk for a venous thromboembolic event was greatest. We conclude that clinically apparent venous thromboembolic events occur in about 7% of patients with membranous nephropathy. Hypoalbuminemia, particularly <2.8 g/dl, is the most significant independent predictor of venous thrombotic risk.
Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome
Focuses on the prevalence of thromboembolic phenomena and renal vein thrombosis as complications of patients with nephrotic syndrome. Incidence of the complications in patients; Association of nephrotic syndrome with a hypercoagulable state; Potential of changes in blood coagulation factors as predictor of thromboembolic complications.
Membranous nephropathy and thromboembolism: is prophylactic anticoagulation warranted?
Bellomo R, Atkins RC.