Chinese Medical Sciences Journal ›› 2022, Vol. 37 ›› Issue (3): 218-227.doi: 10.24920/004065
• Scientific Data Sharing and Reuse:Original Article • Previous Articles Next Articles
Association between Air Pollution and Type 2 Diabetes Mellitus in Developing Countries: A Systematic Review and Meta-Analysis
Zihan Chen1, Zhou Zhao1, 2, Chuiwen Deng3, Naishi Li1, *( )
)
- 1Department of Endocrinology, Key Laboratory of Endocrinology of National Health Commission, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, Beijing 100730, China
2Cadre Medical Department, Beijing Aerospace General Hospital, Beijing 100076, China
3Department of Rheumatology and Clinical Immunology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, the Ministry of Education Key Laboratory, Beijing 100730, China
-
Received:2022-01-20Accepted:2022-05-31Published:2022-09-30Online:2022-06-20 -
Contact:Naishi Li E-mail:lns@medmail.com.cn
Cite this article
Zihan Chen, Zhou Zhao, Chuiwen Deng, Naishi Li. Association between Air Pollution and Type 2 Diabetes Mellitus in Developing Countries: A Systematic Review and Meta-Analysis[J].Chinese Medical Sciences Journal, 2022, 37(3): 218-227.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
Table 1.
Characteristics of the included studies"
| Author and year | Study design | Location | Participants | Study period | Pollutants | Average exposure | Effect estimate (95% CI) | Outcomes | Definition of diabetes |
|---|---|---|---|---|---|---|---|---|---|
| Bo Y, et al(2021)[ | Cohort | Taiwan, China | 146,789 | 2001 - 2014 | PM2.5 | 27μg/m3 | 1.28 (1.19, 1.39) | T2DM incidence | Self-report of physician-diagnosed T2DM |
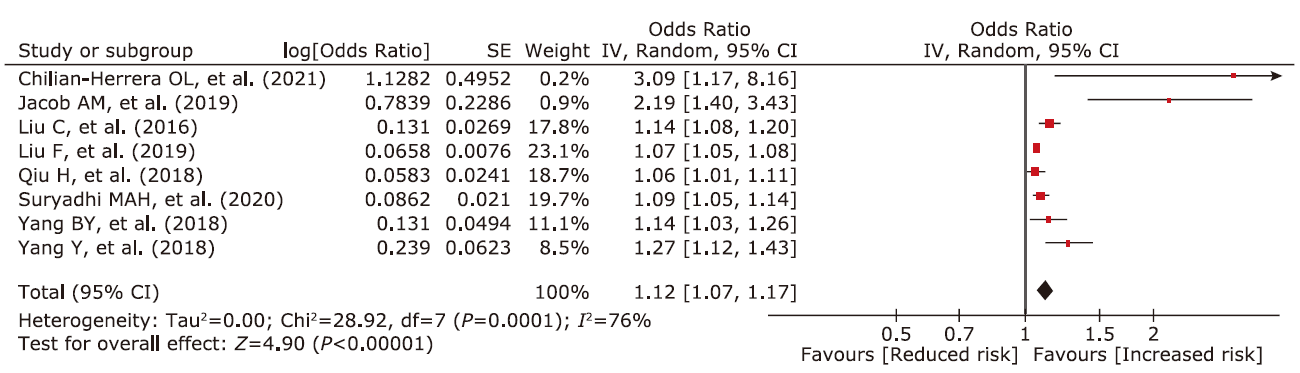
| Chilian-Herrera OL, et al (2021)[ | Cohort | Municipalities of the State of Mexico and Mexico City | 2,297 | 2006 - 2012 | PM2.5 | 24.8μg/m3 | 3.09 (1.17, 8.15) | DM prevalence | Self-report information of “having received a medical diagnosis of diabetes or high blood sugar” |
| Hassanvand MS, et al(2017)[ | Cross-sectional | 5 large cities in Iran | 2,916 | 2006 - 2011 | PM10 | 120.15μg/m3(study group), 83.95μg/m3(control group) | 1.32 (1.03, 1.69) | T2DM prevalence | Defined as a positive response to either of the following two questions: 1) “Have you ever been told by a doctor or other health worker that you have diabetes?”; 2) “Are you currently taking oral medication or insulin for diabetes prescribed by a doctor or other healthcare professional?” |
| Jabbari F, et al (2020)[ | Cohort | Municipal district 13 of Tehran, Iran | 2,428 | 2009 - 2011 | PM10 | 82.6μg/m3 | 1.50 (1, 2.32) | T2DM incidence | Defined as the concentration of FBG ≥ 126 mg/dL, non-FBG ≥ 200 mg/dL, and regular use of glucose-lowering medication |
| Jacob AM, et al (2019)[ | Cross-sectional | Chennai, Tamil Nadu, India | 410 | 2017 - 2018 | PM2.5 | 74.22μg/m3(study group) 27.22μg/m3 (control group) | 2.19 (1.40, 2.43) | T2DM prevalence | Meeting either of the following two criteria: 1) RCBG ≥ 140 mg/dl (7.8 mmol/l); 2) RCBG >200 mg/ dl (11.1 mmol/l) and reporting any one of the classic symptoms or weight loss |
| Liu C, et al(2016)[ | Cross-sectional | 150 counties or districts from 28 provinces, China | 11,847 | 2011 - 2012 | PM2.5 | 72.6μg/m3 | 1.14 (1.08, 1.20) | T2DM prevalence | Self-reported diabetes, and/or FBG ≥7 mmol/L, and/or HbA1c ≥ 6.5%, and/or insulin use according to ADA’s recommendation |
| Liu F, et al (2019)[ | Cohort | Rural areas of Henan province, China | 39,259 | 2015 - 2017 | PM1 | 57.4μg/m3 | 1.040 (1.026, 1.054) | T2DM prevalence | Previously diagnosed with T2DM and currently using antidiabetic medicines and/or FBG ≥ 7.0 mmol/L |
| PM2.5 | 73.4μg/m3 | 1.068 (1.052, 1.084) | |||||||
| NO2 | 39.9μg/m3 | 1.050 (1.039, 1.061) | |||||||
| Li CY, et al(2019)[ | Cohort | Taiwan, China | 505,151 | 2001 - 2012 | PM2.5 | 27.28μg/m3 | 1.08 (1.06, 1.10) | T2DM incidence | Based on ICD-9 |
| Li YL, et al(2021)[ | Cohort | Taiwan, China | 6,426,802 | 2005 - 2010 | O3 | 26.21ppb | 1.058 (1.053, 1.064) | T2DM incidence | Based on ICD-9 |
| SO2 | 4.77ppb | 1.011 (1.007, 1.015) | |||||||
| Qiu H, et al(2018)[ | Cohort | Hong Kong, China | 61,447 | 1998 - 2001 | PM2.5 | 35.8μg/m3 | 1.06 (1.01, 1.11) | T2DM prevalence | Based on ICD-9 |
| 1.15 (1.05, 1.25) | T2DM incidence | ||||||||
| Shan A, et al (2020)[ | Cohort | Four cities in northern China | 38,529 | 1998 - 2009 | PM10 | 143.36μg/m3 | 1.831 (1.778, 1.886) | T2DM incidence | Self-reported physician diagnosis (from at least a class three hospital), intake of antidiabetic drugs or injection of insulin simultaneously |
| SO2 | 66.71μg/m3 | 1.287 (1.256, 1.318) | |||||||
| NO2 | 40.74μg/m3 | 1.472 (1.419, 1.528) | |||||||
| Suryadhi MAH, et al(2020)[ | Cross-sectional | 487 regencies/ municipalities in all 33 provinces in Indonesia | 647,947 | 2007 - 2013 | PM2.5 | 8.3μg/m3 | 1.09 (1.05, 1.14) | DM prevalence | Using the following question “Have you ever been diagnosed with diabetes mellitus by a doctor?” |
| Wang M, et al (2020)[ | Cross-sectional | Jinchang city, Gansu province, China | 19,884 | 2011 - 2013 | PM10 | 109.43μg/m3 | 1.17 (1.08, 1.26) | DM incidence | Defined according to the diagnostic criteria recommended by ADA as FBG ≥ 7.0 mmol/L and/or self-report clinical diagnosed of diabetes and/or self-report used of anti-diabetes drugs |
| Yang BY, et al (2018)[ | Cross-sectional | Liaoning province, China | 15,477 | 2009 | PM1 | 66.0μg/m3 | 1.13 (1.04, 1.22) | DM prevalence | Defined according to ADA’s recommendations, as FBG ≥ 7.0 mmol/L or 2 h glucose ≥ 11.1mmol/L, or intake of any antidiabetic medication (both insulin and oral antidiabetic drugs), or both |
| PM2.5 | 82.0μg/m3 | 1.14 (1.03, 1.25) | |||||||
| PM10 | 123.1μg/m3 | 1.20 (1.12, 1.28) | |||||||
| SO2 | 54.4μg/m3 | 1.12 (1.04, 1.21) | |||||||
| NO2 | 35.3μg/m3 | 1.22 (1.12, 1.33) | |||||||
| O3 | 49.4μg/m3 | 1.14 (1.05, 1.25) | |||||||
| Yang Y, et al (2018)[ | Cross-sectional | 8 provinces across China | 11,504 | 2007 - 2010 | PM2.5 | 46.97μg/m3 | 1.27 (1.12, 1.43) | DM prevalence | Self-reported information using the following three criteria: 1) diagnosed with diabetes mellitus by a health care professional; 2) taking insulin or other medical treatments to reduce blood glucose levels during the last 12 months before the survey; 3) consuming a special diet and physical exercise regimen related to diabetes as recommended by medical professionals |
| Zhang Q, et al (2021)[ | Cross-sectional | 150 counties or districts from 28 provinces, China | 13,013 | 2011 - 2012 | NO2 | 24μg/m3 | 1.13 (1.01, 1.26) | DM prevalence | Primary definition of diabetes meeting at least one of the following criteria: FBG >126 mg/dl, a non-FBG >200 mg/dl, HbA1c > 6.5%, or using antidiabetic medications; self-reported diabetes defined as answering “Yes” to the question “Have you been diagnosed with diabetes or high blood sugar?” |
Table 2.
Assessment of the quality of the enrolled studies on air pollutant and diabetes mellitus"
| Study and year | Selection | Comparability | Exposure | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 | ||||
| Cross-sectional studies | |||||||||||
| Hassanvand MS, et al. (2017) | * | * | * | * | * | * | 6 | ||||
| Jacob AM, et al. (2019) | * | * | * | * | * | 5 | |||||
| Liu C, et al. (2016) | * | * | * | * | ** | * | * | 8 | |||
| Suryadhi MAH, et al. (2020) | * | * | * | * | ** | * | * | 7 | |||
| Wang M, et al. (2020) | * | * | * | * | ** | * | * | 8 | |||
| Yang BY, et al. (2018) | * | * | * | * | ** | * | * | * | 9 | ||
| Yang Y, et al. (2018) | * | * | * | * | ** | * | 7 | ||||
| Zhang Q, et al. (2021) | * | * | * | * | ** | * | * | 8 | |||
| Cohort Studies | |||||||||||
| Bo Y, et al. (2021) | * | * | * | ** | ** | * | * | 9 | |||
| Chilian-Herrera OL, et al. (2021) | * | * | * | ** | * | * | 7 | ||||
| Jabbari F, et al. (2020) | * | * | * | * | ** | * | * | 8 | |||
| Liu F, et al. (2019) | * | * | * | * | ** | * | * | 8 | |||
| Li CY, et al. (2019) | * | * | * | ** | * | * | * | 8 | |||
| Li YL, et al. (2021) | * | * | * | ** | * | * | * | 8 | |||
| Qiu H, et al. (2018) | * | * | * | * | ** | ** | * | * | 10 | ||
| Shan A, et al. (2020) | * | * | * | ** | * | * | * | 8 | |||
| 1. |
Chen B, Kan H. Air pollution and population health: A global challenge. Environ Health Prev Med 2008; 13(2):94-101. doi: 10.1007/s12199-007-0018-5.
doi: 10.1007/s12199-007-0018-5 |
| 2. |
Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012; 380(9859): 2224-60. doi: 10.1016/S0140-6736(12)61766-8.
doi: 10.1016/S0140-6736(12)61766-8 pmid: 23245609 |
| 3. |
Raaschou-Nielsen O, Andersen ZJ, Beelen R, et al. Air pollution and lung cancer incidence in 17 european cohorts: Prospective analyses from the european study of cohorts for air pollution effects (escape). Lancet Oncol. 2013; 14(9): 813-22. doi: 10.1016/S1470-2045(13)70279-1.
doi: 10.1016/S1470-2045(13)70279-1 pmid: 23849838 |
| 4. |
Beelen R, Raaschou-Nielsen O, Stafoggia M, et al. Effects of long-term exposure to air pollution on natural-cause mortality: An analysis of 22 european cohorts within the multicentre escape project. Lancet 2014; 383(9919): 785-95. doi: 10.1016/S0140-6736(13)62158-3.
doi: 10.1016/S0140-6736(13)62158-3 pmid: 24332274 |
| 5. |
Shah AS, Langrish JP, Nair H, et al. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet 2013; 382(9897): 1039-48. doi: 10.1016/S0140-6736(13)60898-3.
doi: 10.1016/S0140-6736(13)60898-3 pmid: 23849322 |
| 6. |
Cesaroni G, Forastiere F, Stafoggia M, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 european cohorts from the escape project. BMJ 2014; 348: f7412. doi: 10.1136/bmj.f7412.
doi: 10.1136/bmj.f7412 |
| 7. |
Mustafic H, Jabre P, Caussin C, et al. Main air pollutants and myocardial infarction: A systematic review and meta-analysis. JAMA 2012; 307(7): 713-21. doi: 10.1001/jama.2012.126.
doi: 10.1001/jama.2012.126 pmid: 22337682 |
| 8. |
Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in chinese adults. JAMA 2013; 310(9): 948-59. doi: 10.1001/jama.2013.168118.
doi: 10.1001/jama.2013.168118 pmid: 24002281 |
| 9. |
Misra A, Gopalan H, Jayawardena R, et al. Diabetes in developing countries. J Diabetes 2019; 11(7): 522-39. doi: 10.1111/1753-0407.12913.
doi: 10.1111/1753-0407.12913 pmid: 30864190 |
| 10. |
Polonsky KS. The past 200 years in diabetes. N Engl J Med 2012; 367(14): 1332-40. doi: 10.1056/NEJMra1110560.
doi: 10.1056/NEJMra1110560 |
| 11. |
Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: From pathophysiology to prevention and management. Lancet 2011; 378(9786): 169-81. doi: 10.1016/S0140-6736(11)60614-4.
doi: 10.1016/S0140-6736(11)60614-4 pmid: 21705072 |
| 12. |
Esposito K, Petrizzo M, Maiorino MI, et al. Particulate matter pollutants and risk of type 2 diabetes: A time for concern? Endocrine 2016; 51(1): 32-7. doi: 10.1007/s12020-015-0638-2.
doi: 10.1007/s12020-015-0638-2 pmid: 26024974 |
| 13. |
Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: Mechanistic insights. Diabetes 2012; 61(12): 3037-45. doi: 10.2337/db12-0190.
doi: 10.2337/db12-0190 pmid: 23172950 |
| 14. |
Hotamisligil GS. Inflammation and metabolic disorders. Nature 2006; 444(7121): 860-7. doi: 10.1038/nature05485.
doi: 10.1038/nature05485 |
| 15. |
Pope CA, 3rd, Turner MC, Burnett RT, et al. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ Res 2015; 116(1): 108-15. doi: 10.1161/CIRCRESAHA.116.305060.
doi: 10.1161/CIRCRESAHA.116.305060 pmid: 25348167 |
| 16. |
Haberzettl P, O’Toole TE, Bhatnagar A, et al. Exposure to fine particulate air pollution causes vascular insulin resistance by inducing pulmonary oxidative stress. Environ Health Perspect 2016; 124(12): 1830-9. doi: 10.1289/EHP212.
doi: 10.1289/EHP212 |
| 17. |
Liu C, Ying Z, Harkema J, et al. Epidemiological and experimental links between air pollution and type 2 diabetes. Toxicol Pathol 2013; 41(2): 361-73. doi: 10.1177/0192623312464531.
doi: 10.1177/0192623312464531 pmid: 23104765 |
| 18. |
Sun Q, Yue P, Deiuliis JA, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 2009; 119(4): 538-46. doi: 10.1161/CIRCULATIONAHA.108.799015.
doi: 10.1161/CIRCULATIONAHA.108.799015 pmid: 19153269 |
| 19. |
Cho CC, Hsieh WY, Tsai CH, et al. In vitro and in vivo experimental studies of PM2.5 on disease progression. Int J Environ Res Public Health 2018; 15(7): 1380. doi: 10.3390/ijerph15071380.
doi: 10.3390/ijerph15071380 |
| 20. |
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories,1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020; 396(10258): 1204-22. doi: 10.1016/S0140-6736(20)30925-9.
doi: 10.1016/S0140-6736(20)30925-9 |
| 21. |
Zanobetti A, Schwartz J. Are diabetics more susceptible to the health effects of airborne particles? Am J Respir Crit Care Med 2001; 164(5): 831-3. doi: 10.1164/ajrccm.164.5.2012039.
doi: 10.1164/ajrccm.164.5.2012039 |
| 22. |
O’Neill MS, Veves A, Zanobetti A, et al. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation 2005; 111(22): 2913-20. doi: 10.1161/CIRCULATIONAHA.104.517110.
doi: 10.1161/CIRCULATIONAHA.104.517110 pmid: 15927967 |
| 23. |
Whitsel EA, Quibrera PM, Christ SL, et al. Heart rate variability, ambient particulate matter air pollution, and glucose homeostasis: The environmental epidemiology of arrhythmogenesis in the women’s health initiative. Am J Epidemiol 2009; 169(6): 693-703. doi: 10.1093/aje/kwn400.
doi: 10.1093/aje/kwn400 pmid: 19208727 |
| 24. |
Balti EV, Echouffo-Tcheugui JB, Yako YY, et al. Air pollution and risk of type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res Clin Pract 2014; 106(2): 161-72. doi: 10.1016/j.diabres.2014.08.010.
doi: 10.1016/j.diabres.2014.08.010 |
| 25. |
Eze IC, Hemkens LG, Bucher HC, et al. Association between ambient air pollution and diabetes mellitus in europe and north america: Systematic review and meta-analysis. Environ Health Perspect 2015; 123(5): 381-9. doi: 10.1289/ehp.1307823.
doi: 10.1289/ehp.1307823 |
| 26. |
He D, Wu S, Zhao H, et al. Association between particulate matter 2.5 and diabetes mellitus: A meta-analysis of cohort studies. J Diabetes Investig 2017; 8(5): 687-96. doi: 10.1111/jdi.12631.
doi: 10.1111/jdi.12631 |
| 27. |
Liu F, Chen G, Huo W, et al. Associations between long-term exposure to ambient air pollution and risk of type 2 diabetes mellitus: A systematic review and meta-analysis. Environ Pollut 2019; 252(Pt B): 1235-45. doi: 10.1016/j.envpol.2019.06.033.
doi: S0269-7491(19)30257-X pmid: 31252121 |
| 28. |
Yang BY, Fan S, Thiering E, et al. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environ Res 2020; 180: 108817. doi: 10.1016/j.envres.2019.108817.
doi: 10.1016/j.envres.2019.108817 |
| 29. |
Krutmann J, Liu W, Li L, et al. Pollution and skin: From epidemiological and mechanistic studies to clinical implications. J Dermatol Sci 2014; 76(3): 163-8. doi: 10.1016/j.jdermsci.2014.08.008.
doi: 10.1016/j.jdermsci.2014.08.008 pmid: 25278222 |
| 30. |
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories,1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018; 392(10159): 1923-94. doi: 10.1016/S0140-6736(18)32225-6.
doi: 10.1016/S0140-6736(18)32225-6 |
| 31. |
NCD-RisC NRFC. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016; 387(10027): 1513-30. doi: 10.1016/s0140-6736(16)00618-8.
doi: S0140-6736(16)00618-8 pmid: 27061677 |
| 32. | Methods guide for effectiveness and comparative effectiveness reviews. AHRQ methods for effective health care. Rockville (MD) 2008. |
| 33. |
Stang A. Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25(9): 603-5. doi: 10.1007/s10654-010-9491-z.
doi: 10.1007/s10654-010-9491-z pmid: 20652370 |
| 34. |
Bo Y, Chang LY, Guo C, Lin C, et al. Associations of reduced ambient PM2.5 level with lower plasma glucose concentration and decreased risk of type 2 diabetes in adults: A longitudinal cohort study. Am J Epidemiol 2021; 190(10): 2148-57. doi: 10.1093/aje/kwab159.
doi: 10.1093/aje/kwab159 |
| 35. |
Chilian-Herrera OL, Tamayo-Ortiz M, Texcalac-Sangrador JL, et al. PM2.5 exposure as a risk factor for type 2 diabetes mellitus in the mexico city metropolitan area. BMC public health. 2021; 21(1): 2087. doi: 10.1186/s12889-021-12112-w.
doi: 10.1186/s12889-021-12112-w |
| 36. |
Hassanvand MS, Naddafi K, Malek M, et al. Effect of long-term exposure to ambient particulate matter on prevalence of type 2 diabetes and hypertension in iranian adults: An ecologic study. Environ Sci Pollut Res Int 2018; 25(2): 1713-8. doi: 10.1007/s11356-017-0561-6.
doi: 10.1007/s11356-017-0561-6 |
| 37. |
Jabbari F, Mohseni Bandpei A, Daneshpour MS, et al. Role of air pollution and rs 10830963 polymorphism on the incidence of type 2 diabetes: Tehran cardiometabolic genetic study. J Diabetes Res 2020; 2020: 2928618. doi: 10.1155/2020/2928618.
doi: 10.1155/2020/2928618 |
| 38. |
Jacob AM, Datta M, Kumpatla S, et al. Prevalence of diabetes mellitus and exposure to suspended particulate matter. J Health Pollut 2019; 9(22): 190608. doi: 10.5696/2156-9614-9.22.190608.
doi: 10.5696/2156-9614-9.22.190608 |
| 39. |
Liu C, Yang C, Zhao Y, et al. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in china. Environ Int 2016; 92-93: 416-21. doi: 10.1016/j.envint.2016.03.028.
doi: 10.1016/j.envint.2016.03.028 pmid: 27148900 |
| 40. |
Liu F, Guo Y, Liu Y, et al. Associations of long-term exposure to PM1, PM2.5, NO2 with type 2 diabetes mellitus prevalence and fasting blood glucose levels in chinese rural populations. Environ Int 2019; 133(Pt B): 105213. doi: 10.1016/j.envint.2019.105213.
doi: 10.1016/j.envint.2019.105213 |
| 41. |
Li CY, Wu CD, Pan WC, et al. Association between long-term exposure to PM2.5 and incidence of type 2 diabetes in taiwan: A national retrospective cohort study. Epidemiology (Cambridge, Mass) 2019; 30 Suppl 1: S67-s75. doi: 10.1097/ede.0000000000001035.
doi: 10.1097/ede |
| 42. |
Li YL, Chuang TW, Chang PY, et al. Long-term exposure to ozone and sulfur dioxide increases the incidence of type 2 diabetes mellitus among aged 30 to 50 adult population. Environ Res 2021; 194: 110624. doi: 10.1016/j.envres.2020.110624.
doi: 10.1016/j.envres.2020.110624 |
| 43. |
Qiu H, Schooling CM, Sun S, et al. Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: A cohort study in Hong Kong. Environ Int 2018; 113: 350-6. doi: 10.1016/j.envint.2018.01.008.
doi: S0160-4120(17)31891-3 pmid: 29357993 |
| 44. |
Shan A, Zhang Y, Zhang LW, et al. Associations between the incidence and mortality rates of type 2 diabetes mellitus and long-term exposure to ambient air pollution: A 12 -year cohort study in northern china. Environ Res. 2020; 186: 109551. doi: 10.1016/j.envres.2020.109551.
doi: 10.1016/j.envres.2020.109551 |
| 45. |
Suryadhi MAH, Suryadhi PAR, Abudureyimu K, et al. Exposure to particulate matter (PM2.5) and prevalence of diabetes mellitus in indonesia. Environ Int 2020; 140: 105603. doi: 10.1016/j.envint.2020.105603.
doi: 10.1016/j.envint.2020.105603 |
| 46. |
Wang M, Jin Y, Dai T, et al. Association between ambient particulate matter (PM10) and incidence of diabetes in northwest of china: A prospective cohort study. Ecotoxicol Environ Saf 2020; 202: 110880. doi: 10.1016/j.ecoenv.2020.110880.
doi: 10.1016/j.ecoenv.2020.110880 |
| 47. |
Yang BY, Qian ZM, Li S, et al. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: A cross-sectional study with findings from the 33 communities chinese health study. Lancet Planet Health 2018; 2(2): e64-e73. doi: 10.1016/S2542-5196(18)30001-9.
doi: 10.1016/S2542-5196(18)30001-9 |
| 48. |
Yang Y, Guo Y, Qian ZM, et al. Ambient fine particulate pollution associated with diabetes mellitus among the elderly aged 50 years and older in china. Environ Pollut 2018; 243(Pt B): 815-23. doi: 10.1016/j.envpol.2018.09.056.
doi: S0269-7491(18)30981-3 pmid: 30243190 |
| 49. |
Zhang Q, Liu C, Wang Y, et al. Associations of long-term exposure to ambient nitrogen dioxide with indicators of diabetes and dyslipidemia in China: A nationwide analysis. Chemosphere 2021; 269: 128724. doi: 10.1016/j.chemosphere.2020.128724.
doi: 10.1016/j.chemosphere.2020.128724 |
| 50. |
Leucht S, Kissling W, Davis JM. How to read and understand and use systematic reviews and meta-analyses. Acta Psychiatrica Scandinavica 2009; 119(6): 443-50. doi: 10.1111/j.1600-0447.2009.01388.x.
doi: 10.1111/j.1600-0447.2009.01388.x pmid: 19469725 |
| 51. |
Puett RC, Hart JE, Schwartz J, et al. Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect 2011; 119(3): 384-9. doi: 10.1289/ehp.1002344.
doi: 10.1289/ehp.1002344 |
| 52. |
Zheng Z, Xu X, Zhang X, et al. Exposure to ambient particulate matter induces a nash-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol. 2013; 58(1): 148-54. doi: 10.1016/j.jhep.2012.08.009.
doi: 10.1016/j.jhep.2012.08.009 pmid: 22902548 |
| 53. |
Elimam H, Abdulla AM, Taha IM. Inflammatory markers and control of type 2 diabetes mellitus. Diabetes Metab Syndr 2019; 13(1): 800-4. doi: 10.1016/j.dsx.2018.11.061.
doi: S1871-4021(18)30535-6 pmid: 30641811 |
| 54. |
Liu C, Wang B, Liu S, et al. Type 2 diabetes attributable to PM2.5: A global burden study from 1990 to 2019. Environ Int 2021; 156: 106725. doi: 10.1016/j.envint.2021.106725.
doi: 10.1016/j.envint.2021.106725 |
| 55. |
Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories,1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020; 396(10258): 1223-49. doi: 10.1016/S0140-6736(20)30752-2.
doi: 10.1016/S0140-6736(20)30752-2 |
| 56. |
Rawal LB, Tapp RJ, Williams ED, et al. Prevention of type 2 diabetes and its complications in developing countries: A review. Int J Behav Med 2012; 19(2): 121-33. doi: 10.1007/s12529-011-9162-9.
doi: 10.1007/s12529-011-9162-9 pmid: 21590464 |
| 57. |
Wiston M. Status of air pollution in botswana and significance to air quality and human health. J Health Pollut 2017; 7(15): 8-17. doi: 10.5696/2156-9614-7.15.
doi: 10.5696/2156-9614-7.15. |
| [1] | Kunrong Wu, Shufang Zhang, Ziwan Guan, Xiaoli Li, Rui Li, Ying Yin, Yan Li. Methylenetetrahydrofolate Reductase Gene Polymorphism C677T is Associated with Increased Risk of Coronary Heart Disease in Chinese Type 2 Diabetic Patients [J]. Chinese Medical Sciences Journal, 2021, 36(2): 103-109. |
| [2] | Yin Ying, Li Rui, Li Xiaoli, Wu Kunrong, Li Ling, Xu Yuedong, Liao Lin, Yang Rui, Li Yan. Association Between Homocysteine Level and Methylenetetrahydrofolate Reductase Gene Polymorphisms in Type 2 Diabetes Accompanied by Dyslipidemia [J]. Chinese Medical Sciences Journal, 2020, 35(1): 85-91. |
| [3] | Ping Fen, Cao Qin, Lin Hua, Han Shuzhi. Antagonistic Effects of N-acetylcysteine on Mitogen-activated Protein Kinase Pathway Activation, Oxidative Stress and Inflammatory Responses in Rats with PM2.5 Induced Lung Injuries [J]. Chinese Medical Sciences Journal, 2019, 34(4): 270-276. |
| [4] | Chen Zhiye, Zang Xiujuan, Liu Mengqi, Liu Mengyu, Li Jinfeng, Gu Zhaoyan, Ma Lin. Abnormal Alterations of Cortical Thickness in 16 Patients with Type 2 Diabetes Mellitus: A Pilot MRI Study△ [J]. Chinese Medical Sciences Journal, 2017, 32(2): 75-82. |
| [5] | Ying Fan, Shan-xiao Zhang, Meng Ren, Li-feng Hong, Xiao-ni Yan. Impact of 1, 25-(OH)2D3 on Left Ventricular Hypertrophy in Type 2 Diabetic Rats [J]. Chinese Medical Sciences Journal, 2015, 30(2): 114-120. |
| [6] | Yi-jun Zhou*,Ai Li, Yu-ling Song, Hui Zhou, Yan Li, Yin-si Tang. Role of Sclerostin in the Bone Loss of Postmenopausal Chinese Women with Type 2 Diabetes [J]. Chinese Medical Sciences Journal, 2013, 28(3): 135-139. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
|