Chinese Medical Sciences Journal ›› 2022, Vol. 37 ›› Issue (2): 151-158.doi: 10.24920/003870
• Original Article • Previous Articles Next Articles
Assessment of Changes in the Cesarean Scar and Uterus Between One and Two Years after Cesarean Section Using 3D T2w SPACE MRI
Yafei Qi1, Yonglan He1, Ning Ding1, Liangkun Ma2, Tianyi Qian3, Yuan Li2, Huadan Xue1, *( ), Zhengyu Jin1
), Zhengyu Jin1
- 1Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
2Department of Obstetrics and Gynecology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
3MR Collaborations NE Asia, Siemens Healthcare, Beijing 100102, China
-
Received:2020-12-20Accepted:2022-02-28Published:2022-06-30Online:2022-04-18 -
Contact:Huadan Xue E-mail:bjdanna95@163.com
Cite this article
Yafei Qi, Yonglan He, Ning Ding, Liangkun Ma, Tianyi Qian, Yuan Li, Huadan Xue, Zhengyu Jin. Assessment of Changes in the Cesarean Scar and Uterus Between One and Two Years after Cesarean Section Using 3D T2w SPACE MRI[J].Chinese Medical Sciences Journal, 2022, 37(2): 151-158.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
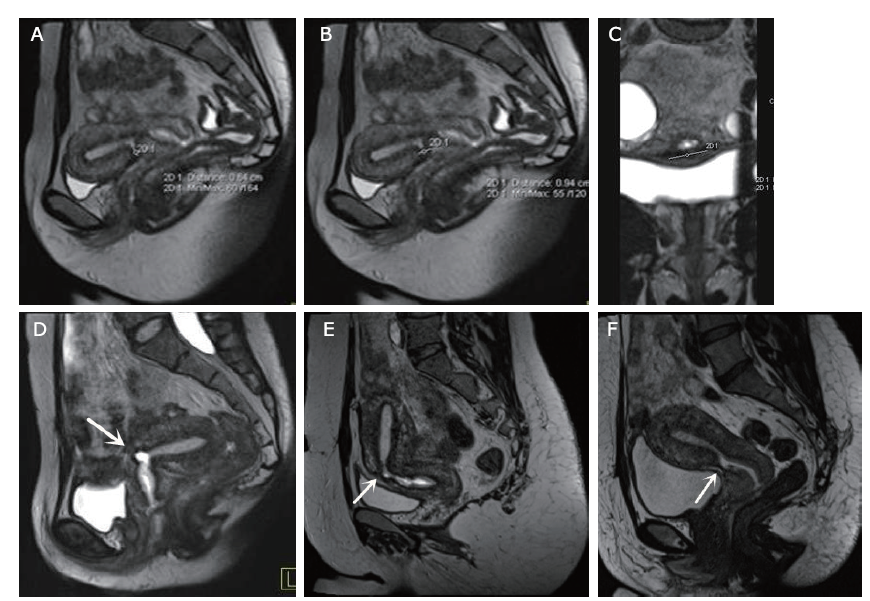
Figure 2.
Measurement of the thickness of the uterine anterior wall (A), uterine length and anteroposterior diameter (B), uterine width (C) on 3D T2w SPACE MRI. Forward angle between the uterus and cervix long axes less than 180 degrees is defined as uterus in anteflexion position (D). Forward angle between the uterus and cervix long axes larger than 180 degrees is defined as uterus in retroflexion position (E)."
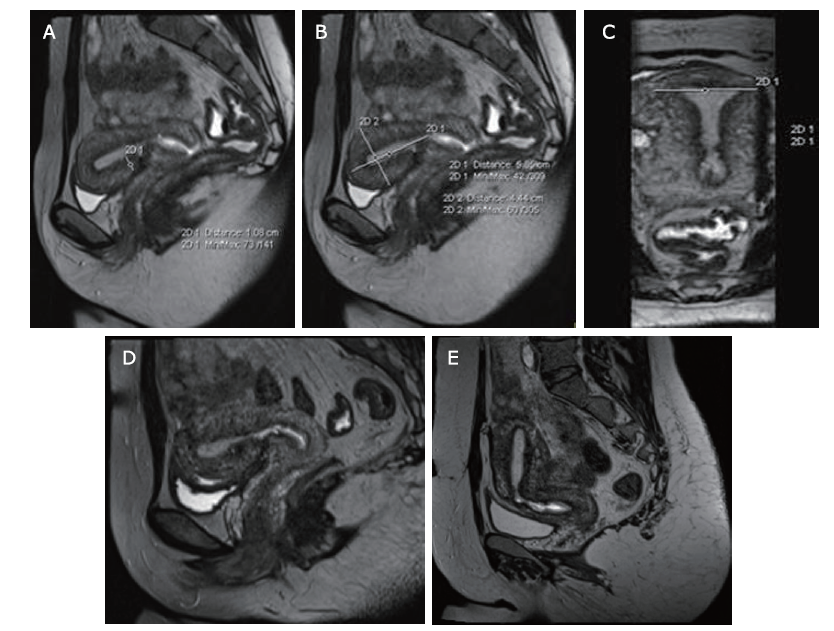
Table 1.
Characteristics of the 46 included volunteers"
| Items | Results |
|---|---|
| Time of CS (n) | |
| One | 39 |
| Two | 7 |
| Hysterorrhaphy at last delivery (n) | |
| One-layer suture | 35 |
| Two-layer suture | 10 |
| Absence of hysterorrhaphy record | 1 |
| Surgery approach (n) | |
| Elective surgery | 33 |
| Emergency surgery | 13 |
| Breastfeeding (n) | |
| More than one year | 30 |
| Less than one year | 16 |
| Menstruation after one year of CS (n) | |
| Regular | 40 |
| Irregular | 6 |
| Uterine position (n) | |
| Anteflexion | 36 |
| Retroflexion | 10 |
Table 3.
Comparisons of uterine morphology between one year and two years after CS (cm)"
| Groups | n | Thickness of the uterine anterior wall | Length of uterus | Anteroposterior diameter of uterus | Width of uterus |
|---|---|---|---|---|---|
| Control group | 13 | 1.58±0.21 | 5.22±0.74 | 4.04±0.42 | 5.02±0.62 |
| One-year after CS | 15 | 1.25±0.27* | 5.33±0.59 | 4.02±0.72 | 5.43±0.99 |
| Two-year after CS | 15 | 1.45±0.35 | 5.75±0.46 | 4.35±0.51 | 5.51±0.62 |
| 1. |
Varner M. Cesarean scar imaging and prediction of subsequent obstetric complications. Clin Obstet Gynecol 2012; 55(4):988-96. doi: 10.1097/GRF.0b013e318263c699.
doi: 10.1097/GRF.0b013e318263c699 |
| 2. |
Rodgers SK, Kirby CL, Smith RJ, et al. Imaging after cesarean delivery: acute and chronic complications. Radiographics 2012; 32(6):1693-712. doi: 10.1148/rg.326125516.
doi: 10.1148/rg.326125516 pmid: 23065165 |
| 3. |
Smith GC, Pell JP, Dobbie R. Interpregnancy interval and risk of preterm birth and neonatal death: retrospective cohort study. BMJ 2003; 327(7410):313. doi: 10.1136/bmj.327.7410.313.
doi: 10.1136/bmj.327.7410.313 |
| 4. |
Bujold E, Mehta SH, Bujold C, et al. Interdelivery interval and uterine rupture. Am J Obstet Gynecol 2002; 187(5):1199-202. doi: 10.1067/mob.2002.127138.
doi: 10.1067/mob.2002.127138 |
| 5. |
Shipp TD, Zelop CM, Repke JT, et al. Interdelivery interval and risk of symptomatic uterine rupture. Obstet Gynecol 2001; 97(2):175-7. doi: 10.1016/s0029-7844(00)01129-7.
doi: 10.1016/s0029-7844(00)01129-7 pmid: 11165577 |
| 6. |
Stamilio DM, DeFranco E, Paré E, et al. Short interpregnancy interval: risk of uterine rupture and complications of vaginal birth after cesarean delivery. Obstet Gynecol 2007; 110(5):1075-82. doi: 10.1097/01.AOG.0000286759.49895.46.
doi: 10.1097/01.AOG.0000286759.49895.46 pmid: 17978122 |
| 7. |
Wang LL, Chen JY, Yang HX, et al. Correlation between uterine scar condition and uterine rupture for pregnancy women after previous cesarean section. Zhonghua Fu Chan Ke Za Zhi 2019; 54(6):375-80. doi: 10.3760/cma.j.issn.0529-567x.2019.06.004.
doi: 10.3760/cma.j.issn.0529-567x.2019.06.004 |
| 8. |
Fiocchi F, Petrella E, Nocetti L, et al. Transvaginal ultrasound assessment of uterine scar after previous caesarean section: comparison with 3T-magnetic resonance diffusion tensor imaging. Radiol Med 2015; 120(2):228-38. doi: 10.1007/s11547-014-0431-y.
doi: 10.1007/s11547-014-0431-y |
| 9. |
Swift BE, Shah PS, Farine D. Sonographic lower uterine segment thickness after prior cesarean section to predict uterine rupture: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2019; 98(7):830-41. doi: 10.1111/aogs.13585.
doi: 10.1111/aogs.13585 |
| 10. |
Glavind J, Madsen LD, Uldbjerg N, et al. Cesarean section scar measurements in non-pregnant women using three-dimensional ultrasound: a repeatability study. Eur J Obstet Gynecol Reprod Biol 2016; 201:65-9. doi: 10.1016/j.ejogrb.2016.03.019.
doi: 10.1016/j.ejogrb.2016.03.019 pmid: 27064944 |
| 11. |
Uharček P, Brešťanský A, Ravinger J, et al. Sonographic assessment of lower uterine segment thickness at term in women with previous cesarean delivery. Arch Gynecol Obstet 2015; 292(3):609-12. doi: 10.1007/s00404-015-3687-0.
doi: 10.1007/s00404-015-3687-0 |
| 12. |
Ofili-Yebovi D, Ben-Nagi J, Sawyer E, et al. Deficient lower-segment cesarean section scars: prevalence and risk factors. Ultrasound Obstet Gynecol 2008; 31(1):72-7. doi: 10.1002/uog.5200.
doi: 10.1002/uog.5200 |
| 13. |
Yao M, Wang W, Zhou J, et al. Cesarean section scar diverticulum evaluation by saline contrast-enhanced magnetic resonance imaging: the relationship between variable parameters and longer menstrual bleeding. J Obstet Gynaecol Res 2017; 43(4):696-704. doi: 10.1111/jog.13255.
doi: 10.1111/jog.13255 |
| 14. |
Tang X, Wang J, Du Y, et al. Caesarean scar defect: risk factors and comparison of evaluation efficacy between transvaginal sonography and magnetic resonance imaging. Eur J Obstet Gynecol Reprod Biol 2019; 242:1-6. doi: 10.1016/j.ejogrb.2019.09.001.
doi: 10.1016/j.ejogrb.2019.09.001 |
| 15. |
Lim KK, Noe G, Hornsey E, et al. Clinical applications of 3D T2-weighted MRI in pelvic imaging. Abdom Imaging 2014; 39(5):1052-62. doi: 10.1007/s00261-014-0124-y.
doi: 10.1007/s00261-014-0124-y |
| 16. |
Polanec SH, Lazar M, Wengert GJ, et al. 3D T2-weighted imaging to shorten multiparametric prostate MRI protocols. Eur Radiol 2018; 28(4):1634-41. doi: 10.1007/s00330-017-5120-5.
doi: 10.1007/s00330-017-5120-5 |
| 17. |
Lv P, Dai Y, Lin J, et al. A comparison study between 3D T2-weighted SPACE and conventional 2D T2-weighted turbo spin echo in assessment of carotid plaque. Int J Cardiovasc Imaging 2017; 33(3):395-400. doi: 10.1007/s10554-016-1017-7.
doi: 10.1007/s10554-016-1017-7 |
| 18. |
Ucar M, Tokgoz N, Koc AM, et al. Assessment of 3D T2-weighted high-sampling-efficiency technique (SPACE) for detection of cerebellar tonsillar motion: new useful sign for Chiari I malformation. Clin Imaging 2015; 39(1):42-50. doi: 10.1016/j.clinimag.2014.08.011.
doi: 10.1016/j.clinimag.2014.08.011 |
| 19. |
Li P, Liu P, Chen C, et al. The 3D reconstructions of female pelvic autonomic nerves and their related organs based on MRI: a first step towards neuronavigation during nerve-sparing radical hysterectomy. Eur Radiol 2018; 28(11):4561-9. doi: 10.1007/s00330-018-5453-8.
doi: 10.1007/s00330-018-5453-8 |
| 20. |
Tsuboyama T, Takei O, Okada A, et al. Effect of uterine position and intrapelvic motions on the image quality of 3D T2-weighted MRI of the uterus: can short prescans predict the non-diagnostic image quality? Eur J Radiol 2020; 130: 109186. doi: 10.1016/j.ejrad.2020.109186.
doi: 10.1016/j.ejrad.2020.109186 |
| 21. |
Whittington JR, Slaton KB, Rhomberg ME, et al. Uterine dehiscence and subsequent pregnancy management: a review of the literature. Obstet Gynecol Surv 2021; 76(1):48-54. doi: 10.1097/OGX.0000000000000856.
doi: 10.1097/OGX.0000000000000856 pmid: 33506878 |
| 22. |
Asakura H, Nakai A, Ishikawa G, et al. Prediction of uterine dehiscence by measuring lower uterine segment thickness prior to the onset of labor: evaluation by transvaginal ultrasonography. J Nippon Med Sch 2000; 67(5):352-6. doi: 10.1272/jnms.67.352.
doi: 10.1272/jnms.67.352 pmid: 11031364 |
| 23. |
Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA 2006; 295(15):1809-23. doi: 10.1001/jama.295.15.1809.
doi: 10.1001/jama.295.15.1809 pmid: 16622143 |
| 24. |
Chen I, Jhangri GS, Lacasse M, et al. Relationship between interpregnancy interval and adverse perinatal and neonatal outcomes in Northern Alberta. J Obstet Gynaecol Can 2015; 37(7):598-605. doi: 10.1016/S1701-2163(15)30197-3.
doi: 10.1016/S1701-2163(15)30197-3 |
| 25. |
Wang CB, Chiu WW, Lee CY, et al. Cesarean scar defect: correlation between cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol 2009; 34(1):85-9. doi: 10.1002/uog.6405.
doi: 10.1002/uog.6405 pmid: 19565535 |
| [1] | Li Zifei, Liu Qingliang, Wang Xiaojun, Luan Jie. The Characteristics of Blood Supply and Tissue Hypoxia in Pathological Scars [J]. Chinese Medical Sciences Journal, 2017, 32(2): 113-118. |
| [2] | Ling Tong, Xian-jiang Wei. Meta-analysis of aspirin-heparin therapy for un-explained recurrent miscarriage [J]. Chinese Medical Sciences Journal, 2016, 31(4): 239-246. |
| [3] | Pan-xi Yu, Wen-qi Diao, Zuo-liang Qi, Jing-long Cai. Effect of Dermabrasion and ReCell® on Large Superficial Facial Scars Caused by Burn, Trauma and Acnes [J]. Chinese Medical Sciences Journal, 2016, 31(3): 173-179. |
| [4] | Min-hui Guo, Mei-fen Wang, Man-man Liu, Feng Qi, Fan Qu, Jian-hong Zhou. Management of Cesarean Scar Pregnancy: A Case Series [J]. Chinese Medical Sciences Journal, 2015, 30(4): 226-230. |
| [5] | Lin Zhu, Ang Zeng, Xiao-jun Wang, Yi-hong Jia, Zhi-fei Liu*. Perinipple Broken Line Incision: a Novel Approach for Breast Augmentation [J]. Chinese Medical Sciences Journal, 2015, 30(2): 76-79. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|