Chinese Medical Sciences Journal ›› 2021, Vol. 36 ›› Issue (4): 284-294.doi: 10.24920/003803
• Original Articles • Previous Articles Next Articles
Does Prior Cancer Have an Influence on the Survival Outcomes of Patients with Localized Pancreatic Neuroendocrine Tumors?
Liang Wang, Gang Li, Yun-tao Bing, Mao-lin Tian, Hangyan Wang( ), Chunhui Yuan(
), Chunhui Yuan( ), Dianrong Xiu(
), Dianrong Xiu( )
)
- Department of General Surgery, Peking University Third Hospital, Beijing 100191, China
-
Received:2020-07-09Published:2021-12-31Online:2021-10-09 -
Contact:Hangyan Wang,Chunhui Yuan,Dianrong Xiu E-mail:wanghangyan111@163.com;yuanchunhui1971@163.com;xiudianrong1964@163.com
Cite this article
Liang Wang, Gang Li, Yun-tao Bing, Mao-lin Tian, Hangyan Wang, Chunhui Yuan, Dianrong Xiu. Does Prior Cancer Have an Influence on the Survival Outcomes of Patients with Localized Pancreatic Neuroendocrine Tumors?[J].Chinese Medical Sciences Journal, 2021, 36(4): 284-294.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1
Characteristics of patients with localized PanNET included in the study [n (%)]"
| Variables | Before PSM | After PSM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NPC | PC | χ2 | P | NPC | PC | χ2 | P | ||
| n | 1211 | 133 | 266 | 133 | |||||
| Age (yrs) | 38.93 | <0.001 | 0.187 | 0.667 | |||||
| ≤65 | 836 (69.0) | 56 (42.1) | 106 (39.8) | 56 (42.1) | |||||
| >65 | 375 (31.0) | 77 (57.9) | 160 (60.2) | 77 (57.9) | |||||
| Gender | 0.347 | 0.584 | 0.005 | 1.000 | |||||
| Male | 623 (51.4) | 72 (54.1) | 145 (54.5) | 72 (54.1) | |||||
| Female | 588 (48.6) | 61 (45.9) | 121 (45.5) | 61 (45.9) | |||||
| Race | 0.183 | 0.913 | 0.367 | 0.832 | |||||
| White | 943 (77.9) | 102 (76.7) | 211 (79.3) | 102 (76.7) | |||||
| Black | 131 (10.8) | 16 (12.0) | 28 (10.5) | 16 (12.0) | |||||
| Other | 137 (11.3) | 15 (11.3) | 27 (10.2) | 15 (11.3) | |||||
| Marital status | 0.624 | 0.437 | 0.024 | 0.907 | |||||
| Married | 815 (67.3) | 94 (70.7) | 190 (71.4) | 94 (70.7) | |||||
| Unmarried | 396 (32.7) | 39 (29.3) | 76 (28.6) | 39 (29.3) | |||||
| Year of diagnosis | 0.049 | 0.368 | 0.649 | ||||||
| 1973-2010 | 240 (19.8) | 17 (12.8) | 40 (15.0) | 17 (12.8) | |||||
| 2011-2015 | 971 (80.2) | 116 (87.2) | 226 (85.0) | 116 (87.2) | |||||
| Tumor site (pancreas) | 3.836 | 0.428 | 1.234 | 0.745 | |||||
| Head | 294 (24.3) | 34 (25.6) | 61 (22.9) | 34 (25.6) | |||||
| Body/tail | 707 (58.4) | 75 (56.4) | 165 (62.0) | 75 (56.4) | |||||
| Overlap | 68 (5.6) | 4 (3.0) | 7 (2.6) | 4 (3.0) | |||||
| Other | 142 (11.7) | 20 (15.0) | 33 (12.4) | 20 (15.0) | |||||
| Histological grade | 6.252 | 0.025 | 0.130 | 0.788 | |||||
| Well/moderately | 1193 (98.5) | 127 (95.5) | 256 (96.2) | 127 (95.5) | |||||
| Poorly/undifferentiated | 18 (1.5) | 6 (4.5) | 10 (3.8) | 6 (4.5) | |||||
| Tumor size (cm) | 4.283 | 0.117 | 0.242 | 0.886 | |||||
| ≤2 | 657 (54.3) | 82 (61.7) | 159 (59.8) | 82 (61.7) | |||||
| 2-4 | 360 (29.7) | 38 (28.6) | 77 (28.9) | 38 (28.6) | |||||
| >4 | 194 (16.0) | 13 (9.8) | 30 (11.3) | 13 (9.8) | |||||
| Primary site surgery | 9.990 | 0.003 | 0.000 | 1.000 | |||||
| No | 126 (10.4) | 26 (19.5) | 52 (19.5) | 26 (19.5) | |||||
| Yes | 1085 (89.6) | 107 (80.5) | 214 (80.5) | 107 (80.5) | |||||

Figure 3.
Overall survival and cancer-specific survival in localized PanNET patients with and without prior cancers before and after PSM. (A) Kaplan-meier analysis for overall survival in patients with and without prior cancers before PSM; (B) Kaplan-meier analysis for cancer-specific survival in patients with and without prior cancers before PSM; (C) Kaplan-meier analysis for overall survival in patients with and without prior cancers after PSM; (D) Kaplan-meier analysis for cancer-specific survival in patients with and without prior cancers after PSM."
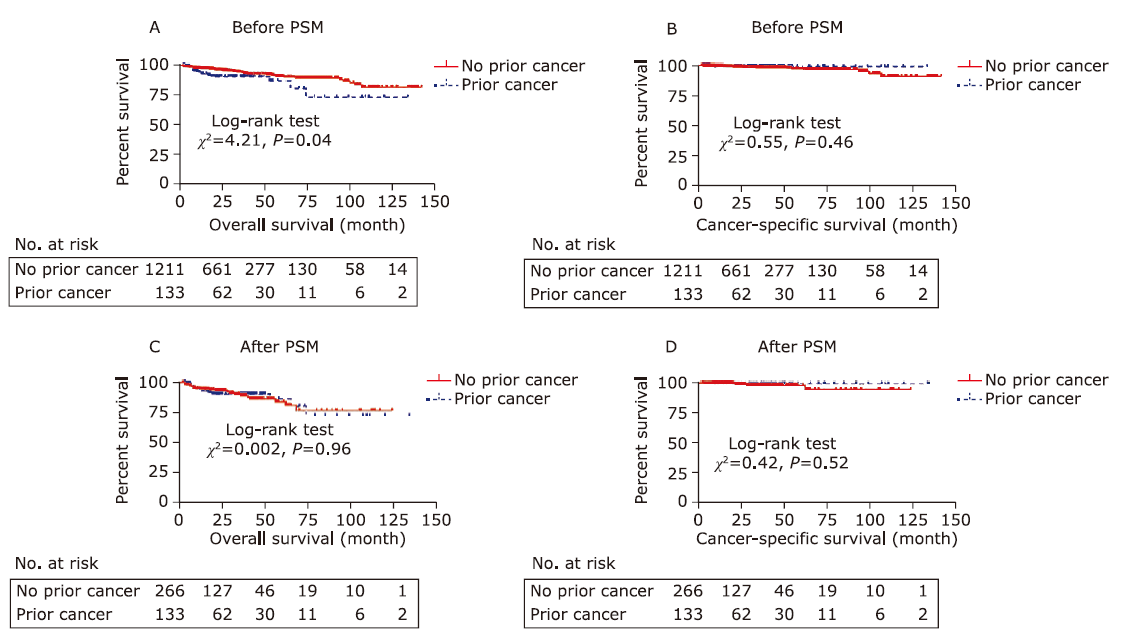
Table 2
Results of univariate and multi-variate Cox proportional hazard regression analyses for overall survival"
| Variables | Before PSM | After PSM | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate analysis (P value) | Multivariate analysis | Univariate analysis (P value) | Multivariate analysis | |||||||||||
| Estimtes of coefficient of correlation | Standard error | Wald χ2 | HR | 95%CI | P | Estimtes of coefficient of correlation | Standard error | Wald χ2 | HR | 95%CI | P | |||
| Prior cancer | 0.060 | 0.347 | 0.964 | |||||||||||
| No | ||||||||||||||
| Yes | ||||||||||||||
| Age (yrs) | 0.000 | 0.000 | 0.053 | 0.178 | ||||||||||
| ≤65 | 1 (Referent) | |||||||||||||
| >65 | 1.219 | 0.234 | 27.19 | 3.383 | 2.140-5.348 | 0.000 | ||||||||
| Gender | 0.115 | 0.210 | 0.510 | |||||||||||
| Male | ||||||||||||||
| Female | ||||||||||||||
| Race | 0.844 | 0.305 | ||||||||||||
| White | ||||||||||||||
| Black | ||||||||||||||
| Other | ||||||||||||||
| Marital status | 0.364 | 0.659 | ||||||||||||
| Married | ||||||||||||||
| Unmarried | ||||||||||||||
| Year of diagnosis | 0.400 | 0.527 | ||||||||||||
| 1973-2010 | ||||||||||||||
| 2011-2015 | ||||||||||||||
| Tumor site | 0.904 | 0.491 | ||||||||||||
| Head | ||||||||||||||
| Body or tail | ||||||||||||||
| Other | ||||||||||||||
| Histological grade | 0.002 | 0.002 | 0.001 | 0.000 | ||||||||||
| Well/moderately | 1 (Referent) | 1 (Referent) | ||||||||||||
| Poorly/undifferentiated | 1.222 | 0.399 | 9.378 | 3.396 | 1.553-7.425 | 1.615 | 0.453 | 12.69 | 5.028 | 2.068-12.228 | 0.000 | |||
| Tumor size (cm) | 0.021 | 0.016 | 0.956 | |||||||||||
| ≤2 | 1 (Referent) | |||||||||||||
| 2-4 | -0.008 | 0.272 | 0.001 | 0.992 | 0.582-1.691 | 0.978 | ||||||||
| >4 | 0.695 | 0.264 | 6.929 | 2.004 | 1.194-3.362 | 0.008 | ||||||||
| Primary site surgery | 0.000 | 0.000 | 0.000 | 0.000 | ||||||||||
| No | 1 (Referent) | 1 (Referent) | ||||||||||||
| Yes | -1.554 | 0.237 | 43.042 | 0.211 | 0.133-0.336 | 0.000 | -1.532 | 0.339 | 20.474 | 0.216 | 0.111-0.420 | 0.000 | ||
Table 3
Results of univariate and multi-variate Cox proportional hazard regression analyses for cancer specific survival"
| Variables | Before PSM | After PSM | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate analysis (P value) | Multivariate analysis | Univariate analysis (P value) | Multivariate analysis | |||||||||||
| Estimtes of coefficient of correlation | Standard error | Wald χ2 | HR | 95.0% CI | P | Estimtes of coefficient of correlation | Standard error | Wald χ2 | HR | 95.0% CI | P | |||
| Prior cancer | 0.418 | 0.500 | ||||||||||||
| No | ||||||||||||||
| Yes | ||||||||||||||
| Age (yrs) | 0.002 | 0.812 | ||||||||||||
| ≤65 | 1(Referent) | |||||||||||||
| >65 | 2.958 | 1.228-7.127 | 0.016 | |||||||||||
| Gender | 0.525 | 0.167 | ||||||||||||
| Male | ||||||||||||||
| Female | ||||||||||||||
| Race | 0.979 | 0.260 | ||||||||||||
| White | ||||||||||||||
| Black | ||||||||||||||
| Other | ||||||||||||||
| Marital status | 0.621 | 0.662 | ||||||||||||
| Married | ||||||||||||||
| Unmarried | ||||||||||||||
| Year of diagnosis | 0.011 | 0.890 | ||||||||||||
| 1973-2010 | 1(Referent) | |||||||||||||
| 2011-2015 | 1.290 | 0.533 | 5.864 | 3.633 | 1.279-10.320 | 0.015 | ||||||||
| Tumor site | 0.615 | 0.480 | ||||||||||||
| Head | ||||||||||||||
| Body or tail | ||||||||||||||
| Other | ||||||||||||||
| Histological grade | 0.001 | 0.000 | 0.000 | |||||||||||
| Well/moderately | 1(Referent) | 1(Referent) | ||||||||||||
| Poorly/undifferentiated | 2.191 | 0.573 | 14.635 | 8.945 | 2.911-27.486 | 0.000 | 3.746 | 0.941 | 15.844 | 42.33 | 6.694-267.7 | 0.000 | ||
| Tumor size (cm) | 0.012 | 0.682 | ||||||||||||
| ≤2 | 1(Referent) | |||||||||||||
| 2-4 | 0.183 | 0.591 | 0.096 | 1.201 | 0.377-3.828 | 0.757 | ||||||||
| >4 | 1.159 | 0.544 | 4.545 | 3.186 | 1.098-9.245 | 0.033 | ||||||||
| Primary site surgery | 0.000 | 0.000 | 0.017 | |||||||||||
| No | 1(Referent) | 1(Referent) | ||||||||||||
| Yes | -1.835 | 0.468 | 15.40 | 0.160 | 0.064-0.399 | 0.000 | -2.256 | 0.984 | 5.259 | 0.105 | 0.015-0.720 | 0.022 | ||

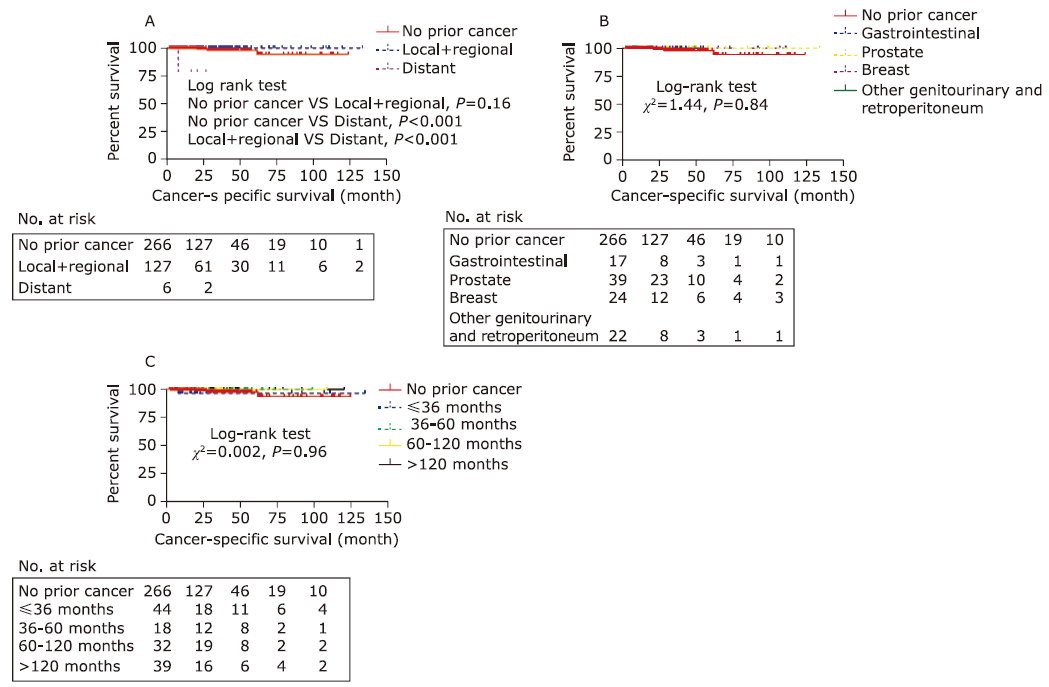
Figure 4.
Kaplan-Meier analysis for cancer-specific survival stratified by the clinical stage, site of the prior cancers, and interval period groups. (A) Kaplan-Meier analysis for cancer-specific survival stratified by the clinical stage of prior cancer; (B) Kaplan-Meier analysis for cancer-specific survival stratified by the site of prior cancer; (C) Kaplan-Meier analysis for cancer-specific survival stratified by the interval month groups."
| 1. |
Halfdanarson TR, Rabe KG, Rubin J, et al. Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol 2008; 19(10):1727-33. doi: 10.1093/annonc/mdn351.
doi: 10.1093/annonc/mdn351 pmid: 18515795 |
| 2. |
Lepage C, Bouvier AM, Phelip JM, et al. Incidence and management of malignant digestive endocrine tumours in a well defined French population. Gut 2004; 53(4):549-53. doi: 10.1136/gut.2003.026401.
doi: 10.1136/gut.2003.026401 pmid: 15016750 |
| 3. |
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008; 26(18):3063-72. doi: 10.1200/JCO.2007.15.4377.
doi: 10.1200/JCO.2007.15.4377 |
| 4. |
Das S, Dasari A. Epidemiology, incidence, and prevalence of neuroendocrine neoplasms: are there global differences?. Curr Oncol Rep 2021; 23(4):43. doi: 10.1007/s11912-021-01029-7.
doi: 10.1007/s11912-021-01029-7 |
| 5. |
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 2017; 3(10):1335-42. doi: 10.1001/jamaoncol.2017.0589.
doi: 10.1001/jamaoncol.2017.0589 |
| 6. |
Bilimoria KY, Tomlinson JS, Merkow RP, et al. Clinicopathologic features and treatment trends of pancreatic neuroendocrine tumors: analysis of 9, 821 patients. J Gastrointest Surg 2007; 11(11):1460-7; discussion 1467-9. doi: 10.1007/s11605-007-0263-3.
doi: 10.1007/s11605-007-0263-3 |
| 7. |
Donin N, Filson C, Drakaki A, et al. Risk of second primary malignancies among cancer survivors in the United States, 1992 through 2008. Cancer 2016; 122(19):3075-86. doi: 10.1002/cncr.30164.
doi: 10.1002/cncr.30164 |
| 8. |
Michaud DS, Giovannucci E, Willett WC, et al. Physical activity, obesity, height, and the risk of pancreatic cancer. JAMA 2001; 286(8):921-9. doi: 10.1001/jama. 286.8.921.
doi: 10.1001/jama. 286.8.921 |
| 9. |
Olson SH, Kurtz RC. Epidemiology of pancreatic cancer and the role of family history. J Clin Oncol 2013; 107(1):1-7. doi: 10.1002/jso.23149.
doi: 10.1002/jso.23149 |
| 10. |
Shahar T, Nossek E, Steinberg DM, et al. The impact of enrollment in clinical trials on survival of patients with glioblastoma. J Clin Neurosci 2012; 19(11):1530-34. doi: 10.1016/j.jocn.2012.04.005.
doi: 10.1016/j.jocn.2012.04.005 pmid: 22989795 |
| 11. |
Laccetti AL, Pruitt SL, Xuan L, et al. Effect of prior cancer on outcomes in advanced lung cancer: implications for clinical trial eligibility and accrual. J Natl Cancer Inst 2015; 107(4):djv002. doi: 10.1093/jnci/djv002.
doi: 10.1093/jnci/djv002 |
| 12. |
Laccetti AL, Pruitt SL, Xuan L, et al. Prior cancer does not adversely affect survival in locally advanced lung cancer: a national SEER-medicare analysis. Lung Cancer 2016; 98:106-13. doi: 10.1016/j. lungcan.2016.05.029.
doi: S0169-5002(16)30355-5 pmid: 27393515 |
| 13. |
Al-Husseini MJ, Saad AM, El-Shewy KM, et al. Prior malignancy impact on survival outcomes of glioblastoma multiforme; population-based study. Int J Neurosci 2019; 129(5):447-54. doi: 10.1080/00207454.2018.1538989.
doi: 10.1080/00207454.2018.1538989 pmid: 30366515 |
| 14. |
Duhamel A, Labreuche J, Gronnier C, et al. Statistical tools for propensity score matching. Ann Surg 2017; 265(6):E79-e80. doi: 10.1097/sla.0000000000001312.
doi: 10.1097/sla.0000000000001312 |
| 15. |
Morgan CJ. Reducing bias using propensity score matching. J Nucl Cardiol 2018; 25(2):404-6. doi: 10.1007/s12350-017-1012-y.
doi: 10.1007/s12350-017-1012-y |
| 16. |
Li G, Tian ML, Bing YT, et al. Impact of a prior nonpancreatic malignancy on survival outcomes of patients with stage Ⅳ pancreatic neuroendocrine tumor: a population-based and propensity score matching study. Pancreas 2020; 49(8):1090-8. doi: 10.1097/MPA.0000000000001630.
doi: 10.1097/MPA.0000000000001630 |
| 17. |
Shen M, Boffetta P, Olsen JH, et al. A pooled analysis of second primary pancreatic cancer. Am J Epidemiol 2006; 163(6):502-11. doi: 10.1093/aje/kwj073.
doi: 10.1093/aje/kwj073 pmid: 16421239 |
| 18. |
Sara JS, Lindsay MM, Amy B, et al. Risk of second primary papillary thyroid cancer among adult cancer survivors in the United States, 2000-2015. Cancer Epidemiol 2020; 64:101664. doi: 10.1016/j.canep.2019.101664.
doi: 10.1016/j.canep.2019.101664 |
| 19. |
Sung H, Hyun N, Leach CR, et al. Association of first primary cancer with risk of subsequent primary cancer among survivors of adult-onset cancers in the United States. JAMA 2020; 324(24):2521-35. doi: 10.1001/jama.2020.23130.
doi: 10.1001/jama.2020.23130 |
| 20. |
Ross S, Grant A, Counsell C, et al. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol 1999; 52(12):1143-56.
pmid: 10580777 |
| 21. |
Al-Husseini MJ, Saad AM, Turk T, et al. Impact of prior malignancy on survival outcomes of stage Ⅳ pancreatic adenocarcinoma: SEER-Based Cohort. J Gastrointest cancer 2018; 50(4):794-800. doi: 10.1007/s12029-018-0158-4.
doi: 10.1007/s12029-018-0158-4 |
| 22. |
Jennifer LG. Inherited syndromes involving pancreatic neuroendocrine tumors. J Gastrointest Oncol 2020; 11(3):559-66. doi: 10.21037/jgo.2020.03.09.
doi: 10.21037/jgo.2020.03.09 pmid: 32655935 |
| 23. |
Oberg K. The genetics of neuroendocrine tumors. Semin Oncol 2013; 40(1):37-44. doi: 10.1053/j.seminoncol.2012.11.005.
doi: 10.1053/j.seminoncol.2012.11.005 |
| [1] | Gang Li, Yuntao Bing, Maolin Tian, Chunhui Yuan, Dianrong Xiu. Using a Nomogram to Preoperatively Predict Distant Metastasis of Pancreatic Neuroendocrine Tumor in Elderly Patients [J]. Chinese Medical Sciences Journal, 2021, 36(3): 218-224. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|