Chinese Medical Sciences Journal ›› 2022, Vol. 37 ›› Issue (3): 181-194.doi: 10.24920/004118
1990-2030年全球和区域感染性心内膜炎的疾病负担及其归因危险因素的趋势和预测
林立金1,3,柳叶茂2,3,4,秦娟娟1,3,雷昉3,5,汪文鑫1,3,黄学伟1,3,刘伟芳3,5,张兴元3,5,折志刚1,3,张鹏3,5,张晓晶3,5,金朝霞2,4,*( ),李红良1,3,*(
),李红良1,3,*( )
)
- 1武汉大学人民医院心血管内科,武汉 430060,中国
2黄冈市中心医院心血管内科,黄冈 438000,中国
3武汉大学模式动物研究所,武汉 430071,中国
4黄冈市医学转化研究院,黄冈 438000,中国
5武汉大学基础医学院,武汉 430071,中国
-
收稿日期:2022-06-02接受日期:2022-08-30出版日期:2022-09-30发布日期:2022-09-26 -
通讯作者:金朝霞,李红良 E-mail:jinzhaoxia@hgyy.org.cn;lihl@whu.edu.cn
Global and Regional Trends and Projections of Infective Endocarditis-Associated Disease Burden and Attributable Risk Factors from 1990 to 2030
Lijin Lin1,3,Yemao Liu2,3,4,Juanjuan Qin1,3,Fang Lei3,5,Wenxin Wang1,3,Xuewei Huang1,3,Weifang Liu3,5,Xingyuan Zhang3,5,Zhigang She1,3,Peng Zhang3,5,Xiaojing Zhang3,5,Zhaoxia Jin2,4,*( ),Hongliang Li1,3,*(
),Hongliang Li1,3,*( )
)
- 1Department of Cardiology, Renmin Hospital of Wuhan University, Wuhan 430060, China
2Department of Cardiovascular, Huanggang Central Hospital, Huanggang, Hubei Province, 438021 China
3Institute of Model Animal, Wuhan University, Wuhan 430071, China
4Huanggang Institute of Translational Medicine, Huanggang, Hubei Province, 438802 China
5School of Basic Medical Science, Wuhan University, Wuhan 430071, China
-
Received:2022-06-02Accepted:2022-08-30Published:2022-09-30Online:2022-09-26 -
Contact:Zhaoxia Jin,Hongliang Li E-mail:jinzhaoxia@hgyy.org.cn;lihl@whu.edu.cn
摘要:
目的 预测感染性心内膜炎(Infective endocarditis,IE)未来的疾病负担及其归因危险因素。
方法 我们利用2019年全球疾病负担数据库分析了1990年至2019年IE的疾病负担及其危险因素,并利用贝叶斯年龄-时期-队列模型预测了2020年至2030年IE的全球疾病负担。
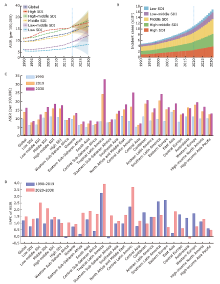
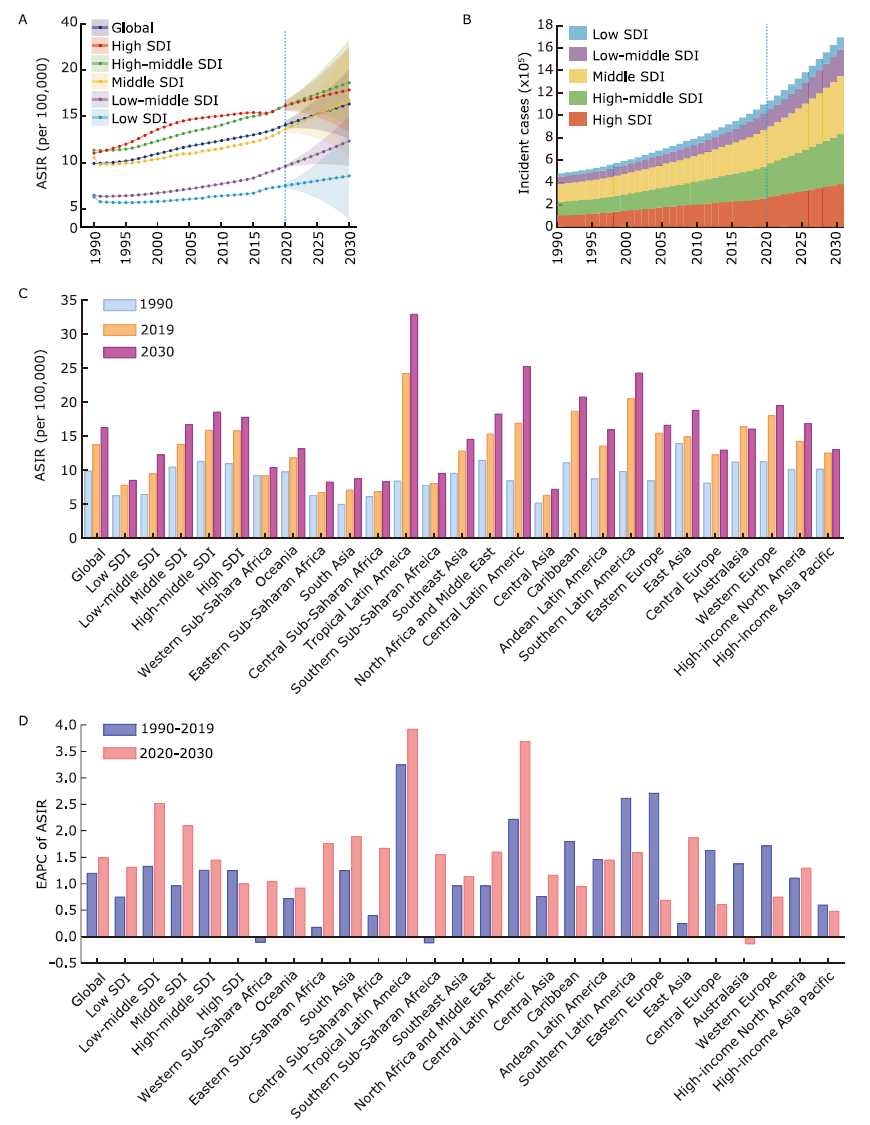
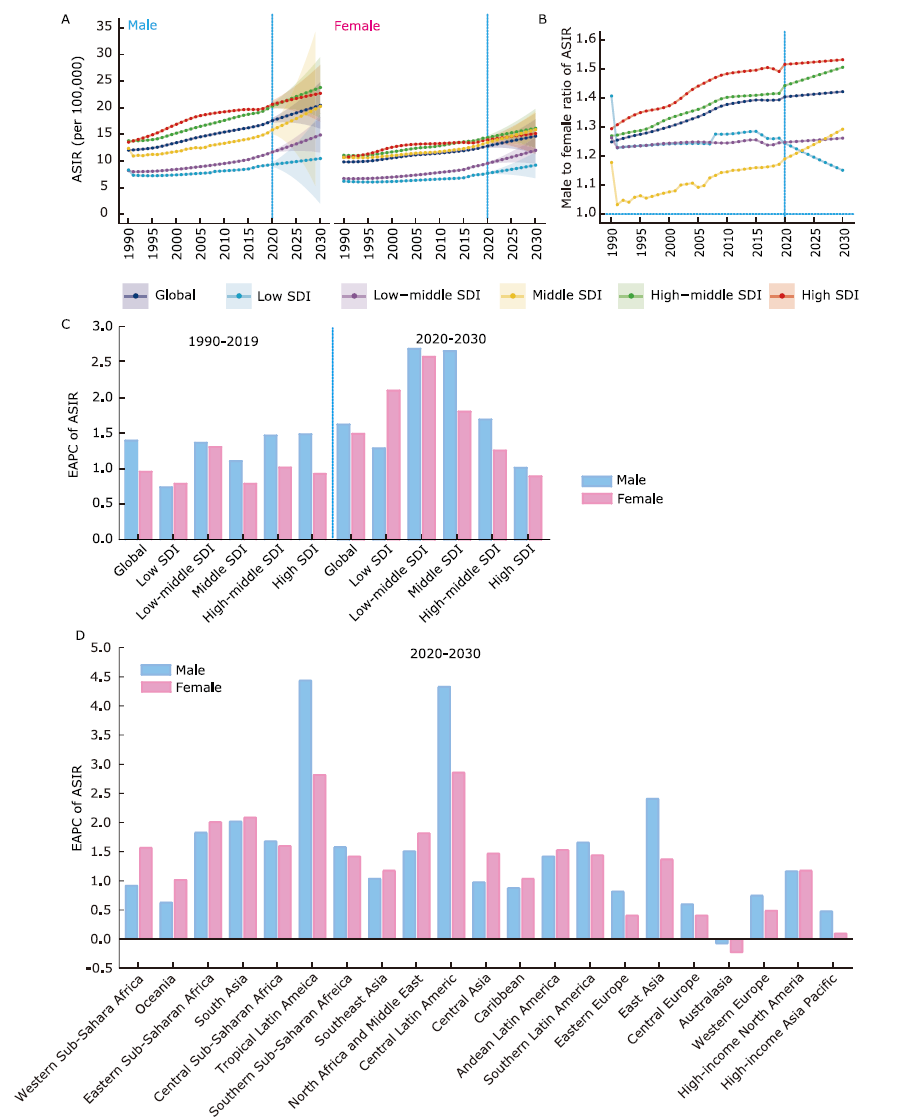
结果 到2030年,全球IE发病率将会不可控制地增加。其中,发展中国家的发病率增长速度最快,发达国家的新发病例数量最高,男性发病率较高,但性别差距将会缩小。高收入国家的老年人的发病负担最重,逐渐向中等收入国家转移。在中/高-中社会人口指数(social-demographic indicators,SDI)国家的发病率将超过高SDI国家。在中国,预计到2030年,IE的年龄标化发病率将达18.07/10万人,而IE患者的数量将达45万人。IE导致的死亡和心力衰竭负担仍然较重,女性的负担将增加并超过男性,而高SDI国家的老年人将承担最严重的疾病负担。高收缩压成为IE相关死亡的主要危险因素。
结论 未来十年全球范围内IE的疾病负担和危险因素分析表明,IE的发病率将会增加,IE相关的死亡和心衰负担的控制将成为严峻问题。应关注IE疾病负担的性别、年龄以及区域和国家的异质性,以便制定降低IE疾病负担的有效策略。
引用本文
Lijin Lin, Yemao Liu, Juanjuan Qin, Fang Lei, Wenxin Wang, Xuewei Huang, Weifang Liu, Xingyuan Zhang, Zhigang She, Peng Zhang, Xiaojing Zhang, Zhaoxia Jin, Hongliang Li. Global and Regional Trends and Projections of Infective Endocarditis-Associated Disease Burden and Attributable Risk Factors from 1990 to 2030[J].Chinese Medical Sciences Journal, 2022, 37(3): 181-194.
"
| Characteristics | Incidence | Death | Heart failure | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ASR per 105 in 2020 n (95% UI) | ASR per 105 in 2030 n (95% UI) | EAPC of ASR 2020 to 2030 n (95% CI) | ASR per 105 in 2020 n (95% UI) | ASR per 105 in 2030 n (95% UI) | EAPC of ASR 2020 to 2030 n (95% CI) | ASR per 105 in 2020 n (95% UI) | ASR per 105 in 2030 n (95% UI) | EAPC of ASR 2020 to 2030 n (95% CI) | |||
| Overall | |||||||||||
| Global | 14.07 (13.65, 14.48) | 16.33 (12.56, 20.10) | 1.50 (1.46, 1.54) | 0.88 (0.86, 0.91) | 0.83 (0.61, 1.06) | -0.58 (-0.59, -0.57) | 4.53 (4.45, 4.60) | 4.34 (3.59, 5.09) | -0.42 (-0.46, -0.37) | ||
| Sex | |||||||||||
| Male | 16.61 (16.15, 17.07) | 19.46 (15.09, 23.83) | 1.60 (1.56, 1.63) | 0.94 (0.92, 0.96) | 0.86 (0.65, 1.07) | -0.90 (-0.91, -0.88) | 4.21 (4.14, 4.29) | 4.07 (3.31, 4.83) | -0.34 (-0.38, -0.30) | ||
| Female | 11.82 (11.48, 12.17) | 13.68 (10.49, 16.88) | 1.47 (1.43, 1.51) | 0.79 (0.77, 0.82) | 0.74 (0.50, 0.99) | -0.62 (-0.63, -0.61) | 4.75 (4.67, 4.83) | 4.62 (3.77, 5.46) | -0.28 (-0.32, -0.24) | ||
| SDI | |||||||||||
| Low SDI | 7.51 (7.29, 7.74) | 8.56 (3.97, 13.14) | 1.31 (1.30, 1.32) | 0.79 (0.76, 0.82) | 0.80 (0.60, 1.00) | 0.10 (0.09, 0.11) | 2.01 (1.96, 2.07) | 2.07 (1.61, 2.52) | 0.27 (0.26, 0.28) | ||
| Low-middle SDI | 9.60 (9.45, 9.76) | 12.32 (9.61, 15.03) | 2.52 (2.50, 2.55) | 0.67 (0.65, 0.69) | 0.70 (0.52, 0.89) | 0.48 (0.47, 0.49) | 1.56 (1.52, 1.60) | 1.65 (1.32, 1.99) | 0.59 (0.57, 0.60) | ||
| Middle SDI | 13.59 (13.16, 14.03) | 16.72 (10.76, 22.68) | 2.10 (2.05, 2.14) | 0.61 (0.60, 0.63) | 0.58 (0.42, 0.74) | -0.49 (-0.51, -0.47) | 3.30 (3.24, 3.35) | 3.40 (2.82, 3.99) | 0.32 (0.30, 0.34) | ||
| High-middle SDI | 16.12 (15.63, 16.60) | 18.60 (14.06, 23.14) | 1.45 (1.40, 1.49) | 0.69 (0.67, 0.71) | 0.58 (0.43, 0.72) | -1.81 (-1.84, -1.78) | 3.10 (3.03, 3.16) | 3.15 (2.35, 3.95) | 0.16 (0.11, 0.21) | ||
| High SDI | 16.15 (15.56, 16.74) | 17.84 (13.30, 22.38) | 1.00 (0.96, 1.04) | 1.14 (1.10, 1.18) | 1.03 (0.43, 1.63) | -0.99 (-0.99, -0.99) | 8.52 (8.28, 8.76) | 7.97 (5.97, 9.96) | -0.67 (-0.69, -0.65) | ||
| Regions | |||||||||||
| Western Sub-Saharan Africa | 9.41 (9.19, 9.63) | 10.44 (7.74, 13.14) | 1.04 (1.04, 1.05) | 0.78 (0.74, 0.83) | 0.70 (0.38, 1.03) | -1.06 (-1.06, -1.06) | 2.51 (2.42, 2.60) | 2.57 (1.92, 3.21) | 0.22 (0.21, 0.22) | ||
| Oceania | 12.03 (11.35, 12.70) | 13.18 (9.07, 17.29) | 0.92 (0.91, 0.93) | 1.66 (1.44, 1.89) | 1.76 (0.89, 2.64) | 0.60 (0.60, 0.60) | 4.35 (3.86, 4.85) | 4.23 (2.40, 6.07) | -0.28 (-0.30, -0.25) | ||
| Eastern Sub-Saharan Africa | 6.96 (6.79, 7.14) | 8.29 (5.95, 10.63) | 1.76 (1.75, 1.77) | 0.90 (0.86, 0.95) | 0.87 (0.60, 1.14) | -0.33 (-0.35, -0.31) | 3.76 (3.64, 3.89) | 3.87 (2.92, 4.82) | 0.27 (0.27, 0.28) | ||
| South Asia | 7.28 (7.16, 7.41) | 8.78 (6.55, 11.01) | 1.89 (1.88, 1.90) | 0.64 (0.62, 0.66) | 0.68 (0.49, 0.87) | 0.57 (0.57, 0.57) | 1.31 (1.27, 1.34) | 1.34 (1.05, 1.62) | 0.23 (0.22, 0.23) | ||
| Central Sub-Saharan Africa | 7.06 (6.83, 7.29) | 8.33 (6.06, 10.60) | 1.67 (1.66, 1.67) | 1.00 (0.93, 1.07) | 0.99 (0.64, 1.33) | -0.08 (-0.09, -0.07) | 2.63 (2.48, 2.77) | 2.75 (1.92, 3.57) | 0.46 (0.46, 0.46) | ||
| Tropical Latin America | 22.45 (20.73, 24.18) | 32.97 (9.10, 56.84) | 3.92 (3.87, 3.97) | 1.05 (1.00, 1.09) | 0.93 (0.63, 1.23) | -1.15 (-1.19, -1.11) | 2.39 (2.31, 2.48) | 2.47 (1.87, 3.08) | 0.33 (0.30, 0.35) | ||
| Southern Sub-Saharan Africa | 8.21 (7.93, 8.49) | 9.58 (6.85, 12.30) | 1.55 (1.54, 1.55) | 0.78 (0.70, 0.86) | 0.73 (0.16, 1.30) | -0.72 (-0.74, -0.69) | 4.23 (4.04, 4.42) | 4.18 (3.03, 5.33) | -0.13 (-0.13, -0.12) | ||
| Southeast Asia | 13.04 (12.82, 13.25) | 14.60 (12.02, 17.18) | 1.14 (1.12, 1.16) | 1.28 (1.24, 1.32) | 1.26 (0.90, 1.63) | -0.16 (-0.18, -0.13) | 8.95 (8.78, 9.12) | 9.35 (7.65, 11.04) | 0.43 (0.40, 0.47) | ||
| North Africa and Middle East | 15.61 (15.37, 15.86) | 18.31 (14.76, 21.85) | 1.60 (1.60, 1.61) | 0.65 (0.62, 0.67) | 0.58 (0.42, 0.74) | -1.10 (-1.11, -1.09) | 2.29 (2.22, 2.36) | 2.25 (1.60, 2.91) | -0.17 (-0.19, -0.15) | ||
| Central Latin America | 17.60 (17.00, 18.19) | 25.29 (16.48, 34.10) | 3.69 (3.66, 3.72) | 0.54 (0.51, 0.57) | 0.53 (0.34, 0.72) | -0.21 (-0.22, -0.19) | 1.80 (1.73, 1.86) | 1.84 (1.38, 2.30) | 0.21 (0.20, 0.23) | ||
| Central Asia | 6.45 (6.24, 6.66) | 7.24 (5.41, 9.08) | 1.16 (1.15, 1.18) | 0.33 (0.30, 0.37) | 0.32 (0.17, 0.47) | -0.37 (-0.40, -0.34) | 0.31 (0.28, 0.35) | 0.30 (0.17, 0.42) | -0.57 (-0.57, -0.57) | ||
| Caribbean | 18.91 (18.39, 19.44) | 20.78 (15.88, 25.67) | 0.95 (0.93, 0.96) | 0.89 (0.82, 0.96) | 0.93 (0.59, 1.26) | 0.39 (0.39, 0.40) | 1.78 (1.67, 1.88) | 1.75 (1.20, 2.31) | -0.12 (-0.12, -0.12) | ||
| Andean Latin America | 13.84 (13.44, 14.25) | 15.99 (12.14, 19.84) | 1.45 (1.45, 1.46) | 0.57 (0.53, 0.62) | 0.51 (0.32, 0.71) | -1.09 (-1.10, -1.08) | 2.68 (2.54, 2.82) | 3.01 (2.09, 3.92) | 1.14 (1.10, 1.19) | ||
| Southern Latin America | 20.77 (20.25, 21.28) | 24.31 (18.65, 29.97) | 1.59 (1.57, 1.60) | 1.83 (1.73, 1.93) | 1.79 (1.08, 2.50) | -0.22 (-0.23, -0.21) | 6.50 (6.28, 6.72) | 6.72 (5.08, 8.36) | 0.34 (0.26, 0.42) | ||
| Eastern Europe | 15.55 (15.13, 15.98) | 16.66 (9.97, 23.34) | 0.69 (0.67, 0.71) | 0.78 (0.71, 0.84) | 0.70 (-0.06, 1.46) | -1.00 (-1.02, -0.97) | 0.77 (0.74, 0.81) | 0.75 (0.52, 0.97) | -0.38 (-0.39, -0.37) | ||
| East Asia | 15.65 (14.83, 16.47) | 18.82 (12.07, 25.57) | 1.87 (1.81, 1.92) | 0.28 (0.26, 0.29) | 0.24 (0.05, 0.42) | -1.56 (-1.58, -1.55) | 2.15 (2.10, 2.20) | 2.23 (1.78, 2.69) | 0.38 (0.35, 0.41) | ||
| Central Europe | 12.23 (11.92, 12.53) | 12.99 (9.63, 16.35) | 0.61 (0.57, 0.64) | 0.48 (0.45, 0.51) | 0.44 (0.27, 0.62) | -0.74 (-0.76, -0.71) | 1.16 (1.10, 1.22) | 1.11 (0.66, 1.56) | -0.42 (-0.43, -0.41) | ||
| Australasia | 16.31 (15.81, 16.81) | 16.09 (12.18, 20.00) | -0.14 (-0.15, -0.12) | 0.82 (0.75, 0.89) | 0.77 (0.44, 1.09) | -0.69 (-0.69, -0.68) | 7.97 (7.55, 8.39) | 8.00 (3.17, 12.83) | 0.03 (0.03, 0.04) | ||
| Western Europe | 18.15 (17.61, 18.68) | 19.55 (15.12, 23.98) | 0.75 (0.70, 0.79) | 1.25 (1.19, 1.30) | 1.04 (0.42, 1.65) | -1.83 (-1.85, -1.80) | 7.26 (7.12, 7.40) | 7.38 (5.84, 8.93) | 0.16 (0.16, 0.16) | ||
| High-income North America | 14.83 (13.95, 15.72) | 16.87 (10.86, 22.89) | 1.30 (1.26, 1.34) | 1.35 (1.26, 1.44) | 1.35 (-0.21, 2.92) | -0.01 (-0.02, -0.01) | 11.55 (10.95, 12.16) | 9.92 (5.73, 14.12) | -1.52 (-1.54, -1.50) | ||
| High-income Asia Pacific | 12.44 (11.95, 12.94) | 13.06 (9.42, 16.69) | 0.48 (0.44, 0.52) | 0.73 (0.69, 0.76) | 0.67 (0.29, 1.05) | -0.76 (-0.78, -0.74) | 6.93 (6.71, 7.16) | 6.56 (4.55, 8.58) | -0.54 (-0.55, -0.53) | ||
| 1. |
Baddour LM. Infective Endocarditis: Escalating Human and Health Care Burdens. Mayo Clin Proc 2020; 95(5):837-9. doi: 10.1016/j.mayocp.2020.03.022.
doi: S0025-6196(20)30311-6 pmid: 32370844 |
| 2. |
Habib G, Hoen B, Tornos P, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J 2009; 30(19):2369-413. doi: 10.1093/eurheartj/ehp285.
doi: 10.1093/eurheartj/ehp285 pmid: 19713420 |
| 3. |
Wang A, Gaca JG, Chu VH. Management Considerations in Infective Endocarditis: A Review. JAMA 2018; 320(1):72-83. doi: 10.1001/jama.2018.7596.
doi: 10.1001/jama.2018.7596 pmid: 29971402 |
| 4. |
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol 2020; 76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010.
doi: 10.1016/j.jacc.2020.11.010 pmid: 33309175 |
| 5. |
Yang X, Chen H, Zhang D, et al. Global magnitude and temporal trend of infective endocarditis, 1990-2019: results from the Global Burden of Disease Study. Eur J Prev Cardiol 2022; 29(8):1277-86. doi: 10.1093/eurjpc/zwab184.
doi: 10.1093/eurjpc/zwab184 |
| 6. |
Miro JM, Ambrosioni J. Infective endocarditis: an ongoing global challenge. Eur Heart J 2019; 40(39):3233-6. doi: 10.1093/eurheartj/ehz694.
doi: 10.1093/eurheartj/ehz694 pmid: 31589743 |
| 7. |
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
doi: 10.1016/S0140-6736(20)30925-9 pmid: 33069326 |
| 8. |
GBD 2019 Adolescent Young Adult Cancer Collaborators. The global burden of adolescent and young adult cancer in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Oncol 2021; 23(1):27-52. doi: 10.1016/S1470-2045(21)00581-7.
doi: 10.1016/S1470-2045(21)00581-7 pmid: 34871551 |
| 9. |
GBD 2019 Adolescent Mortality Collaborators. Global, regional, and national mortality among young people aged 10-24 years, 1950-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021; 398(10311):1593-618. doi: 10.1016/S0140-6736(21)01546-4.
doi: 10.1016/S0140-6736(21)01546-4 pmid: 34755628 |
| 10. |
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Disease and Injury Burden 1990-2019. Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME). 2020. doi: 10.6069/P5WM-5A36.
doi: 10.6069/P5WM-5A36 |
| 11. |
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Burden by Risk 1990-2019. Seattle, United States of America: Institute for Health Metrics and Evaluation (IHME). 2020. doi: 10.6069/630D-5V32.
doi: 10.6069/630D-5V32 |
| 12. |
Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36(44):3075-128. doi: 10.1093/eurheartj/ehv319.
doi: 10.1093/eurheartj/ehv319 |
| 13. |
Correction to: 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2016; 134(13):e298. doi: 10.1161/CIR.0000000000000460.
doi: 10.1161/CIR.0000000000000460 |
| 14. |
Mortality GBD, Causes of Death C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053):1459-544. doi: 10.1016/S0140-6736(16)31012-1.
doi: S0140-6736(16)31012-1 pmid: 27733281 |
| 15. |
Du Z, Chen W, Xia Q, et al. Trends and projections of kidney cancer incidence at the global and national levels, 1990-2030: a Bayesian age-period-cohort modeling study. Biomark Res 2020; 8:16. doi: 10.1186/s40364-020-00195-3.
doi: 10.1186/s40364-020-00195-3 pmid: 32435498 |
| 16. |
Yu J, Yang X, He W, et al. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019, and projections until 2039. Int J Cancer 2021; 149(5):993-1001. doi: 10.1002/ijc.33617.
doi: 10.1002/ijc.33617 pmid: 33937984 |
| 17. |
Liu W, Yang C, Chen Z, et al. Global death burden and attributable risk factors of peripheral artery disease by age, sex, SDI regions, and countries from 1990 to 2030: Results from the Global Burden of Disease study 2019. Atherosclerosis 2022; 347:17-27. doi: 10.1016/j.atherosclerosis.2022.03.002.
doi: 10.1016/j.atherosclerosis.2022.03.002 pmid: 35299057 |
| 18. |
Huang X, Wang Z, Shen Z, et al. Projection of global burden and risk factors for aortic aneurysm - timely warning for greater emphasis on managing blood pressure. Ann Med 2022; 54(1):553-64. doi: 10.1080/07853890.2022.2034932.
doi: 10.1080/07853890.2022.2034932 pmid: 35139697 |
| 19. |
Liu Z, Xu K, Jiang Y, et al. Global trend of aetiology-based primary liver cancer incidence from 1990 to 2030: a modelling study. Int J Epidemiol 2021; 50(1):128-42. doi: 10.1093/ije/dyaa196.
doi: 10.1093/ije/dyaa196 pmid: 33349860 |
| 20. |
Wang W, Hu M, Liu H, et al. Global Burden of Disease Study 2019 suggests that metabolic risk factors are the leading drivers of the burden of ischemic heart disease. Cell Metab 2021; 33(10):1943-56 e2. doi: 10.1016/j.cmet.2021.08.005.
doi: 10.1016/j.cmet.2021.08.005 pmid: 34478633 |
| 21. |
Pega F, Nafradi B, Momen NC, et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000-2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int 2021; 154:106595. doi: 10.1016/j.envint.2021.106595.
doi: 10.1016/j.envint.2021.106595 |
| 22. |
Sunil M, Hieu HQ, Arjan Singh RS, et al. Evolving trends in infective endocarditis in a developing country: a consequence of medical progress?. Ann Clin Microbiol Antimicrob 2019; 18(1):43. doi: 10.1186/s12941-019-0341-x.
doi: 10.1186/s12941-019-0341-x |
| 23. |
Mirabel M, Rattanavong S, Frichitthavong K, et al. Infective endocarditis in the Lao PDR: clinical characteristics and outcomes in a developing country. Int J Cardiol 2015; 180:270-3. doi: 10.1016/j.ijcard.2014.11.184.
doi: 10.1016/j.ijcard.2014.11.184 pmid: 25482077 |
| 24. |
Math RS, Sharma G, Kothari SS, et al. Prospective study of infective endocarditis from a developing country. Am Heart J 2011; 162(4):633-8. doi: 10.1016/j.ahj.2011.07.014.
doi: 10.1016/j.ahj.2011.07.014 pmid: 21982654 |
| 25. |
Sy RW, Kritharides L. Health care exposure and age in infective endocarditis: results of a contemporary population-based profile of 1536 patients in Australia. Eur Heart J 2010; 31(15):1890-7. doi: 10.1093/eurheartj/ehq110.
doi: 10.1093/eurheartj/ehq110 pmid: 20453066 |
| 26. |
Regueiro A, Linke A, Latib A, et al. Association Between Transcatheter Aortic Valve Replacement and Subsequent Infective Endocarditis and In-Hospital Death. JAMA 2016; 316(10):1083-92. doi: 10.1001/jama.2016.12347.
doi: 10.1001/jama.2016.12347 pmid: 27623462 |
| 27. |
Ostergaard L, Valeur N, Ihlemann N, et al. Incidence and factors associated with infective endocarditis in patients undergoing left-sided heart valve replacement. Eur Heart J 2018; 39(28):2668-75. doi: 10.1093/eurheartj/ehy153.
doi: 10.1093/eurheartj/ehy153 pmid: 29584858 |
| 28. |
Budea CM, Pricop M, Bratosin F, et al. Antibacterial and Antifungal Management in Relation to the Clinical Characteristics of Elderly Patients with Infective Endocarditis: A Retrospective Analysis. Antibiotics (Basel) 2022; 11(7). doi: 10.3390/antibiotics11070956.
doi: 10.3390/antibiotics11070956 |
| 29. |
Shah ASV, McAllister DA, Gallacher P, et al. Incidence, Microbiology, and Outcomes in Patients Hospitalized With Infective Endocarditis. Circulation 2020; 141(25):2067-77. doi: 10.1161/CIRCULATIONAHA.119.044913.
doi: 10.1161/CIRCULATIONAHA.119.044913 pmid: 32410460 |
| 30. |
Kuijpers JM, Koolbergen DR, Groenink M, et al. Incidence, risk factors, and predictors of infective endocarditis in adult congenital heart disease: focus on the use of prosthetic material. Eur Heart J 2017; 38(26):2048-56. doi: 10.1093/eurheartj/ehw591.
doi: 10.1093/eurheartj/ehw591 pmid: 28065906 |
| 31. |
Dilsizian V, Budde RPJ, Chen W, et al. Best Practices for Imaging Cardiac Device-Related Infections and Endocarditis: A JACC: Cardiovascular Imaging Expert Panel Statement. JACC Cardiovasc Imaging 2022; 15(5):891-911. doi: 10.1016/j.jcmg.2021.09.029.
doi: 10.1016/j.jcmg.2021.09.029 |
| 32. |
Lafrance JP, Rahme E, Lelorier J, et al. Vascular access-related infections: definitions, incidence rates, and risk factors. Am J Kidney Dis 2008; 52(5):982-93. doi: 10.1053/j.ajkd.2008.06.014.
doi: 10.1053/j.ajkd.2008.06.014 |
| 33. |
Chirillo F. New approach to managing infective endocarditis. Trends Cardiovasc Med 2021; 31(5):277-86. doi: 10.1016/j.tcm.2020.04.008.
doi: 10.1016/j.tcm.2020.04.008 |
| 34. |
Iung B, Duval X. Infective endocarditis: innovations in the management of an old disease. Nat Rev Cardiol 2019; 16(10):623-35. doi: 10.1038/s41569-019-0215-0.
doi: 10.1038/s41569-019-0215-0 pmid: 31175343 |
| 35. |
Ghanta RK, Pettersson GB. Surgical Treatment of Infective Endocarditis in Elderly Patients: The Importance of Shared Decision Making. J Am Heart Assoc 2021; 10(19): e022186; doi: 10.1161/JAHA.121.022186.
doi: 10.1161/JAHA.121.022186 |
| 36. |
Yang X, Chen H, Zhang D, et al. Global magnitude and temporal trend of infective endocarditis, 1990-2019: results from the Global Burden of Disease Study. Eur J Prev Cardiol 2022; 29(8):1277-86. doi: 10.1093/eurjpc/zwab184.
doi: 10.1093/eurjpc/zwab184 |
| 37. |
Mir T, Uddin M, Qureshi WT, et al. Predictors of Complications Secondary to Infective Endocarditis and Their Associated Outcomes: A Large Cohort Study from the National Emergency Database (2016-2018). Infect Dis Ther 2021. doi: 10.1007/s40121-021-00563-y.
doi: 10.1007/s40121-021-00563-y |
| 38. |
Tagliari AP, Steckert GV, da Silveira LMV, et al. Infective endocarditis profile, prognostic factors and in-hospital mortality: 6-year trends from a tertiary university center in South America. J Card Surg 2020; 35(8):1905-11. doi: 10.1111/jocs.14787.
doi: 10.1111/jocs.14787 pmid: 32598521 |
| 39. |
Bansal A, Cremer PC, Jaber WA, et al. Sex Differences in the Utilization and Outcomes of Cardiac Valve Replacement Surgery for Infective Endocarditis: Insights From the National Inpatient Sample. J Am Heart Assoc 2021; 10(20):e020095. doi: 10.1161/JAHA.120.020095.
doi: 10.1161/JAHA.120.020095 |
| 40. |
Smit J, Lopez-Cortes LE, Kaasch AJ, et al. Gender differences in the outcome of community-acquired Staphylococcus aureus bacteraemia: a historical population-based cohort study. Clin Microbiol Infect 2017; 23(1):27-32. doi: 10.1016/j.cmi.2016.06.002.
doi: 10.1016/j.cmi.2016.06.002 |
| 41. |
Lee GB, Shin KE, Han K, et al. Association Between Hypertension and Incident Infective Endocarditis. Hypertension 2022; 79(7):1466-74. doi: 10.1161/HYPERTENSIONAHA.122.19185.
doi: 10.1161/HYPERTENSIONAHA.122.19185 |
| 42. |
Toyoda N, Chikwe J, Itagaki S, et al. Trends in Infective Endocarditis in California and New York State, 1998-2013. JAMA 2017; 317(16):1652-60. doi: 10.1001/jama.2017.4287.
doi: 10.1001/jama.2017.4287 pmid: 28444279 |
| 43. |
Wu Z, Chen Y, Xiao T, et al. Epidemiology and risk factors of infective endocarditis in a tertiary hospital in China from 2007 to 2016. BMC Infect Dis 2020; 20(1):428. doi: 10.1186/s12879-020-05153-w.
doi: 10.1186/s12879-020-05153-w pmid: 32552765 |
| 44. |
Li HL, Tromp J, Teramoto K, et al. Temporal trends and patterns of infective endocarditis in a Chinese population: A territory-wide study in Hong Kong (2002-2019). Lancet Reg Health West Pac 2022; 22:100417. doi: 10.1016/j.lanwpc.2022.100417.
doi: 10.1016/j.lanwpc.2022.100417 |
| 45. |
Naegle MA. Theoretical perspectives on the etiology of substance abuse. Holist Nurs Pract 1988; 2(4):1-13. doi: 10.1097/00004650-198808000-00004.
doi: 10.1097/00004650-198808000-00004 pmid: 3403632 |
| 46. |
Sedrakyan A, Dhruva SS, Sun T, et al. Trends in Use of Transcatheter Aortic Valve Replacement by Age. JAMA 2018; 320(6):598-600. doi: 10.1001/jama.2018.9938.
doi: 10.1001/jama.2018.9938 pmid: 30039166 |
| 47. |
Eleyan L, Khan AA, Musollari G, et al. Infective endocarditis in paediatric population. Eur J Pediatr 2021; 180(10):3089-100. doi: 10.1007/s00431-021-04062-7.
doi: 10.1007/s00431-021-04062-7 |
| 48. |
Ren Z, Mo X, Chen H, et al. A changing profile of infective endocarditis at a tertiary hospital in China: a retrospective study from 2001 to 2018. BMC Infect Dis 2019; 19(1):945. doi: 10.1186/s12879-019-4609-8.
doi: 10.1186/s12879-019-4609-8 pmid: 31703633 |
| 49. |
Yang F, Zhang B, Yu J, et al. Epidemiology and the prognosis of healthcare-associated infective endocarditis in China: the significance of non-nosocomial acquisition. Emerg Microbes Infect 2015; 4(7):e38. doi: 10.1038/emi.2015.38.
doi: 10.1038/emi.2015.38 |
| 50. |
Lee JH, Kwak JG, Cho S, et al. Surgical outcomes of infective endocarditis in children: should we delay surgery for infective endocarditis?. Eur J Cardiothorac Surg 2021; 60(4):920-7. doi: 10.1093/ejcts/ezab149.
doi: 10.1093/ejcts/ezab149 pmid: 33842975 |
| [1] | 谷雨,张婷,彭敏,施举红. 显微镜下多血管炎患者继发弥漫性肺泡出血和肺间质病的临床特征及预后分析[J]. Chinese Medical Sciences Journal, 2022, 37(4): 293-302. |
| [2] | 王梓阳, 兰雨姗, 徐子犊, 顾耀文, 李姣. 基于机器学习的脓毒症死亡率预测模型对比研究[J]. Chinese Medical Sciences Journal, 2022, 37(3): 201-209. |
| [3] | 刘婕妤, 王嘉祥, 许力, 邓飞艳. 骨质疏松性骨折风险评估的潜在生物分子:一项综述回顾[J]. Chinese Medical Sciences Journal, 2021, 36(2): 135-149. |
| [4] | 吴斌,周江华,汪文鑫,杨慧琳,夏盟,张丙宏,折志刚,李红良. 高脂血症与新型冠状病毒肺炎住院患者28天全因死亡率的关系[J]. Chinese Medical Sciences Journal, 2021, 36(1): 17-26. |
| [5] | 李文省, 张彦丽. 用于膀胱癌预后预测的lncRNA分子标记物开发[J]. Chinese Medical Sciences Journal, 2020, 35(3): 239-247. |
| [6] | 朱卫华,谢文勇,张哲栋,李澍,张大方,刘以俊,朱继业,冷希圣. 59例肝门部胆管癌切除术后并发症和生存率分析[J]. Chinese Medical Sciences Journal, 2020, 35(2): 157-169. |
| [7] | 白冰, 田园, 张越伦, 马满娇, 虞雪融, 黄宇光. 后路脊柱手术隐性失血的预测[J]. Chinese Medical Sciences Journal, 2019, 34(1): 38-44. |
| [8] | 张荣强, 李凤英, 刘军礼, 刘美宁, 罗文瑞, 马婷, 马波, 张志刚. 构建预测陕西省咸阳市日本脑炎疫情的季节性时间序列模型[J]. Chinese Medical Sciences Journal, 2017, 32(3): 152-160. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
|