Chinese Medical Sciences Journal ›› 2022, Vol. 37 ›› Issue (3): 201-209.doi: 10.24920/004102
• Scientific Data Sharing and Reuse:Original Article • Previous Articles Next Articles
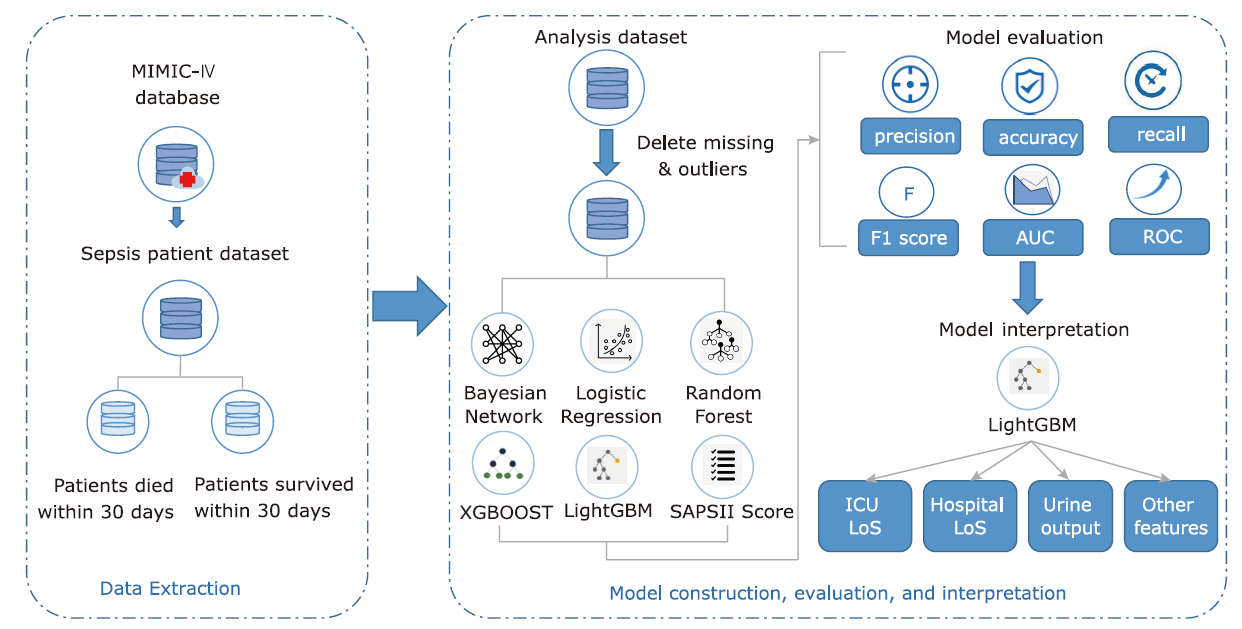
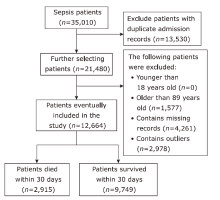
Comparison of Mortality Predictive Models of Sepsis Patients Based on Machine Learning
Ziyang Wang, Yushan Lan, Zidu Xu, Yaowen Gu, Jiao Li*( )
)
- Institute of Medical Information/Medical Library, Chinese Academy of Medical Science & Peking Union Medical College, Beijing 100020, China
-
Received:2022-04-21Accepted:2022-08-10Published:2022-09-30Online:2022-09-20 -
Contact:Jiao Li E-mail:li.jiao@imicams.ac.cn
Cite this article
Ziyang Wang, Yushan Lan, Zidu Xu, Yaowen Gu, Jiao Li. Comparison of Mortality Predictive Models of Sepsis Patients Based on Machine Learning[J].Chinese Medical Sciences Journal, 2022, 37(3): 201-209.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Figure 3.
Performance of models at different number of features. Three lines represent AUC scores in different models with top n features selected by MIC in (A), with different number of bins for continuous features discretization in (B). The color shadow area represents the fluctuation of AUC in different folds. The red dashed line represents the feature numbers we chose. LR: Logistic Regression; RF: Random Forest; BN: Bayesian Network."
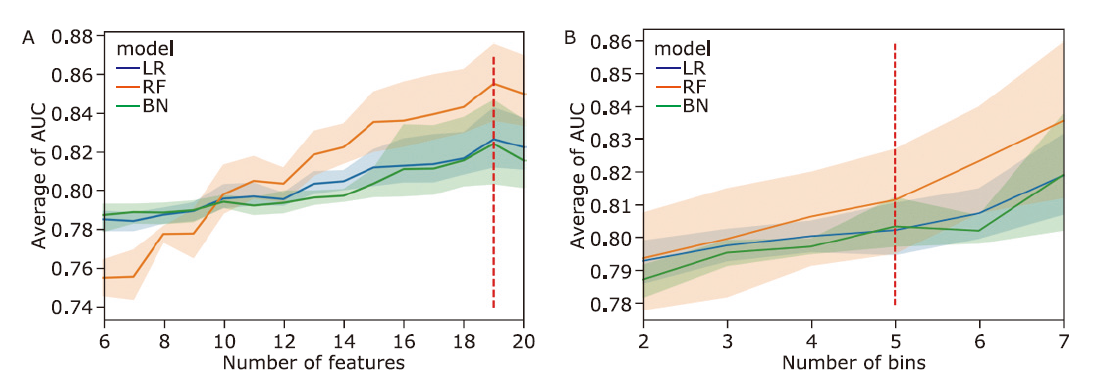
Table 2.
MIC values of the features in feature selection."
| NO | Feature | MIC |
|---|---|---|
| 1 | urine_max | 0.0441 |
| 2 | los_hospital | 0.0418 |
| 3 | aniongap_max | 0.0370 |
| 4 | specimen_count | 0.0347 |
| 5 | antibiotic_num | 0.0346 |
| 6 | bun_max | 0.0325 |
| 7 | bun_min | 0.0303 |
| 8 | aniongap_min | 0.0295 |
| 9 | bicarbonate_min | 0.0273 |
| 10 | inr_max | 0.0271 |
| 11 | creatinine_max | 0.0270 |
| 12 | vent_status | 0.0224 |
| 13 | los_ICU | 0.0223 |
| 14 | charlson_score_max | 0.0185 |
| 15 | bicarbonate_max | 0.0181 |
| 16 | chloride_max | 0.0180 |
| 17 | heart_rate_max | 0.0173 |
| 18 | sodium_max | 0.0160 |
| 19 | spo2_mean | 0.0158 |
Table 3.
Comparisons of features between survived and dead patients (n=12,664)"
| Features | All (n=12,664) | Survival (n=9,749) | Death (n=2,915) | t/χ2 | P value |
|---|---|---|---|---|---|
| aniongap_max (mmol/L, mean±SD) | 16.99 ± 5.37 | 19.43 ± 6.36 | 16.26 ± 4.81 | 24.85 | <0.001 |
| aniongap_min (mmol/L, mean±SD) | 13.12 ± 3.70 | 14.72 ± 4.47 | 12.64 ± 3.29 | 23.32 | <0.001 |
| antibiotic_num (mean±SD) | 6.31 ± 5.72 | 8.38 ± 6.00 | 5.69 ± 5.48 | 21.67 | <0.001 |
| bicarbonate_max (mmol/L, mean±SD) | 24.34 ± 4.71 | 23.39 ± 5.44 | 24.62 ± 4.43 | -11.14 | <0.001 |
| bicarbonate_min (mmol/L, mean±SD) | 21.15 ± 5.21 | 19.46 ± 6.04 | 21.65 ± 4.82 | -17.93 | <0.001 |
| bun_max (mg/L, mean±SD) | 32.40 ± 25.09 | 42.77 ± 29.93 | 29.30 ± 22.54 | 22.46 | <0.001 |
| bun_min (mg/L, mean±SD) | 26.98 ± 21.93 | 35.84 ± 26.48 | 24.33 ± 19.61 | 21.75 | <0.001 |
| charlson_score_max (mean±SD) | 6.59 ± 3.03 | 7.63 ± 2.94 | 6.28 ± 2.98 | 21.79 | <0.001 |
| creatinine_max (mmol/L, mean±SD) | 1.64 ± 1.49 | 2.03 ± 1.56 | 1.53 ± 1.45 | 15.45 | <0.001 |
| chloride_max (mmol/L, mean±SD) | 106.21 ± 6.73 | 106.4 ± 6.29 | 105.58 ± 7.98 | 14.26 | <0.001 |
| inr_max (mean±SD) | 1.73 ± 1.27 | 2.11 ± 1.62 | 1.61 ± 1.11 | 15.47 | <0.001 |
| los_hospital (days, mean±SD) | 13.03 ± 13.76 | 11.73 ± 15.19 | 13.42 ± 13.28 | -5.42 | <0.001 |
| los_ICU (days, mean±SD) | 6.16 ± 6.80 | 7.14 ± 5.79 | 5.87 ± 7.05 | 9.85 | <0.001 |
| heart_rate_max (bpm, mean±SD) | 107.82 ± 21.48 | 106.05 ± 20.48 | 113.73 ± 23.60 | -14.54 | <0.001 |
| spo2_mean (%, mean±SD) | 96.94 ± 2.25 | 97.09 ± 1.95 | 96.44 ± 2.99 | 14.49 | <0.001 |
| sodium_max (mmol/L, mean±SD) | 140.14 ± 5.36 | 140.32 ± 6.65 | 140.08 ± 4.91 | 1.81 | 0.0696 |
| specimen_count (mean±SD) | 6.11 ± 5.51 | 8.14 ± 5.81 | 5.51 ± 5.26 | 21.91 | <0.001 |
| urine_max (ml, mean±SD) | 1,751.39 ± 1,253.79 | 1,284.30 ± 1,234.80 | 1,891.05 ± 1,225.37 | -23.32 | <0.001 |
| vent_status [n(%)]* | 12,664 (100) | 9,749 (77) | 2,915 (23) | 503.11 | <0.001 |
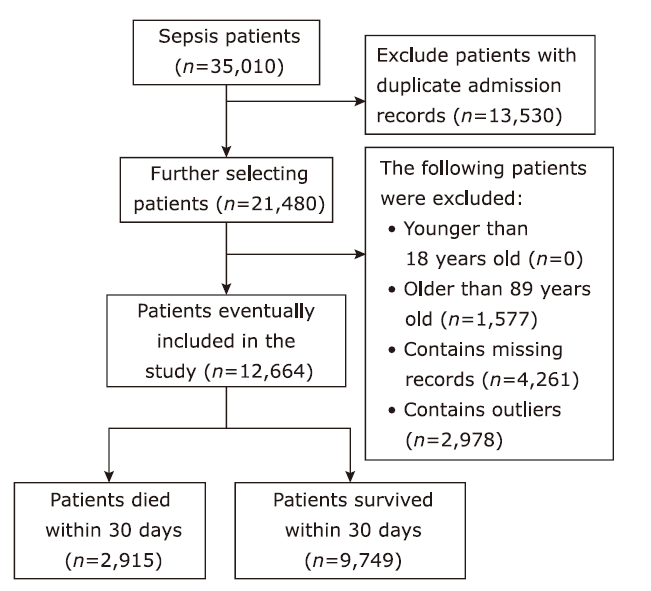
Table 4.
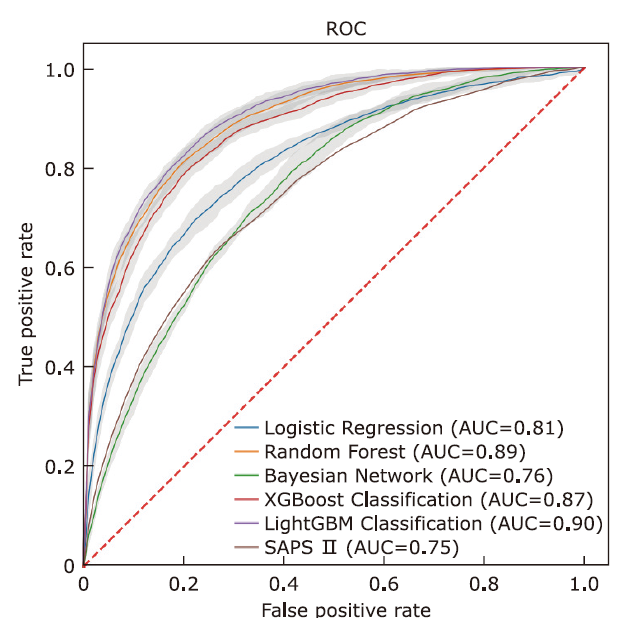
Performance comparison of five machine learning models and SAPS Ⅱ score predictor"
| Model | Accuracy | Precision | Recall | F1 Score | AUC |
|---|---|---|---|---|---|
| SAPS Ⅱ Score | 0.725 | 0.430 | 0.604 | 0.502 | 0.748 |
| Logistic Regression | 0.751(0.02)# | 0.486(0.03)# | 0.719(0.06)# | 0.571(0.02)# | 0.807(0.01)# |
| Bayesian Network | 0.654(0.03)# | 0.378(0.02)# | 0.773(0.06)* | 0.507(0.01)# | 0.756(0.01)# |
| Random Forest | 0.806(0.02)# | 0.558(0.04) | 0.807(0.05) | 0.657(0.01) | 0.891(0.01)* |
| XGBoost | 0.795(0.02) | 0.541(0.04) | 0.804(0.05) | 0.645(0.02)* | 0.875(0.01)# |
| LightGBM | 0.808(0.02) | 0.559(0.04) | 0.834(0.04) | 0.668(0.02) | 0.900(0.01) |
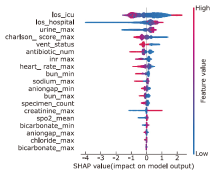
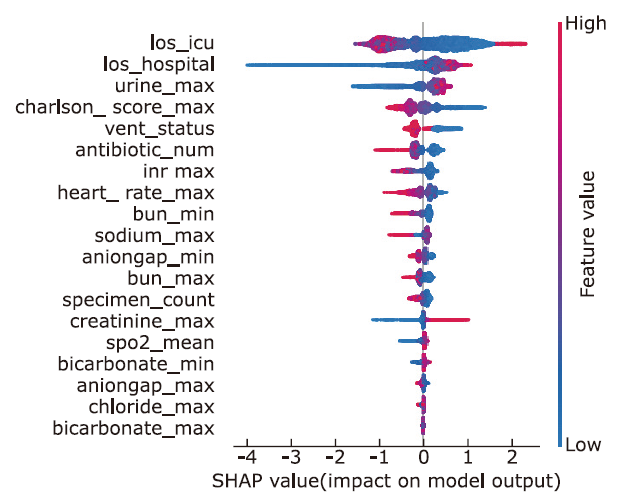
Figure 5.
Feature explanation of lightGBM model using the SHapley Addictive exPlanations (SHAP) value Each point in the figure is the SHAP value of a sample, and the color of the point represents the value of the feature. Red represents high values while blue represents low values. SHAP value greater than 0 indicates that the feature is a risk factor for death, while less than 0 indicates a protective factor."
| 1. |
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315(8):801-10. doi: 10.1001/jama.2016.0287.
doi: 10.1001/jama.2016.0287 pmid: 26903338 |
| 2. |
Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther 2012; 10(6):701-6. doi: 10.1586/eri.12.50.
doi: 10.1586/eri.12.50 pmid: 22734959 |
| 3. |
Song J, Park DW, Moon S, et al. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect Dis 2019; 19:68. doi: 10.1186/s12879-019-4618-7.
doi: 10.1186/s12879-019-4618-7 |
| 4. |
Xie J, Wang H, Kang Y, et al. The epidemiology of sepsis in Chinese ICUs: A national cross-sectional survey. Crit Care Med 2020; 48(3):e209-e218. doi: 10.1097/CCM.0000000000004155.
doi: 10.1097/CCM.0000000000004155 |
| 5. |
Zhao L, Zhao L, Wang YY, et al. Platelets as a prognostic marker for sepsis: a cohort study from the MIMIC-III database. Medicine 2020; 99(45):e23151. doi: 10.1097/MD.0000000000023151.
doi: 10.1097/MD.0000000000023151 |
| 6. |
Chen H, Zhu Z, Zhao C, et al. Central venous pressure measurement is associated with improved outcomes in septic patients: an analysis of the MIMIC-III database. Crit Care 2020; 24(1):433. doi: 10.1186/s13054-020-03109-9.
doi: 10.1186/s13054-020-03109-9 |
| 7. |
Zhu C, Xu Z, Gu Y, et al. Prediction of post-stroke urinary tract infection risk in immobile patients using machine learning: an observational cohort study. J Hosp Infect 2022; 122:96-107. doi: 10.1016/j.jhin.2022.01.002.
doi: 10.1016/j.jhin.2022.01.002 pmid: 35045341 |
| 8. |
Wang Y, Sun F, Hong G, et al. Thyroid hormone levels as a predictor marker predict the prognosis of patients with sepsis. Am J Emerg Med 2021; 45:42-7. doi: 10.1016/j.ajem.2021.02.014.
doi: 10.1016/j.ajem.2021.02.014 pmid: 33652253 |
| 9. |
Hou N, Li M, He L, et al. Predicting 30-days mortality for MIMIC-III patients with sepsis-3: a machine learning approach using XGboost. J Transl Med 2020; 18:462. doi: 10.1186/s12967-020-02620-5.
doi: 10.1186/s12967-020-02620-5 pmid: 33287854 |
| 10. |
Feng M, McSparron JI, Kien DT, et al. Transthoracic echocardiography and mortality in sepsis: analysis of the MIMIC-III database. Intens Care Med 2018; 44(6): 884-92. doi: 10.1007/s00134-018-5208-7.
doi: 10.1007/s00134-018-5208-7 |
| 11. |
Hou N, Li M, He L, et al. Predicting 30-days mortality for MIMIC-III patients with sepsis-3: a machine learning approach using XGboost. J Transl Med 2020; 18:462. doi: 10.1186/s12967-020-02620-5.
doi: 10.1186/s12967-020-02620-5 pmid: 33287854 |
| 12. |
Wang D, Li J, Sun Y, et al. A machine learning model for accurate prediction of sepsis in ICU patients. Front Public Health 2021; 9: 754348. doi: 10.3389/fpubh.2021.754348.
doi: 10.3389/fpubh.2021.754348 |
| 13. | Johnson A, Bulgarelli L, Pollard T, et al. MIMIC-IV (version 0.4). PhysioNet 2020. https://doi.org/10.13026/a3wn-hq05. |
| 14. |
Uusitalo L. Advantages and challenges of Bayesian networks in environmental modelling. Ecol Modell 2007; 203(3): 312-18. doi: 10.1016/j.ecolmodel.2006.11.033.
doi: 10.1016/j.ecolmodel.2006.11.033 |
| 15. |
Mihaljević B, Bielza C, Larrañaga P. Bayesian networks for interpretable machine learning and optimization. Neurocomputing 2021; 456:648-65. doi: 10.1016/j.neucom.2021.01.138.
doi: 10.1016/j.neucom.2021.01.138 |
| 16. |
Hanko M, Grendár M, Snopko P, et al. Random forest-based prediction of outcome and mortality in patients with traumatic brain injury undergoing primary decompressive craniectomy. World Neurosurg 2021; 148: e450-e458. doi: 10.1016/j.wneu.2021.01.002.
doi: 10.1016/j.wneu.2021.01.002 pmid: 33444843 |
| 17. |
Davagdorj K, Pham VH, Theera-Umpon N, et al. XGBoost-based framework for smoking-induced noncommunicable disease prediction. Int J Environment Res Public Health 2020; 17(18): e6513. doi: 10.3390/ijerph17186513.
doi: 10.3390/ijerph17186513 |
| 18. |
Zhang C, Lei X, Liu L. Predicting metabolite-disease associations based on lightgbm model. Front Genet 2021; 12: 660275. doi: 10.3389/fgene.2021.660275.
doi: 10.3389/fgene.2021.660275 |
| 19. |
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993; 270(24): 2957-63. doi: 10.1001/jama.270.24.2957.
doi: 10.1001/jama.270.24.2957 |
| 20. |
Moreno-Torres V, Royuela A, Múñez E, et al. Better prognostic ability of NEWS2, SOFA and SAPS-II in septic patients. Medicina Cinica 2021; 159(5):224-9. doi: 10.1016/j.medcli.2021.10.021.
doi: 10.1016/j.medcli.2021.10.021 |
| 21. |
Cohen J, Vincent JL, Adhikari NKJ, et al. Sepsis: a roadmap for future research. Lancet Infect Dis 2015 ;15(5): 581-614. doi: 10.1016/S1473-3099(15)70112-X.
doi: 10.1016/S1473-3099(15)70112-X |
| 22. | Zhang ZQ. Effect of changes in urine volume on prognosis of patients with sepsis and acute kidney injury after continuous renal replacement therapy. Chin Med Pharm 2021; 11(12): 178-82. |
| 23. | Lundberg S, Lee SI. A Unified Approach to Interpreting Model Predictions, carXiv: 1705.07874. Available from: http://doi.org/1048550/arXiv.1705.07874. |
| 24. |
Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: Guideline-based management. Cleveland Clin J Med 2020; 87(1): 53-64. doi: 10.3949/ccjm.87a.18143.
doi: 10.3949/ccjm.87a.18143 |
| 25. |
Vincent JL, Ferguson A, Pickkers P, et al. The clinical relevance of oliguria in the critically ill patient: analysis of a large observational database. Criti Care 2020; 24: 171. doi: 10.1186/s13054-020-02858-x.
doi: 10.1186/s13054-020-02858-x |
| [1] | Chen Xu, Huo Xiaofei, Wu Zhe, Lu Jingjing. Advances of Artificial Intelligence Application in Medical Imaging of Ovarian Cancers [J]. Chinese Medical Sciences Journal, 2021, 36(3): 196-203. |
| [2] | Jiazheng Li, Lei Tang. Radiomics in Antineoplastic Agents Development: Application and Challenge in Response Evaluation [J]. Chinese Medical Sciences Journal, 2021, 36(3): 187-195. |
| [3] | Junxiong Yin, Cheng Yu, Lixia Wei, Chuanyong Yu, Hongxing Liu, Mingyang Du, Feng Sun, Chongjun Wang, Xiaoshan Wang. Detection of Asymptomatic Carotid Artery Stenosis in High-Risk Individuals of Stroke Using a Machine-Learning Algorithm [J]. Chinese Medical Sciences Journal, 2020, 35(4): 297-305. |
| [4] | Guan Jian. Artificial Intelligence in Healthcare and Medicine: Promises, Ethical Challenges and Governance [J]. Chinese Medical Sciences Journal, 2019, 34(2): 76-83. |
| [5] | Zhang Hongmin, Wang Xiaoting, Zhang Qing, Liu Dawei. Resuscitation of Septic Patients with Target-and-endpoint Protocol: A Retrospective Study from a Chinese Tertiary Hospital ICU [J]. Chinese Medical Sciences Journal, 2018, 33(3): 135-142. |
| [6] | Jun Shen, Fa Sun, Fang-min Chen, Zhi-ping Wu, and Sheng-wen Li. Therapy and Prevention of Postoperative Urosepsis of Ureter Endoscopic Lithotripsy for “Non-infection” [J]. Chinese Medical Sciences Journal, 2016, 31(1): 49-53. |
| [7] | Gao Zeng, Jie Liu, Ning Wu, Cong-wei Jia, Shu-bin Guo. Lipopolysaccharide Challenge Induces Long Pentraxin 3 Expression in Mice Independently from Acute Lung Injury [J]. Chinese Medical Sciences Journal, 2015, 30(1): 7-17. |
| [8] | Gao Zeng, Cong-wei Jia, Jie Liu, Shu-bin Guo. Lipocalin-2 Test in Distinguishing Acute Lung Injury Cases from Septic Mice Without Acute Lung Injury [J]. Chinese Medical Sciences Journal, 2014, 29(2): 65-77. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|