NONARTERITIC anterior ischemic optic neuropathy (NAION) is one of the major causes of acute optic neuropathy in the elderly.1,2 Despite the wide consensus on the “ischemic” nature and the gross anatomical location of this disease as the name implies, the exact underlying hemodynamic mechanism within the optic nerve head (ONH) remain to be fully elucidated.
The ONH is vascularized by two major arterial systems:3 the superficial nerve fiber layer is mainly supplied by retinal arterioles; the deep major part of the ONH, subdivided into prelaminar, lamina and retrolaminar regions, are principally supplied by direct branches of the posterior ciliary arteries (PCAs). It has been suggested that it is the deep ONH regions, supplied by PCAs, that probably show more decrease in circulation4 and are involved in the pathogenetic changes in NAION.5-7 However, most current available techniques for blood flow measurement in NAION patients, such as Laser Doppler Flowmetry (LDF), laser speckle flowgraphy, can only measure the blood flow of superficial nerve fiber layer in NAION patients.3,8 LDF is one of the non-invasive techniques for assessment of volumetric blood flow.9 It has been widely used to measure the hemodynamics of cerebral vascular after stroke,10,11 and also in the measurement of blood flow in the optic nerve head12 and subfoveal choroid.13 Rodents are significant animal model in physiology and therapeutics, and similar LDF technique has been developed to measure the vascular bed of the rat eyes.14
A rat NAION (rNAION) model with similar funduscopic and pathological changes to those of human NAION was first established by Bernstein in 2003.15,16 The key event to generate this model is to induce photochemical thrombosis of the microvasculature in the ONH by direct irradiating the ONH with argon green laser after intravenous injection of Rose Bengal (RB), which results in ischemic ONH edema.17 With the rNAION model, some studies have observed the deeper ONH circulation alterations in vitro ONH tissues.15,18,19 The strength of these results, however, is limited by the “in vitro” nature of the experimental approaches. In addition, the microcirculation status of ONH was only measured at the very early phase (no more than 3 days) after disease induction, which only provided a snapshot of the dynamic process and may obscure the speed and duration of arterial blood flow reduction in ONH during disease progression.
In our previous studies, the structure and function changes have been longitudinally monitored.15,19 To shed new light on the characteristics of the hemodynamic changes in rNAION at different time points, dynamic changes in blood flow kinetics of the ONH were measured “in vivo”.
MATERIALS AND METHODS
Animals
All protocols were approved by the Experimental Animals Committee and were consistent with the Declaration of Helsinki or the NIH statement for the Use of Animals in Ophthalmic and Vision Research. Male pathogen-free Sprague-Dawley (SD) rats (weighing 200-220 g, kept at 20-22 °C) were used for this study. Each rat in this study underwent a complete ophthalmic examination to rule out ocular abnormalities.
Induction of rNAION
The experimental protocol for rNAION induction has been reported previously.15,19 In brief, 1 ml/kg Rose Bengal (RB) [2.5 mM in phosphate-buffered saline (PBS), 90% purity; Sigma-Aldrich, St. Louis, MO, USA] was injected via femoral vein and the right ONHs were immediately photo-activated using an argon-laser photo-coagulator (Ultima 2000 SE Argon, Coherent inc., Santa Clara, CA, USA) with the following parameters: wave length 532 nm; power 50 mW; laser spot size 500 um; duration 12 seconds. The posterior segments of the eyes were examined immediately after induction to rule out hemorrhage. For the laser group, the ONH of the right eyes were illuminated with the laser without intraperitoneal injection of RB; and vice versa for the RB group (only injected with RB via the femoral vein). The naive group received no intervention as the name indicates.
Fundus photography and fundus fluorescein angiography
Fundus photography and fundus fluorescein angiography (FFA) were performed after anesthetization and mydriasis using a slip lamp equipped with a camera (ASA 800, incandescent; Nikon, Tokyo, Japan) and Spectralis HRA+OCT (Heidelberg Engineering, Heidelberg, Germany), respectively. For FFA, angiographic images centered on the ONH were taken at intervals of approximately 1 second immediately after injection of fluorescein sodium for about 20 seconds, and continued at intervals of about 10 seconds for up to 5-9 minutes. Fundus photographs were taken in naive rats (n=2) and rNAION 3 h, 1 d, 5 d, 14 d and 90 d after disease induction (n=3 for each time point). FFAs were performed for naive rats (n=2) and rNAION (n=3) in 3 hours after disease induction. The early phase of FFA was defined as before 1.5 minutes after injection, and late phase was defined as over 3 minutes after injection.
Histologic preparation
Animals were euthanized after deep anesthetization, and the eyes were removed immediately and then fixed in 4% paraformaldehyde-phosphate-buffered saline (PF-PBS) for 1 h. Tissues were then embedded in paraffin, sectioned, and stained with hematoxylin-eosin (H&E) or toluidine blue for histologic examination. Histologic examinations were performed in naive rats (n=2), laser-only rats and RB-only rats (1 d after treatment, n=2 for each group), and rNAION rats 1 d and 90 d after disease induction (n=2 at each time point).
Laser doppler flowmetry
Longitudinal hemodynamic changes of posterior ONH were monitored with laser doppler flowmetry(LDF) device (moorVMS-LDF2, Moor Instruments Ltd., UK) on day 3, day 7, day 14, day 21 and day 40 after disease induction in rNAION rats (n=3 at each time point) and in naive rats. The surface laser Doppler probe (VP3.0, Moor Instruments Ltd., UK), with a tip diameter of 0.50 mm, operated at the wavelength of 785 nm. As previously described,20 the optic nerve of rat was exposed through a lateral canthus incision. The LDF probe was placed perpendicular to the surface of the optic nerve and as close as possible to the eyeball. The volume of LDF measurement was approximately 1 mm3. The ONH blood flow kinetics, measured in perfusion units (PU) on a real-time basis, was monitored for about 3 minutes till the readout reached steady state. PU is the basic index of LDF measurement and is the Doppler shift value produced by RBC flowing. It is a relative unit to measure the microcirculatory blood flow in local deep tissue and the change of PU value directly shows the changes of microcirculatory blood flow of tissue.
Statistical analysis
All data were reported as mean ± SD. Statistical analysis was performed using SAS (version 9.3, SAS Institute Inc, Cary, NC) to evaluate longitudinal changes in ONH blood perfusion over time. Statistical differences were evaluated by one-way ANOVA, Student’s t-test and Bonferroni adjustment for multiple comparisons. A two-sided P value less than 0.05 was considered statistically significant.
RESULTS
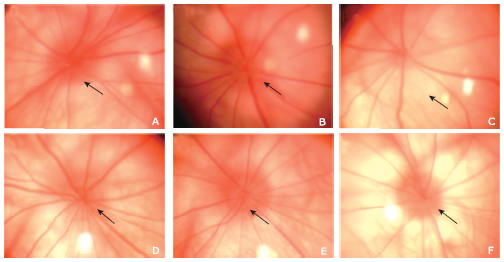
Fundus photography and FFA of rNAION
Fundus photography (Fig. 1) showed that, in contrast to fundus of naive eyes, the edema of ONH in the rNAION eyes was observed at 3 hour after disease induction and reached maximum on day 1 after disease induction. On day 5, profound resolution of ONH edema was observed in the rNAION eyes, and the appearance of ONH returned to normal on day 14; on day 90, however, the ONH appeared to be pale and reduction in size.
Figure 1.
Fundus photographs of optic nerve head (ONH) in naive rats and rNAION rats. A. The border of the ONH in a naive rat eye was distinct (arrow); B. in rNAION rats, blurring of the ONH border (arrow) observed 3 hours after disease induction, indicating edema; C. diameter of the ONH enlarged and reached the maximum (arrow) 1 day after disease induction; D. five days after induction, edema of the ONH resolved almost completely; E. the appearance of the ONH returned to normal on day 14; F. the ONH was apparently pale with reduction in size on day 90. rNAION: rat model of nonarteritic anterior ischemic optic neuropathy; ONH: optic nerve head.
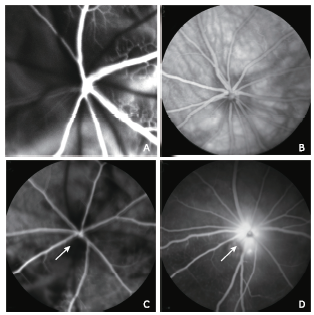
FFA (Fig. 2) revealed the normal fluorescein perfusion of the choroidal and retinal vasculature in the early phase and normal fluorescein distribution of fundus in the late phase in naive rats (n=2). In rNAION rats 3 hours after disease induction, however, filling defects in the choroid and ONH were observed in the early phase, and marked dye leakage from the ONH was present in the late phase.
Figure 2.
Representative FFA images of a naive eye and an rNAION eye 3 hours after disease induction. A. normal fluorescein perfusion of the choroidal and retinal vasculature in the early phase of FFA in a naive eye. B. normal fluorescein distribution in the fundus in the late phase of FFA in a naive eye; C. FFA imaging 3 seconds after injection (early phase) of an rNAION eye showed filling defects in the choroid and the ONH (arrow); D. late phase imaging of the same eye showed marked dye leakage (arrow) from the ONH. FFA: fundus fluorescein angiography.
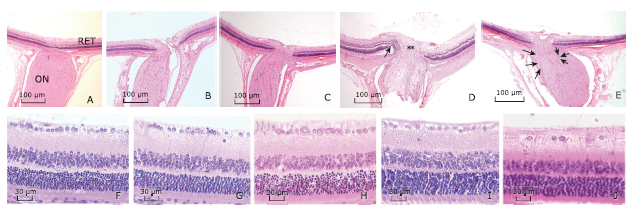
Histopathology
As compared with naive eyes, no abnormal changes were observed in the retina and ONH in the laser-only rats 1 day after laser treatment and RB-only rats 1 day after RB injection. In the rNAION rats, however, obvious ONH edema, usually associated with peripapillary retinal detachment, was observed on the day 1 after disease induction; and on the day 90, a reduction in number of retinal ganglion cell (RGC) axons, as well as tissue fibrosis and cellular infiltration were observed, while cell densities of inner nuclear layer (INL) and outer
nuclear layer (ONL) remained unchanged (Fig. 3).
Figure 3.
Representative histologic sections of ONH and retina in naive and rNAION eyes (H&E stain). A. longitudinal sections of the ONH in naive eyes, B. in the laser-only eyes and C. in the RB-only eyes showed normal histology and anatomy of the optic nerve and peripapillary retina. D. On day 1 after rNAION induction, the ONH was edematous with thickened nerve fiber bundles (double asterisks) and peripapillary retinal detachment (arrow). E. On day 90 after induction, there was a reduced number of RGC axons (long arrow) accompanied by gliosis and cellular infiltration (short arrow). F. naive eyes, G. laser-only eyes, H. RB-only eyes, and I. eyes 1 day after rNAION induction. The RGCs in peripapillary retina were closely packed in a single layer with normal density. J. On day 90 after rNAION induction, there was an obvious reduction in density of the RGCs in retina, while the cell densities in the INL and ONL remained mainly unchanged. (magnifying power: A-E, 50×; F-J, 200×). RB: rose bengal; RGC: retinal ganglion cell; INL: inner nuclear layer; ONL: outer nuclear layer.
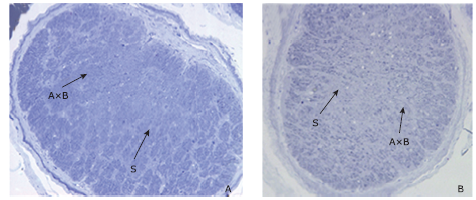
Myelinated axon bundles of retinal ganglion cells (RGCs) were tightly packed and surrounded by thin pial septate in the optic nerve (ON) in naive rat eyes. On the day 90 after rNAION induction, however, there was a marked loss of central axons with increased septal thickness and shrinkage of the axonal bundles (Fig. 4).
Figure 4.
Representative cross sections of ON in naive and rNAION eyes (Toluidine blue stain, 200×). A. cross section of ON in naive eye showed tightly packed axonal bundles by the pial septate (S); B. cross section of ON on day 90 after rNAION induction, an apparent reduction in central axonal bundle density with increased septal thickness was observed. AxB: axonal bundle. ON: optic nerve.
Longitudinal measurement in hemodynamic changes of posterior ONH blood flow in rNAION
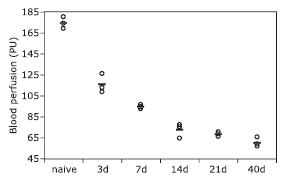
The mean blood flow kinetics of naive eyes was 174.73 ±5.34 PU (n=3), and the mean blood flow of rNAION eyes on day 3, 7, 14, 21 and 40 after NAION modeling were 116.12±8.93 PU (n=3), 94.89±1.83 PU (n=3), 73.02±6.99 PU (n=3), 68.94±2.24 PU (n=3) and 60.92±4.58 PU (n=3) respectively, where a significant difference was noticed (F=175.06, P<0.0001) with a rapid and pronounced drop of blood perfusion in posterior ONH observed (Fig. 5). The reduction in blood perfusion was statistically significant at each time point after disease induction as compared with that in naive rats (all P<0.0001). The blood perfusion significantly decreased compared with that in naive rats, with a 33.55%, 45.69% and 58.21% reduction on day 3, day 7 and day 14, respectively. The differences were significant between the data of day 3 and day 7 (t=4.66, P=0.008), day 7 and day 14 (t=4.81, P=0.006), day 3 and day 14 (t=9.47, P<0.0001). No significant differences demonstrated between neither day 14 and day 21 (t=0.90, P=1.00), nor day 21 and day 40 (t=1.76, P=1.00).
Figure 5.
The hemodynamic changes in blood flow kinetics of posterior ONH in naive rats and rNAION rats at different time points after disease induction. The posterior ONH blood perfusion measurements in rNAION rats were significantly lower than that in naive rats (all P<0.0001). Statistically significant reductions of optic nerve blood flow were detected between day 3 and day 7, day 7 and day 14 after disease induction (both P<0.01).
DISCUSSION
Nowadays, plenty of experimental researches using rNAION have been conducted to investigate cellular inflammation,21 oligodendrocyte death22 and neuroprotective effects of drugs.23,24 The blood flow of ONH has been observed in vitro in rNAION. Bernstein15 used intra-cardiac perfusion of India ink and found a severe reduction in the filling of ONH capillaries 30 minutes after induction. Chuman et al. also found the reduction of capillary perfusion in the ONH 3 days after induction by using the same method.19 However, Nicholson et al. used perfusion of fluorescent marker (FITC-BSA) and showed a quite different kinetic of microcirculation impairment in the posterior segment of ONH with detectable but minimal loss of capillary perfusion 4 hours after disease induction and a much more significant loss of perfusion 1 day after induction.18 It is worth noting that in these studies, microcirculation status of the ONH was only measured at the very early time after disease induction.
In this study, we produced the rNAION following the method of Bernstein.9 Optic disc edema appeared as a hallmark in the early phase of disease and the FFA revealed early hypofluorescence followed by late hyperfluorescence in the optic disc. Histopathological study showed tissue edema followed by loss of axonal bundles, thickening of septa and gliosis in the optic nerve. These results demonstrated that there was a selective damage to capillaries in ONH, followed by ONH edema, and finally optic atrophy with loss of RGC. Therefore, we believed that the rNAION in our study was successfully established as Bernstein did.
Then, we longitudinally measured the dynamics of blood flow kinetic changes in ONH of rNAION by placing LDF probe directly 1 mm anterior to the optic nerve (the posterior ONH), where the most prominent degenerative changes were detected histologically.25Interestingly, in rNAION, the ONH blood perfusion did not reduce uniformly in depth. A sharp reduction of blood perfusion was found in 14 days after the disease induction, while in the longitudinal observation of the posterior ONH blood flow, the blood perfusion remained low steadily afterwards, indicating that the ischemic status was then stable. The underlying mechanism may lie in that in the early time, the capillary is blocked by fibrin, capillary leakage and extracellular edema result in intracellular edema and/or capillary compassion,18 while in the late time, the impaired blood flow autoregu-lated25,26 after photochemical thrombosis of microvasculature in the ONH.
In rNAION, we found that as the progress of the disease, even when the edema of the ONH had resolved, the density of RGCs still reduced. Our finding was consistent with the report in 2016.27 The coupling association between blood flow and neural activity in neural tissues has been demonstrated in literatures.28 Relationship had been also found between ischemic status and deteriorated visual function, damaged structure and other morphometric changes.29,30 Thus we hypothesized that the reduced blood flow might be the reflection of the reduced metabolic demand associated with neuronal loss and connective tissue changes.
Despite we firstly observed in vivo the dynamic feature of posterior ONH blood flow in rNAION in this study, limitations of this study should be addressed. Firstly, the approach used to measure the posterior ONH blood flow was invasive and the surgical exposure of the posterior ONH was of high skilled operation. Secondly, we did not measure RGCs density of the retina which might be associated with the blood flow of posterior ONH, thus we were not able to provide a quantitative assessment of the neurodegeneration. Thirdly, functional evaluations of the ON, e.g. visual evoked potential, were not carried out in this study. These limitations should be kept in mind when interpreting the data and should be taken into consideration for studies in future.
In summary, we successfully established rNAION. With this model, our study characterized the in vivo dynamic feature of posterior ONH blood perfusion reduction at different time points. Our findings, to some extent, provide a reference for understanding the hemodynamic changes occurred in rNAION. Further studies on ameliorating the early blood flow with rNAION will provide valuable information on the therapeutic approaches.
Conflict of interest statement
All authors declared no conflict of interests.
参考文献
Incidence of nonarteritic and arteritic anterior ischemic optic neuropathy. Population-based study in the state of Missouri and Los Angeles County, California
Abstract This population-based study was undertaken to obtain information on age-, sex-, and race-specific incidence of nonarteritic and arteritic anterior ischemic optic neuropathy for the State of Missouri and for Los Angeles County, California. Among subjects who were 50 or older the estimated mean annual incidence rates per 100,000 population were 2.30 for nonarteritic anterior ischemic optic neuropathy and 0.36 for arteritic anterior ischemic optic neuropathy. White individuals appear to be at significantly higher risk of developing nonarteritic anterior ischemic optic neuropathy than black or Hispanic individuals, suggesting possible genetic predisposition.
Incidence of nonarteritic anterior ischemic optic neuropathy
. PURPOSE : Nonarteritic anterior ischemic optic neuropathy is the most common acute optic nerve disease of adults over age 50 years. This study determined the incidence of acute nonarteritic anterior ischemic optic neuropathy in the circumscribed population of Olmsted County, Minnesota. . METHODS : This was a retrospective study of the incidence of acute nonarteritic anterior ischemic optic neuropathy between 1981 and 1990. The Rochester Epidemiology Project medical records linkage system facilitates identification of the medical records of virtually all Olmsted County residents with a given diagnosis. All cases of acute nonarteritic anterior ischemic optic neuropathy that fulfilled certain inclusion and exclusion criteria were identified. . RESULTS : Twenty-two cases in 21 patients (11 men and 10 women) were recorded. The crude annual incidence rate was 10.3 per 100,000 individuals (95% confidence interval [CI] = 5.1 to 18.4). When adjusted to the age and sex distribution of the 1990 United States white population, the incidence rate was 10.2 per 100,000 (95% CI = 6.5 to 15.6). At diagnosis, the median age was 72 years, mean visual acuity was 20/200 in the affected eye, and the most common visual field defect was an altitudinal deficit (10 cases). . CONCLUSIONS : Although results of this small study should be interpreted cautiously, extrapolation of our findings to the United States white population indicates that nearly 5,700 new cases of acute nonarteritic anterior ischemic optic neuropathy may be expected to occur each year in this group.
Ocular blood flow assessment using continuous laser Doppler flowmetry
.This article describes the technique of continuous laser Doppler flowmetry (LDF) as applied to the measurement of the flux of red blood cells in the optic nerve head, iris and subfoveal choroid. Starting with the exposition of the physical principles underlying LDF, we first describe the various devices developed to perform LDF in these vascular beds. We then discuss the clinical protocols, blood flow parameters, calibration procedures, reproducibility and limitations of the LDF technique. Various problems still need to be solved in order to bring to light the full potential of LDF in the assessment of microcirculatory haemodynamics.
Retrobulbar haemodynamics in non-arteritic anterior ischaemic optic neuropathy
In this issue of the journal, Kaup et al (see p 1350) report results relating to blood flow dynamics in the ophthalmic artery, the nasal and temporal short posterior ciliary arteries and the central retinal artery in patients in the acute stage of non-arteritic anterior ischaemic optic neuropathy (NAION). Although they are not the first group to conduct such a study, they are the first to compare their findings in patients with NAION with those measured in a group of age-matched controls.
Ischemic optic neuropathy
Neuron stress and loss following rodent anterior ischemic optic neuropathy in double-reporter transgenic mice
PURPOSE: (NAION) is an optic nerve involving of retinal ganglion (RGC) neurons. The rodent NAION model (rAION) can use transgenic strains to reveal unique characteristics about the effects of sudden on RGCs and their . The impact of rAION on RGC stress patterns, RGC loss, and their after axonal were evaluated.: A double-transgenic strain was used, containing a construct with cyan fluorescent () under promoter control, and a construct with () linked to the stress gene c-promoter. in the is expressed predominantly in RGCs, enabling stereologic analysis of (+) RGC numbers and loss post-rAION-using confocal microscopy. RGC loss was correlated with axonal counts using transmission microscopy (TEM). immunohistochemistry was used to evaluate retinal stress after rAION.: The 45,000 CFP(+) in the RGC layer of control compared with previous RGC quantitative estimates. rAION produced RGC stress, defined as expression, in patterns corresponding with later RGC loss. rAION-associated RGC loss correlated with regional nerve fiber layer loss. Axonal loss correlates with stereologically determined RGC loss estimates in retinas.: Post-ON RGC stress patterns correlate with regional RGC loss. Cellular levels in most RGCs are low, suggesting rAION-affected RGCs express c-only transiently. (+) loss correlates closely with quantitative axonal loss, suggesting that the () transgenic strain is appropriate for RGC stereologic analyses.
Evaluation of inner retinal thickness around the optic disc using optical coherence tomography of a rodent model of nonarteritic ischemic optic neuropathy
Laser speckle flowgraphy for differentiating between nonarteritic ische-mic optic neuropathy and anterior optic neuritis
The aim of this study was to investigate the usefulness of laser speckle flowgraphy (LSFG) for the differentiation of acute nonarteritic ischemic optic neuropathy (NAION) from anterior optic neuritis (ON).To investigate blood flow in the optic disc under normal conditions, NAION, and anterior ON, we compared the tissue blood flow of the right eye with that of the left eye in the control group, and that of the affected eye with that of the unaffected eye in the NAION and anterior ON groups.In the normal control group, the tissue blood flow did not significantly differ between the right and left eyes. In the NAION group, all 6 patients had decreased optic disc blood flow in the NAION eye when compared with the unaffected eye. By contrast, in the anterior ON group, all 6 patients had increased optic disc blood flow in the anterior ON eye when compared with the unaffected eye. In the NAION group, the mean blur rate (MBR) of the affected eyes was 29.5 % lower than that of the unaffected eyes. In the anterior ON group, the MBR of the affected eyes was 15.9 % higher than that of the unaffected eyes.LSFG could be useful in differentiating between NAION and anterior ON. In addition, this imaging technique saves time and is noninvasive.
Assessment of flow dynamics in retinal and choroidal microcirculation
Alterations in ocular blood flow have been implicated in mechanisms that lead to vision loss in patients with various ocular disorders such as diabetic retinopathy, glaucoma, and age-related macular degeneration. Assessment of retinal and choroidal blood flow is also a window to evaluate systemic diseases that affect microvasculature. Quantification and qualification of the blood flow in the retina and choroid help us understand pathophysiology, stratify disease risk, and monitor disease progression in these disorders. Multiple methods are employed by researchers for assessment of blood flow, but a gold standard is lacking. We review commonly used methods, both invasive and non-invasive, for evaluation of blood flow including intravital microscopy, laser Doppler velocimetry, laser Doppler flowmetry, laser interferometry, confocal scanning laser Doppler flowmetry, laser speckle flowgraphy, Doppler optical coherence tomography, blue-field entoptic simulation, retinal vessel calibre assessment, optical coherence tomography angiography, retinal function imaging, color Doppler imaging, and scanning laser ophthalmoscope angiogram. As technology evolves, better evaluation of blood flow in various ocular and systemic diseases will likely bring new perspectives into clinical practice and translate to better diagnosis and treatment.
Complexity analysis of beat-to-beat skin-surface laser-doppler flowmetry signals in stroke patients
Abstract Objectives This study performed skin-surface LDF measurements and SampEn analysis with the aims of (i) capturing the temporal complexity of cerebral hemodynamics in stroke patients and (ii) discriminating stroke patients from healthy control subjects. We also investigated the response induced by AS in beat-to-beat SampEn indexes of LDF signals. Methods LDF signals were obtained at bilateral TaiYang acupoints in 52 stroke patients. Each assessment involved a 20-minute baseline recording, a 20-minute AS, and a subsequent 20-minute recording. The FDT, FRT, and PW were calculated for each pulse of the LDF signals, and then their SampEn values were calculated. Results The SampEn values of FRT were significantly larger in the stroke group (1.06402±020.052 and p02 = 02 0.013 at the stroke side; 1.05902±020.055 and p02 = 02 0.017 at the controlateral side) than in the control group (0.97502±020.120). On the stroke side, the SampEn of value of FRT was significantly decreased following AS (1.06402±020.052 to 1.00802±020.060; p02 = 02 0.027). Conclusion Larger SampEn values of FRT can be partly attributed to the local regulatory activities that are present in the stroke subjects when facing the induced abnormal vascular conditions and blood flow perfusion resistance. The present findings could aid the development of a noninvasive monitoring technique that will enable discrimination of the different microcirculatory responses in stroke patients.
Bifurcation in blood oscillatory rhythms for patients with ischemic stroke: a small scale clinical trial using laser doppler flowmetry and computational modeling of vasomotion
We describe application of spectral analysis of laser Doppler flowmetry (LDF) signals to investigation of cerebrovascular haemodynamics in patients with post-acute ischemic stroke (AIS) and cerebrovascular insufficiency. LDF was performed from 3 to 7 days after the onset of AIS on forehead in the right and left supraorbital regions in patients. Analysis of LDF signals showed that perfusion in the microvasculature in AIS patients was lower than that in patients with cerebrovascular insufficiency. As a result of wavelet analysis of the LDF signals we obtained activation of the vasomotion in the frequency range of myogenic oscillation of 0.1 Hz and predominantly nutritive regime microcirculation after systemic thrombolytic therapy of the AIS patients. In case of significant stroke size, myogenic activity, and nutritive pattern microhaemodynamics were reduced, in some cases non-nutritive pattern and/or venular stasis was revealed. Wavelet analysis of the LDF signals also showed asymmetry in wavelet spectra of the LDF signals obtained in stroke-affected and unaffected hemispheres in the AIS patients. A mechanism underlying the observed asymmetry was analyzed by computational modeling of vasomotion developed in Arciero and Secomb (2012). We applied this model to describe relaxation oscillation of arteriole diameter which is forced by myogenic oscillation induced by synchronous calcium oscillation in vascular smooth muscle cells. Calculation showed that vasomotion frequency spectrum at the low-frequency range (0.01 Hz) is reciprocally modulated by myogenic oscillation (0.1 Hz) that correlates with experimental observation of inter-hemispheric variation in the LDF spectrum.
Schlieren laser Doppler flowmeter for the human optical nerve head with the flicker stimuli
We describe a device to measure blood perfusion for the human optic nerve head (ONH) based on laser Doppler flowmetry (LDF) with a flicker stimuli of the fovea region. This device is self-aligned for LDF measurements and includes near-infrared pupil observation, green illumination, and observation of the ONH. The optical system of the flowmeter is based on a Schlieren arrangement which collects only photons that encounter multiple scattering and are back-scattered out of the illumination point. LDF measurements are based on heterodyne detection of Doppler shifted back-scattered light. We also describe an automated analysis of the LDF signals which rejects artifacts and false signals such as blinks. By using a Doppler simulator consisting of a lens and a rotating diffusing wheel, we demonstrate that velocity and flow vary linearly with the speed of the wheel. A cohort of 12 healthy subjects demonstrated that flicker stimulation induces an increase of 17.8% of blood flow in the ONH. (C) 2013 Society of Photo-Optical Instrumentation Engineers (SPIE)
Hypoxic, hypercapnic, and hyperoxic responses of the optic nerve head and subfoveal choroid blood flow in healthy humans
Abstract Purpose: To investigate the impact of different gas mixtures (hyperoxia, hypoxia, and hypercapnia) on the optic nerve head (ONH) and choroidal (Ch) hemodynamics. Methods: Twenty-three healthy subjects (28 00± 6 years) took part in the study. Variations in inspired oxygen and carbon dioxide fraction were produced by a gas mixing device. Arterial oxygen saturation (SpO2) was measured continuously using a transcutaneous sensor and end-tidal carbon dioxide partial pressure by capnography. The experiment comprised three successive periods: 3-minute baseline (room air breathing), 15-minute gas mixture inhalation (normocapnic hypoxia, hypercapnia, or hyperoxia), and 15-minute recovery (room air breathing). Laser Doppler flowmeter parameters-velocity (VEL), volume (VOL), and flow (BF) of red blood cells-were measured. Two-way ANOVAs were performed for statistical analysis. Results: In response to hyperoxia, ONHBF significantly decreased by -18% 00± 6% (P = 0.04) from baseline, due to significant changes in VEL (-12% 00± 3% P = 0.0002). During hypoxia at 85% SpO2, ONH VEL increased by +12% 00± 3% (P = 0.0009), whereas VOL and BF did not change significantly. ChBF significantly increased by +7% 00± 2% (P = 0.004) in response to hypoxia, due to significant changes in VEL +5% 00± 2% (P = 0.03). Both Ch and ONHBFs did not vary significantly in response to hypercapnia. Conclusions: The magnitude of the blood flow response is the most significant during hyperoxia for ONH and hypoxia for ChBF. For ONHBF, a 37% difference between hyperoxia and hypoxia can be useful when vasoreactivity to O2 will be tested in patients.
Compact laser doppler flowmeter (LDF) fundus camera for the assessment of retinal blood perfusion in small animals
Noninvasive techniques for ocular blood perfusion assessment are of crucial importance for exploring microvascular alterations related to systemic and ocular diseases. However, few techniques adapted to rodents are available and most are invasive or not specifically focused on the optic nerve head (ONH), choroid or retinal circulation. Here we present the results obtained with a new rodent-adapted compact fundus camera based on laser Doppler flowmetry (LDF). A confocal miniature flowmeter was fixed to a specially designed 3D rotating mechanical arm and adjusted on a rodent stereotaxic table in order to accurately point the laser beam at the retinal region of interest. The linearity of the LDF measurements was assessed using a rotating Teflon wheel and a flow of microspheres in a glass capillary. In vivo reproducibility was assessed in Wistar rats with repeated measurements (inter-session and inter-day) of retinal arteries and ONH blood velocity in six and ten rats, respectively. These parameters were also recorded during an acute intraocular pressure increase to 150 mmHg and after heart arrest (n = 5 rats). The perfusion measurements showed perfect linearity between LDF velocity and Teflon wheel or microsphere speed. Intraclass correlation coefficients for retinal arteries and ONH velocity (0.82 and 0.86, respectively) indicated strong inter-session repeatability and stability. Inter-day reproducibility was good (0.79 and 0.7, respectively). Upon ocular blood flow cessation, the retinal artery velocity signal substantially decreased, whereas the ONH signal did not significantly vary, suggesting that it could mostly be attributed to tissue light scattering. We have demonstrated that, while not adapted for ONH blood perfusion assessment, this device allows pertinent, stable and repeatable measurements of retinal blood perfusion in rats.
Functional and cellular responses in a novel rodent model of anterior ischemic optic neuropathy
Abstract PURPOSE: Anterior ischemic optic neuropathy (AION) is caused by sudden loss of vascular supply to retinal ganglion cell (RGC) axons in the anterior portion of the optic nerve and is a major cause of optic nerve dysfunction. There has been no easily obtainable animal model of this disorder. The current study was conducted to design a novel model of rodent AION (rAION), to enable more detailed study of this disease. METHODS: A novel rodent photoembolic stroke model was developed that is directly analogous to human AION. Using histologic, electrophysiological, molecular- and cell biological methods, the early changes associated with isolated RGC axonal ischemia were characterized. RESULTS: Functional (electrophysiological) changes occurred in RGCs within 1 day after rAION, with a loss of visual evoked potential (VEP) amplitude that persisted in the long term. The retinal gene expression pattern rapidly changed after rAION induction, with an early (<1 day) initial induction of c-Fos mRNA, and loss of RGC-specific gene expression. RGC-specific protein expression declined 2 days after detectable mRNA level changes, and immunostaining suggested that multiple retinal layers react to isolated RGC axonal ischemia. CONCLUSIONS: rAION rapidly results in electrophysiological and histologic changes similar to clinical AION, with reactive responses in primary and supporting neuronal cell layers. The rAION model can enable a detailed analysis of the individual retinal and optic nerve changes that occur after optic nerve stroke, which may be useful in determining possible therapeutic interventions for this disorder.
The rodent model of nonarteritic anterior ischemic optic neuropathy (rNAION)
Nonarteritic anterior ischemic optic neuropathy (NAION) is a focal ischemic lesion of the optic nerve that affects 1/700 individuals throughout their lifetime. NAION results in optic nerve edema, selective loss of the retinal ganglion cell neurons (RGCs) and atrophy of the optic nerve. A rodent model of NAION that expresses most NAION features and sequelae has been developed, which is applicable to both rats and mice. This model utilizes a focal laser application of 532 nm wavelength to illuminate a photoactive dye, Rose Bengal (RB), to cause capillary damage and leakage at the targeted anterior optic nerve (the laminar region). After rNAION induction, there is an early optic nerve ischemia, optic nerve edema, and intraneural inflammation, followed by selective RGC and axonal loss. Since the optic nerve is a CNS white matter tract, the rNAION model is applicable to mechanistic studies of selective white matter ischemia, as well as neuroprotective analyses and short and long-term mechanisms of glial and neuronal response to ischemia.
Establishing an experimental model of photodynamically induced anterior ischemic optic neuropathy
Numerous methods and drugs have been used to treat anterior ischemic optic neuropathy (AION); however, further investigations to determine the value of treatments for AION have been impeded by the lack of appropriate animal models of AION, significantly impacting on in-depth study of the disease. A rat model of AION was established, and corresponding functional changes of the fundus were observed using fundus fluorescein angiography (FFA), optical coherence tomography (OCT), and flash visual-evoked potential (F-VEP) in order to confirm the reliability of the AION model histopathologically. One day after model establishment, histopathology demonstrated that portions of the optic disc were highly edematous, with edema of nerve fibers and loose tissue, accompanied by displacement of the surrounding retina. At 23 days, the optic disc and surrounding nerve fiber layers had become thinner. None of the above-mentioned changes was observed in the laser, hematoporphyrin derivative (HPD), or naive groups. The results of fundus, FFA, F-VEP, and OCT ithin 90 days after model establishment onfirmed that krypton red laser irradiation (647 nm), applied 2 h after HPD injection, can establish an ideal animal model of AION.
PGJ(2) provides prolonged CNS stroke protection by reducing white matter edema
Abstract Few clinically effective approaches reduce CNS-white matter injury. After early in-vivo white matter infarct, NFB-driven pro-inflammatory signals can amplify a relatively small amount of vascular damage, resulting in progressive endothelial dysfunction to create a severe ischemic lesion. This process can be minimized by 15-deoxy-(12,14)-prostaglandin J2 (PGJ(2)), an analog of the metabolically active PGD(2) metabolite. We evaluated PGJ(2)'s effects and mechanisms using rodent anterior ischemic optic neuropathy (rAION); an in vivo white matter ischemia model. PGJ(2) administration systemically administered either acutely or 5 hours post-insult results in significant neuroprotection, with stereologic evaluation showing improved neuronal survival 30 days post-infarct. Quantitative capillary vascular analysis reveals that PGJ(2) improves perfusion at 1 day post-infarct by reducing tissue edema. Our results suggest that PGJ(2) acts by reducing NFB signaling through preventing p65 nuclear localization and inhibiting inflammatory gene expression. Importantly, PGJ(2) showed no in vivo toxicity structurally as measured by optic nerve (ON) myelin thickness, functionally by ON-compound action potentials, on a cellular basis by oligodendrocyte precursor survival or changes in ON-myelin gene expression. PGJ(2) may be a clinically useful neuroprotective agent for ON and other CNS infarcts involving white matter, with mechanisms of action enabling effective treatment beyond the currently considered maximal time for intervention.
Rodent model of nonarteritic ischemic optic neuropathy and its electrophysiological evaluation
Our aim was to establish a rodent model of nonarteritic ischemic optic neuropathy (rNAION). To induce rNAION, after administration of Rose Bengal (RB) (2.5 mM), the small vessels of the left optic nerve were photoactivated using a 514-nm argon green laser with about 500-mu m spot size for 12 s (RB-laser induction). To evaluate the induction, funduscopic examination, fluorescein angiography (FA), visualization of capillaries within the optic disc, histologic evaluation, and electrophysiological testing were performed. In the RB-laser-induction eyes, the optic disc became swollen on day 3 followed by atrophy on week 8. FA showed filling defects in the choroid and optic disc at an early stage, followed by hyperfluorescence at a late stage. The capillaries within the optic disc were reduced markedly. Histopathologic examination showed acellular nerve fiber layer (NFL) swelling anterior to the optic disc. The morphologic retinal changes were apparent only in the retinal ganglion cell (RGC) layer, with a reduction in the number of cells. Visually evoked potential (VEP) amplitude decreased significantly, but electroretinography (ERG) showed no significant difference. The positive scotopic threshold response (pSTR) was not reduced on the 1st day but was significantly reduced 3 days after induction. The findings are similar to human NAION. Therefore, RB-laser induction is well suited to establish the presence of rNAION.
Neuroprotective effect on retinal ganglion cells by transpupillary laser irradiation of the optic nerve head
This study demonstrates that subthreshold transpupillary thermotherapy (TTT) laser irradiation on optic nerve head protects retinal ganglion cells (RGCs) in an optic nerve crush (ONC) model. TTT was performed in right eyes with an 810-nm diode laser aimed at the center of the optic nerve head, using the following protocol: power 60 mW, duration 60 s, spot size 500 m. Fluoro-Gold was injected into bilateral superior colliculi 5 days before sacrifice and fluorescent gold labeled RGCs were counted under fluorescence microscopy. In the ONC group, a progressive loss of RGCs was observed; however, in comparison with the ONC group, RGCs density was significantly higher ( P = 0.001, independent samples t-test) at day 7 postoperative and only borderline significances were obtained at days 14 and 28 postoperative ( P = 0.044 and P = 0.045, respectively, independent samples t-test) in ONC + TTT group, which implies the potential neuroprotective role of TTT. This protective effect seems to be heat shock proteins (HSPs) related, because intraperitoneal Quercetin (an inhibitor of HSPs, 4 mg/kg/day for 7 days) could completely abolish this protective effect at days 7, 14 and 28 postoperative ( P = 0.012, P = 0.002, and P = 0.000, respectively, independent samples t-test). Minimal collateral damage of TTT on optic nerve head tissue, peripapillary RGCs and the myelin sheath of the optic nerve were observed under transmission electron microscopy. These findings suggested that subthreshold TTT might be a safe and practical approach to protect RGCs. The underlying mechanisms may involve TTT-induced HSPs in RGCs.
Optic nerve inflammation and demyelination in a rodent model of nonarteritic anterior ischemic optic neuropathy
PURPOSE. Optic nerve (ON) ischemia associated with nonarteric anterior ischemic optic neuropathy (NAION) results in axon and myelin damage. Myelin damage activates the intraneural Ras homolog A (RhoA), contributing to axonal regeneration failure. We hypothesized that increasing extrinsic macrophage activity after ON infarct would scavenge degenerate myelin and improve postischemic ON recovery. We used the cytokine granulocyte-macrophage colony-stimulating factor (GM-CSF) to upregulate ON macrophage activity, and evaluated GM-CSF's effects after ON ischemia in the NAION rodent model (rAION).METHODS. Following rAION induction, GM-CSF was administered via intraventricular injection. Retinal ganglion cell (RGC) stereologic analysis was performed 1 month postinduction. The retinae and optic nerve laminae of vehicle-and GM-CSF-treated animals were examined immunohistochemically and ultrastructurally using transmission electron microscopy (TEM). RhoA activity was analyzed using a rhotekin affinity immunoanalysis and densitometry. Isolated ONs were analyzed functionally ex vivo by compound action potential (CAP) analysis.RESULTS. Rodent NAION produces ON postinfarct demyelination and myelin damage, functionally demonstrable by CAP analysis and ultrastructurally by TEM. Granulocyte-macrophage colony-stimulating factor increased intraneural inflammation, activating and recruiting endogenous microglia, with only a moderate amount of exogenous macrophage recruitment. Treatment with GM-CSF reduced postinfarct intraneural RhoA activity, but did not neuroprotect RGCs after rAION.CONCLUSIONS. Sudden ON ischemia results in previously unrecognized axonal demyelination, which may have a clinically important role in NAION-related functional defects and recovery. Granulocyte-macrophage colony-stimulating factor is not neuroprotective when administered directly to the optic nerve following ON ischemia, and does not improve axonal regeneration. It dramatically increases ON-microglial activation and recruitment.
Oligodendrocyte dysfunction after induction of experimental anterior optic nerve ischemia
Abstract PURPOSE: The early response and survival of oligodendrocytes after axonal stroke and their potential contribution to neuronal survival in vivo have not been adequately addressed. The purpose of this study was to investigate the changes occurring in the retina and optic nerve (ON) in anterior ischemic optic neuropathy (AION), using a c-fos transgenic mouse model. METHODS: A new mouse model of AION (rodent AION) was developed to evaluate the in vivo stress response of oligodendrocytes and retinal ganglion cells (RGCs) in a transgenic mouse strain, using the immediate early stress-response gene c-fos, RT-QPCR technology, immunohistochemistry, and electron microscopy. Confocal microscopy was used with cell-specific antibodies to characterize the timing of cells responding to rAION. The TUNEL assay detected cells undergoing apoptosis. Ultrastructural changes were analyzed by electron microscopy. RESULTS: In rAION, oligodendrocytes rapidly respond in vivo to ischemic ON damage, with c-fos activation as an early detectable event. Early evidence of progressive oligodendrocyte stress, is followed by demyelination, wallerian degeneration of the ON, and oligodendrocyte and RGC death far from the primary lesion. CONCLUSIONS: After rAION induction oligodendrocytes, as well as RGCs, undergo progressive stress, with dysfunction and apoptosis. The findings lead to a proposal that progressive retrograde oligodendrocyte stress, away from the primary lesion, is an important factor after ischemic optic neuropathy. Postinduction demyelination must be addressed for effective neuroprotection of ischemic and hypoxic white matter.
Effects of L-arginine on anatomical and electrophysiological deterioration of the eye in a rodent model of nonarteritic ischemic optic neuropathy
The aims of this study were to clarify the effectiveness of l-arginine (1) for reducing the severity of anatomical changes in the eye and improving visual function in the acute stage of a rodent model of nonarteritic ischemic optic neuropathy (rNAION) and (2) in preventing those changes in anatomy and visual function.For the first aim, l-arginine was intravenously injected into rats 3 h after rNAION induction; for the second aim, rNAION was induced after the oral administration of l-arginine for 7 days. The inner retinal thickness was determined over time by optical coherence tomography, and the amplitude of the scotopic threshold response (STR) and the number of surviving retinal ganglion cells (RGCs) were measured. These data were compared with the baseline data from the control group.Both intravenous infusion of l-arginine after rNAION induction and oral pretreatment with l-arginine significantly decreased optic disc edema in the acute stage and thinning of the inner retina, reduced the decrease in STR amplitude, and reduced the decrease in the number of RGCs during rNAION.Based on these results, we conclude that l-arginine treatment is effective for reducing anatomical changes in the eye and improving visual function in the acute stage of rNAION and that pretreatment with l-arginine is an effective therapy to reduce the severity of the condition during recurrence in the other eye.
Effects of steroid administration and transcorneal electrical stimulation on the anatomic and electrophysiologic deterioration of nonarteritic ischemic optic neuropathy in a rodent model
To elucidate the effectiveness of steroid administration and transcorneal electrical stimulation (TES) on anatomic changes and visual function in a rodent model of nonarteritic ischemic optic neuropathy (rNAION).Methylprednisolone (20 mg/kg) was injected through a central venous catheter twice a day for 3 days. TES was delivered with biphasic square pulses of 1 ms/phase, 100 mu A of current, and 20 Hz of frequency for 60 min 3 h after induction on the 1st, 4th, 7th, 14th, and 28th days.Intravenous infusion of methylprednisolone significantly decreased the degree of acute disc edema but did not preserve the inner retinal thinning, decreasing the amplitude of scotopic threshold responses (STR) and decreasing retinal ganglion cell (RGC) numbers in rNAION. TES preserved the decreasing STR amplitude and the decreasing RGC numbers in rNAION.Steroids are effective for reducing disc edema in the acute stage in rNAION. TES is effective for preserving decreasing RGC numbers and function in the chronic stage of rNAION.
Blood flow in the optic nerve head and factors that may influence it
In the recent past there has been great interest in the blood supply of the optic nerve head (ONH), how to evaluate ONH blood flow, and what factors influence it, in health and disease. This is because evidence has progressively accumulated that there is vascular insufficiency in the ONH in both anterior ischemic optic neuropathy (AION) and glaucomatous optic neuropathy (GON)-two major causes of blindness or of seriously impaired vision in man. For the management and prevention of visual loss in these two disorders, a proper understanding of the factors that influence the blood flow in the ONH is essential. The objective of this paper is, therefore, to review and discuss all these factors. The various factors that influence the vascular resistance, mean blood pressure and intraocular pressure are discussed, to create a better basic understanding of the ONH blood flow, which may help us toward a logical strategy for prevention and management of ischemic disorders of the ONH.
Pathogenesis of nonarteritic anterior ischemic optic neuropathy
Nonarteritic anterior ischemic optic neuropathy (NAION) is the most common clinical presentation of acute ischemic damage to the optic nerve. Most treatments proposed for NAION are empirical and include a wide range of agents presumed to act on thrombosis, on the blood vessels, or on the disk edema itself. Others are presumed to have a neuroprotective effect. Although there have been multiple therapies attempted, most have not been adequately studied, and animal models of NAION have only recently emerged. The Ischemic Optic Neuropathy Decompression Trial, the only class I large multicenter prospective treatment trial for nonarteritic anterior ischemic optic neuropathy, found no benefit from surgical intervention. One recent large, nonrandomized controlled study suggested that oral steroids might be helpful for acute NAION. Others recently proposed interventions are intravitreal injections of steroids or anti-vascular endothelial growth factor (anti-VEGF) agents. There are no class I studies showing benefit from either medical or surgical treatments. Most of the literature on the treatment of NAION consists of retrospective or prospective case series and anecdotal case reports. Similarly, therapies aimed at secondary prevention of fellow eye involvement in NAION remain of unproven benefit.
Temporal and spatial characteristics of RGC death and axon degeneration in the rat model of nonarteritic anterior ischemic optic neuropathy
Basal blood flow and autoregulation changes in the optic nerve of rhesus monkeys with idiopathic bilateral optic atrophy
PURPOSE. To characterize the hemodynamic features and the association with structural damage in the optic nerve head (ONH) of idiopathic bilateral optic atrophy (BOA) in rhesus macaque monkeys.METHODS. In five animals with BOA and nine healthy animals under general anesthesia (pentobarbital), intraocular pressure (IOP) was manometrically controlled. ONH blood flow was measured with a laser speckle flow graph device. Basal blood flow in global and quadrantal sectors was measured with IOP set at 10 mm Hg; autoregulation capacity was assessed by comparing blood flow changes before and after IOP was increased from 10 to 30 mm Hg. Spectral-domain optic coherence tomography was used to measure retinal nerve fiber layer thickness (RNFLT) by peripapillary circular scans.RESULTS. Compared with control eyes, RNFLT in BOA eyes was significantly less in all sectors (P CONCLUSIONS. Basal blood flow and autoregulation capacity in the ONH of BOA were significantly compromised, with a close correlation to structural changes. The hemodynamic changes showed no regional preference across the ONH, which was consistent with postmortem histological observations. (Invest Ophthalmol Vis Sci. 2013; 54: 714-721) DOI:10.1167/iovs.12-9773
Association between optic nerve blood flow and objective examinations in glaucoma patients with generalized enlargement disc type
Naoki Chiba, Kazuko Omodaka, Yu Yokoyama, Naoko Aizawa, Satoru Tsuda, Masayuki Yasuda, Takaaki Otomo, Shunji Yokokura, Nobuo Fuse, Toru Nakazawa Department of Ophthalmology, Tohoku University Graduate School of Medicine, Sendai, Japan Background: The purpose of this study was to investigate the correlations between microcirculation in the optic disc, average peripapillary retinal nerve fiber layer thickness cupping parameters, and visual field defects in glaucoma patients with the generalized enlargement disc type. Methods: A total of 38 eyes from 38 glaucoma patients with the generalized enlargement disc type were included. The microcirculation of the optic nerve head was examined with laser speckle flow graphy, and the mean blur rate in all areas, in vessel area, and in tissue area were calculated using the laser speckle flow graphy analyzer software. Average peripapillary retinal nerve fiber layer thickness was measured using Stratus optical coherence tomography, and cupping parameters were accessed using the Heidelberg retina tomograph. The mean deviation in the Humphrey field analyzer (30-2 SITA standard) was analyzed. The correlation between these parameters was evaluated using the Spearman rank correlation coefficient. Results: The correlation coefficient of mean blur rate in all optic disc area to the average peripapillary retinal nerve fiber layer thickness, vertical C/D, and mean deviation were r = 0.7546 (P amp;lt; 0.0001), r = amp;ndash;0.6208 (P amp;lt; 0.0001), and r = 0.6010 (P = 0.0001), respectively. The mean blur rate in tissue area of the optic disc showed r = 0.7305 (P amp;lt; 0.0001), r = amp;ndash;0.6438 (P amp;lt; 0.0001), and r = 0.6338 (P amp;lt; 0.0001). Conclusion: We found that the mean blur rate in the optic disc was significantly correlated with the average peripapillary retinal nerve fiber layer thickness, vertical C/D, and mean deviation in patients with the generalized enlargement disc type of glaucoma. In particular, the mean blur rate in tissue area was more highly correlated than the vessel area with other results of examination in glaucoma patients with the generalized enlargement disc type. Keywords: ocular blood flow, optic disc type, laser speckle flowgraphy, function, structure
Relationship among visual field, blood flow, and neural structure measurements in glaucoma
Abstract PURPOSE: To determine the relationship among visual field, neural structural, and blood flow measurements in glaucoma. METHODS: Case-control study. Forty-seven eyes of 42 patients with perimetric glaucoma were age-matched with 27 normal eyes of 27 patients. All patients underwent Doppler Fourier-domain optical coherence tomography to measure retinal blood flow and standard glaucoma evaluation with visual field testing and quantitative structural imaging. Linear regression analysis was performed to analyze the relationship among visual field, blood flow, and structure, after all variables were converted to logarithmic decibel scale. RESULTS: Retinal blood flow was reduced in glaucoma eyes compared to normal eyes (P < 0.001). Visual field loss was correlated with both reduced retinal blood flow and structural loss of rim area and retinal nerve fiber layer (RNFL). There was no correlation or paradoxical correlation between blood flow and structure. Multivariate regression analysis revealed that reduced blood flow and structural loss are independent predictors of visual field loss. Each dB decrease in blood flow was associated with at least 1.62 dB loss in mean deviation (P 0909¤ 0.001), whereas each dB decrease in rim area and RNFL was associated with 1.15 dB and 2.56 dB loss in mean deviation, respectively (P 0909¤ 0.03). CONCLUSIONS: There is a close link between reduced retinal blood flow and visual field loss in glaucoma that is largely independent of structural loss. Further studies are needed to elucidate the causes of the vascular dysfunction and potential avenues for therapeutic intervention. Blood flow measurement may be useful as an independent assessment of glaucoma severity.